How to Decrease Stroke Patient Arrival Time to Revascularization
advertisement
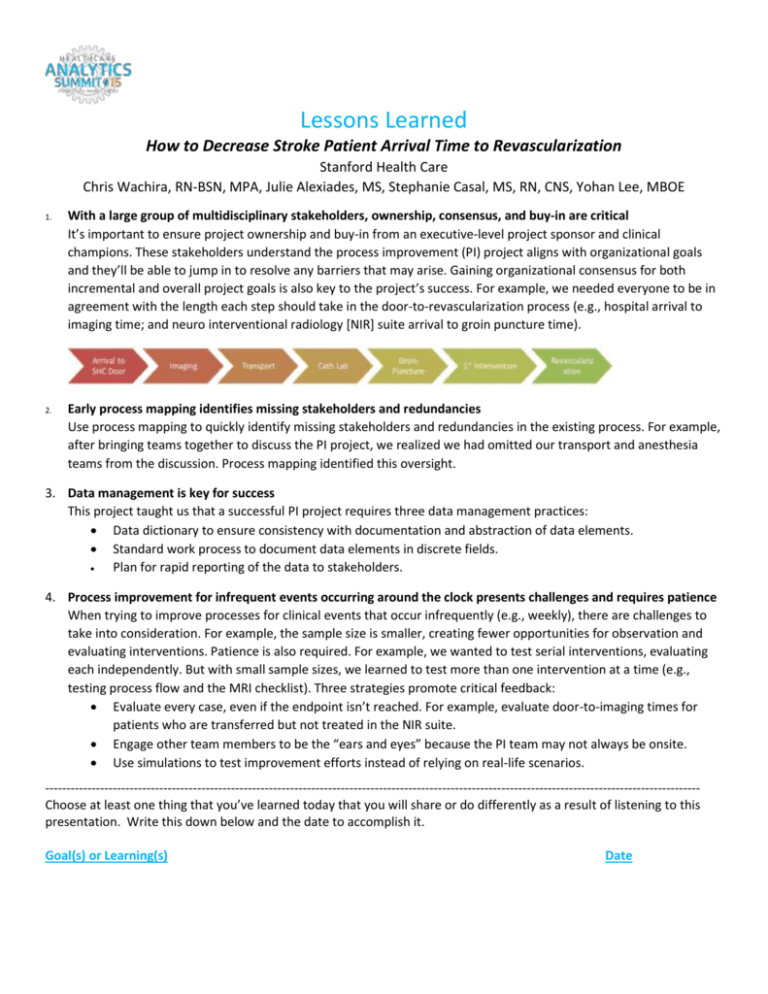
Lessons Learned How to Decrease Stroke Patient Arrival Time to Revascularization Stanford Health Care Chris Wachira, RN-BSN, MPA, Julie Alexiades, MS, Stephanie Casal, MS, RN, CNS, Yohan Lee, MBOE 1. With a large group of multidisciplinary stakeholders, ownership, consensus, and buy-in are critical It’s important to ensure project ownership and buy-in from an executive-level project sponsor and clinical champions. These stakeholders understand the process improvement (PI) project aligns with organizational goals and they’ll be able to jump in to resolve any barriers that may arise. Gaining organizational consensus for both incremental and overall project goals is also key to the project’s success. For example, we needed everyone to be in agreement with the length each step should take in the door-to-revascularization process (e.g., hospital arrival to imaging time; and neuro interventional radiology [NIR] suite arrival to groin puncture time). 2. Early process mapping identifies missing stakeholders and redundancies Use process mapping to quickly identify missing stakeholders and redundancies in the existing process. For example, after bringing teams together to discuss the PI project, we realized we had omitted our transport and anesthesia teams from the discussion. Process mapping identified this oversight. 3. Data management is key for success This project taught us that a successful PI project requires three data management practices: Data dictionary to ensure consistency with documentation and abstraction of data elements. Standard work process to document data elements in discrete fields. Plan for rapid reporting of the data to stakeholders. 4. Process improvement for infrequent events occurring around the clock presents challenges and requires patience When trying to improve processes for clinical events that occur infrequently (e.g., weekly), there are challenges to take into consideration. For example, the sample size is smaller, creating fewer opportunities for observation and evaluating interventions. Patience is also required. For example, we wanted to test serial interventions, evaluating each independently. But with small sample sizes, we learned to test more than one intervention at a time (e.g., testing process flow and the MRI checklist). Three strategies promote critical feedback: Evaluate every case, even if the endpoint isn’t reached. For example, evaluate door-to-imaging times for patients who are transferred but not treated in the NIR suite. Engage other team members to be the “ears and eyes” because the PI team may not always be onsite. Use simulations to test improvement efforts instead of relying on real-life scenarios. ----------------------------------------------------------------------------------------------------------------------------------------------------------Choose at least one thing that you’ve learned today that you will share or do differently as a result of listening to this presentation. Write this down below and the date to accomplish it. Goal(s) or Learning(s) Date