Read the SCOPE "Proof of Principle" Final Report here
advertisement
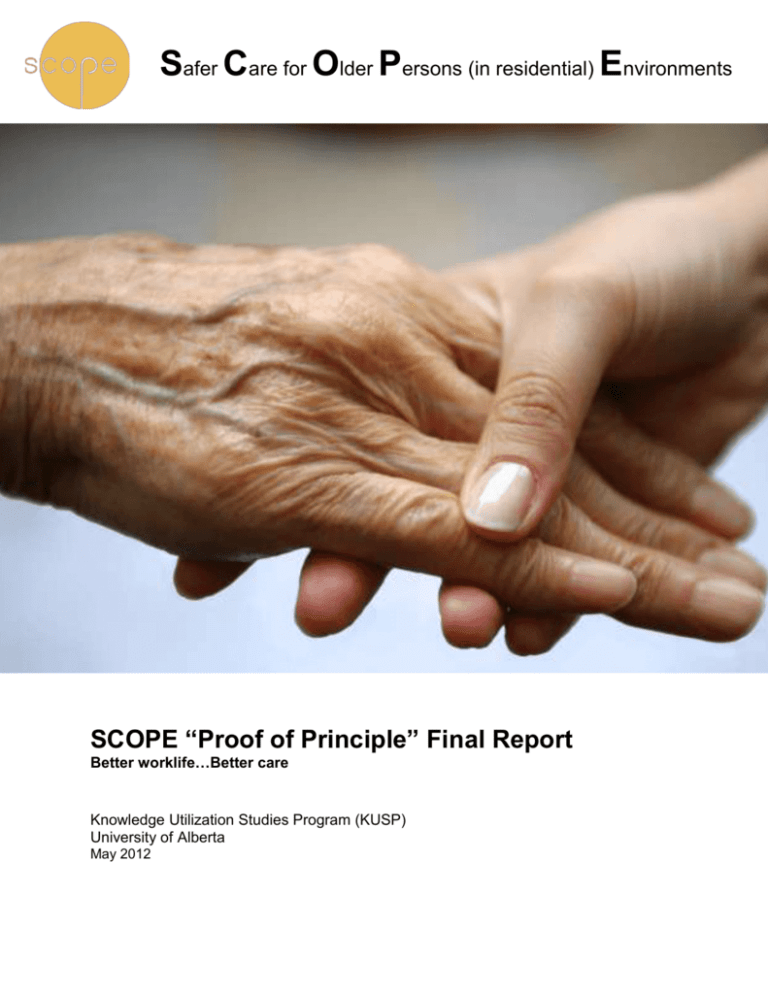
Safer Care for Older Persons (in residential) Environments SCOPE “Proof of Principle” Final Report Better worklife…Better care Knowledge Utilization Studies Program (KUSP) University of Alberta May 2012 Production of this final report has been made possible through a financial contribution from Health Canada. The views expressed herein do not necessarily represent the views of Health Canada. 2 |Page SCOPE Final Report, May 2012 Main Messages Increasing complexity of care required for nursing home residents and the often low value placed on their healthcare providers (primarily unregulated healthcare aides) contribute to poor quality of worklife for healthcare providers. This, in turn, can result in high rates of staff burnout and turnover, and less than optimal resident care. The Safer Care for Older Persons (in residential) Environments (SCOPE) study concluded that: Collaborative quality improvement (QI) can enhance the quality of worklife of healthcare providers in long-term care facilities. QI support can also improve the quality of care to nursing home residents. To be successful, this type of QI initiative requires a concerted team effort among frontline staff, managers, and administrators. Managerial support is key to QI team success. Facilitating an exchange of learning and care strategies among different nursing homes can expedite improvements in care and potentially decrease costs. Collaboration and support among provincial decision makers and various stakeholders are essential to widespread success. Decision makers and stakeholders should consider the value of collaborative QI initiatives in nursing homes as a means to: Improve recruitment and retention of healthcare providers, especially healthcare aides. Enhance the care of frail elderly residents. Use routinely collected data from the Resident Assessment Instrument – Minimum Data Set 2.0 to monitor the effects of QI activities on resident outcomes. SCOPE Final Report, May 2012 Page |3 Executive Summary Safer Care for Older Persons (in residential) Environments (SCOPE) was a two-year (20102012) pilot or proof of principle project conducted in seven nursing homes in Alberta and British Columbia. The overall goal of this project was to improve the quality of worklife for healthcare aides (HCAs) in nursing homes in Canada and to improve the safety and quality of care for frail elderly Canadians living in these nursing homes. Background Almost one-half of Canadians in long-term care (LTC) facilities are frail elderly over 80 years of age. Recent Canadian Institute for Health Information figures show that nation-wide in 2010/11, approximately 60% of LTC residents had a diagnosis of dementia. This growing number of nursing home residents with dementia has created job strain and job-related stress for healthcare providers, leading to reduced job satisfaction and high staff turnover. Healthcare providers’ quality of worklife in turn affects resident outcomes; for example, high staff turnover has been linked to poor resident outcomes, such as decreased functional ability and pressure ulcers. The SCOPE Project A 12-month collaborative quality improvement (QI) program was initiated in the participating nursing homes. Teams of three to five staff were led by a healthcare aide and supported by a senior sponsor. The teams selected one of three areas of care - behaviour management, pain management, or pressure ulcer (skin care) management - and used a process to improve care based on the Plan-Do-Study-Act model. Throughout the QI intervention, the teams were supported through learning sessions, getting-started kits, access to clinical and QI experts, coaching and change management techniques The effect of the QI program on the work setting (context) and resident outcomes was assessed using the SCOPE survey and the Resident Assessment Instrument – Minimum Data Set 2.0, respectively. QI process data were also analysed. Findings 1. The more successful QI teams showed greater team engagement, as well as stronger senior leadership and support. 2. Teams placed more value on manager support than administrator support. 3. Most of the QI teams rated themselves highly on team performance. 4. Team success was higher with more frequent brief, informal team meetings (huddles) and regular participation in team telephone calls. 5. Barriers to implementation included: time constraints, flu outbreaks, manager or staff turnover, team members working different shifts, structural or regional issues, and lack of buy-in from staff. 6. Some participating nursing homes reported an improvement in the work setting and use of best practices by staff. 7. Some participating nursing homes reported an improvement in resident outcomes: less aggressive behaviour, fewer pressure ulcers, and less daily pain. Based on these results decision makers and stakeholders are encouraged to adopt policies, practices, and structures that promote a collaborative culture of quality improvement in residential/long-term care. This culture should include meaningful “bottom-up”, as well as traditional “top down” QI strategies in order to achieve change at the care unit level. 4 |Page SCOPE Final Report, May 2012 Background SCOPE was one of three studies in an applied research program in long-term care: 1. TREC, Translating Research in Elder Care, examined the role of organizational context in establishing best practices in the long-term care (LTC) environment in three Canadian prairie provinces. 2. OPTIC, Older Persons Transitions in Care, looked at the relationship between nursing homes, emergency departments, and medical transfer services in British Columbia and Alberta. 3. SCOPE, Safer Care for Older Persons (in residential) Environments was a two-year quality improvement (QI) project that took place in seven urban nursing homes - two in Alberta, and five in British Columbia, beginning in September 2010. It involved a collaborative approach to QI based on similar models developed by the Institute for Healthcare Improvement for their Breakthrough Series and by the Safer Healthcare Now!, Canadian initiative. The objectives of the SCOPE project were to: 1. support staff in learning and using quality improvement methods to enhance the safety and quality of care of nursing home residents, and 2. improve the quality of worklife for staff providing direct care to older persons in participating nursing homes. It was anticipated that achieving these objectives would also improve resident outcomes in the areas of care on which the QI teams focused: pain, pressure sores, and declining behaviour. The SCOPE project sought to answer several questions. Does the SCOPE process lead to increased use of best practices to inform care provision? Does engaging staff in a QI initiative improve resident outcomes and staff quality of worklife? How does organizational context influence the degree of success of the teams in improving quality and safety of care? How does organizational context affect staff and resident outcomes? Context is the environment or setting where people receive healthcare services or in the case of moving research evidence into practice, the environment or setting where a proposed change is implemented. Appendix A outlines how organizational context is measured. “SCOPE enabled us to build the capacity and confidence of our point-of-care teams. Team members have become champions for Quality Improvement and are making a significant impact on the quality of care of our residents.” -Don McLeod, VP for Organization Effectiveness, Bethany Care Society, Calgary SCOPE Final Report, May 2012 Page |5 The Quality Improvement Initiative SCOPE had two components that ran in parallel: a quality improvement (QI) arm and a research arm. The QI Arm For the purposes of the project, each nursing home formed one or more QI teams consisting of two to three healthcare aides and one to two registered healthcare professionals. A healthcare aide headed each team. In each facility, a senior sponsor was recruited to serve as a champion. Teams selected one of three areas of care to focus on: pain management, behaviour management, or pressure ulcer (skin care) management. The teams then worked to improve that area of care on their unit. SCOPE QI Team Configuration HCA RN QI TEAM HCA Team Leader Senior Sponsor HCA RPT HCA, healthcare aide; RN, registered nurse, and Legend: HCA: Healthcare Aide; RN, registered nurse, and RPT, registered physiotherapist, represent the registered professional; The 12-month QI intervention was RPT, registered physical therapist, represent registered healthcare professionals. designed on the Institute for Healthcare Improvement, Breakthrough Series Collaborative Model. The model is a shared learning system where teams aim to improve their work in care areas. SCOPE Coaching and Change Management Support COACHING & CHANGE MANAGEMENT SUPPORT SCOPE STAFF, QI EXPERTS AND CLINICAL EXPERTS Weekly QI Team Coaching Online Access to Team Data Monthly Feedback Reports Monthly Joint Team Conference Calls Change Packages Emails Throughout the SCOPE intervention, teams received QI training and support that included skill development in QI techniques, provision of change packages, and regular coaching and mentoring. “I believe that this project is a wonderful opportunity to make beneficial changes on the frontline.” -HCA team leader 6 |Page SCOPE Final Report, May 2012 Other key components included face-to-face learning sessions, action periods using the PlanDo-Study-Act cycle, a meeting of all provincial QI teams, and a final celebratory learning congress. The SCOPE Learning Collaborative Model Recruitment of 7 sites (AB and BC) and Formation of QI Teams Selection of Areas of Focus (3-Step Collaborative Process) Tools/Resource Development by Clinical & QI Expertsa AP 1 LS1 AP 2 LS 2 AP 3 PTM b LC COACHING & CHANGE MANAGEMENT SUPPORTS E ma ils S it e Vis it s Ph o n e Ca lls A s s e s s m e n ts S e n i o r L e a d e r R e p o rt s a Co n feren c e Ca lls Team Reports Tools, e.g. change packets b Provincial Team Meetings consisted of regional face-to-face half-day sessions, one for BC and another for AB. Legend: AB, Alberta; AP, Action Period; BC, British Columbia; LC, Learning Congress; LS, Learning Session; PDSA, Plan-Do-Study-Act Cycle; PTM, Provincial Team Meeting; QI, Quality Improvement. The Plan-Do-Study-Act (PDSA) cycle of rapid change was derived from the Model for Improvement (developed by the Associates in Process Improvement), which also provided three fundamental questions used to drive the QI teams’ work: What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in improvement? The Research Arm To learn about organizational context, research use, and staff outcomes (e.g., job satisfaction), healthcare aides in each facility were surveyed before (2010) and after the intervention (2011). Additional data were collected to learn about the facility, how the teams worked, the QI process, and changes in the quality of care to residents. Information collected within the SCOPE research arm included: SCOPE Survey: data on organizational context, staff outcomes, and quality of worklife. Staffing data and facility and unit profiles. QI Data: Monthly assessment of QI processes such as team readiness for change and barriers to change. Resident Assessment Instrument – Minimum Data Set (RAI-MDS 2.0) collected routinely on admission and quarterly from 2009 to 2011 to track resident outcomes. See Appendix B. The QI and resident outcome data were also used in feedback reports to the teams within the PDSA cycles. 1 http://www.apiweb.org/services.html SCOPE Final Report, May 2012 Page |7 Study Results Quality of Team Process Most of the QI teams gave high ratings to their performance as a team. This included assessments of team spirit, standing up for each other, pitching in to help each other, discussion of resident care assignments, and sharing of ideas and information. The teams identified several facilitators and barriers to successful performance. The facilitators were strong team communication, team motivation, team work, and manager support. The perceived barriers were time constraints, leadership issues, change issues, external regional issues, lack of buy-in from the staff, and difficulty engaging staff in the initiative. 7.5 Team Performance Ratings During the QI Intervention STRONGLY AGREE 7 TEAM SPIRIT AMONG MEMBERS 6.5 DEPENDENCE ON EACH OTHER MODERATELY AGREE 6 STAND UP FOR EACH OTHER PITCH IN TO HELP EACH OTHER 5.5 SLIGHTLY AGREE 5 4.5 NEUTRAL 4 A B C D E NURSING HOMES F G Quality of Worklife Comparing SCOPE survey scores before and after the QI initiative, ratings of the work setting and the use of best practices showed a trend towards improvement in some of the participating nursing homes. Positive change in practice measures included: using data to assess and improve on performance, thinking about best practice and how to do it (conceptual research use), and the perception of the amount of time healthcare aides have to deliver care on their unit. Conceptual Research Use in SCOPE Units. 3.8 SCOPE Units 3.7 Non-SCOPE Units 3.6 Pre-SCOPE 8 |Page Post-SCOPE SCOPE Final Report, May 2012 Quality of Care and Resident Outcomes The quality of care also showed an improvement in resident outcomes in some of the SCOPE units. The figure below illustrates how staff in one nursing home focused on improving skin care using a resident turning schedule. The proportion of resident turns completed increased to 100% during the intervention and was maintained at that level throughout the following 5 months. Percentage of Turning, Turns Completed Completion of Resident Facility X, Mar–Oct 2011. 100% 100% 80% 91 % 60% 20% 30% 1 3 5 7 9 Time 11 13 15 17 In a number of facilities, the targeted resident outcomes also showed improvements in the RAI quality indicators. These RAI indicators will continue to be monitored for further changes over time. Trends in the Resident Outcomes During SCOPE QI Team Facility 1 A 2 Topic Area Skin Trend over the course of SCOPE Decreasing RAI QI indicator Stage 2-4 Pressure Ulcer A Pain Stable Mild to Severe Pain, Daily 3 A Behaviour Stable Declining Behavioural Symptoms 4 B Behaviour Improving Declining Behavioural Symptoms 5 B Pain Decreasing Mild to Severe Pain, Daily 6 C Behaviour Got worse Declining Behavioural Symptoms 7 D Pain Improving Mild to Severe Pain, Daily 8 E Behaviour Improving Declining Behavioural Symptoms 9 F Pain Stable Worsening Pain 10 G Skin Improved Stage 2-4 Pressure Ulcer SCOPE Final Report, May 2012 Page |9 Key Learnings 1. The QI initiative strengthened the QI teams’ knowledge and capacity to achieve change. 2. The QI teams valued engagement and support from managers and senior leaders. 3. The teams found the QI advisors’ coaching helpful. 4. Using facility (local) RAI-MDS 2.0 data helped track team progress on their QI activities. 5. Quality of care and worklife showed highly promising trends toward improvement with QI support. Good communication and frequent team huddles were essential in the QI team’s success. Where to from here? SCOPEOut is a one-year follow-up to the proof of principle project aimed at measuring the dynamics of spread and sustainability of the SCOPE-initiated: quality improvement activity, clinical care, quality of worklife, and attitudes to uptake research-informed practices All 7 SCOPE facilities are participating in SCOPEOut . 10 | P a g e SCOPE Final Report, May 2012 Appendices Appendix A. The Alberta Context Tool Context is the environment or setting where people receive healthcare services or in the case of moving research evidence into practice, the environment or setting where a proposed change is implemented. The SCOPE Survey uses the Alberta Context Tool (ACT) which measures variables that can have an effect on an organization’s environment. The three core dimensions of context looked at based on the PARIHS framework are culture, leadership, and evaluation, (http://www.parihs.org). Other dimensions we looked at include organizational slack, formal interactions, informal interactions, structural and electronic resources, and social capital. The Alberta Context Tool Framework Leadership Plus: • Organizational slack (time, space, staff) Context Culture • Formal interactions • Informal interactions • Resources Evaluation (Feedback) • Social capital Appendix B. The RAI-MDS 2.0 The Resident Assessment Instrument – Minimum Data Set 2.0 is used to assess the needs and risks of residents in long-term care. It measures 24 indicators for quality of care, e.g. behavioural patterns, physician functioning, and nutrition.2 The SCOPE Project used the RAIMDS indicators for the selected care areas in behaviour, pain, and skin ulcers. Some of the RAI-MDS 2.0 Quality Indicators used in SCOPE. QI indicator Percentage of residents with... DAILY PAIN Mild to severe daily pain on a daily basis BEHD 4 Declining behavioural symptoms PRU 05 Stage 2-4 Pressure ulcers PAN 01 Worsening pain 2 Hutchinson et al., The Resident Assessment Instrument-Minimum Data Set 2.0 quality indicators: a systematic review BMC Health Services Research 2010, 10:166. SCOPE Final Report, May 2012 P a g e | 11 Acknowledgement SCOPE is grateful for the participation and enthusiasm of the administrative and care staff of the following nursing homes: Bethany Care Society, Capital Care Lynnwood, The Gateby, Noric House, Pleasant Valley Manor, Trinity Care Centre, Westview Place Principal Investigator Carole A. Estabrooks, RN, PhD, FCAHS, FAAN Professor & Canada Research Chair in Knowledge Translation, Faculty of Nursing, University of Alberta Co-Investigators Peter G. Norton, MD, PhD, FRCPSC Greta G. Cummings, RN, PhD, FCAHS Lisa Cranley, RN, PhD Professor, Department of Family Medicine, University of Calgary Professor, Faculty of Nursing University of Alberta Postdoctoral Fellow, Faculty of Nursing University of Alberta Research Team Debbie Barnard Marlies van-Djik Project Manager, University of Alberta Julia Arsenault QI Consultant, BC Patient Safety & Quality Council (formerly with Safer Healthcare Now) Quality Improvement Advisor, University of Alberta Peter George Tian Carole Taylor Project Coordinator, University of Alberta Quality Improvement Advisor, University of Alberta Mehvash Qureshi Research Assistant, University of Alberta Decision Makers Alberta Caroline Clark British Columbia Joanne Konnert Executive Director, Seniors Health, Alberta Health Services, Edmonton Vice President, Tertiary Services, Interior Health Authority, British Columbia Belle Gowriluk Cindy Regier Director, Supportive Living Services, Alberta Health Services, Calgary Director, Residential Services, Interior Health Authority, British Columbia Funding Funding for this project is provided through a contribution agreement with Health Canada (CA# 6804-152009/9180076). We gratefully acknowledge the British Columbia Quality Council and the Canadian Institutes of Health Research--Institute of Aging (201102MPA-248060-MPA-CBAA-55100) for their financial contribution to the project. Production of this final report has been made possible through a financial contribution from Health Canada. The views expressed herein do not necessarily represent the views of Health Canada. Contact Details Carole A. Estabrooks, RN, PhD, FCAHS, FAAN Safer Care for Older Persons (in residential) Environments (SCOPE) Knowledge Utilization Studies Program, Faculty of Nursing, University of Alberta 5-007 Edmonton Clinic Health Academy, 11405 87 Avenue, Edmonton, Alberta T6G 1C9 Telephone: (780-) 492-3451 or 492-6187; Fax: (780-) 492-6186 Email: carole.estabrooks@ualberta.ca Webpage: http://www.trec.ualberta.ca/en/SCOPE.aspx; http://www.kusp.ualberta.ca 12 | P a g e SCOPE Final Report, May 2012