Rana et al Final (ref comm edit) - Spiral
advertisement
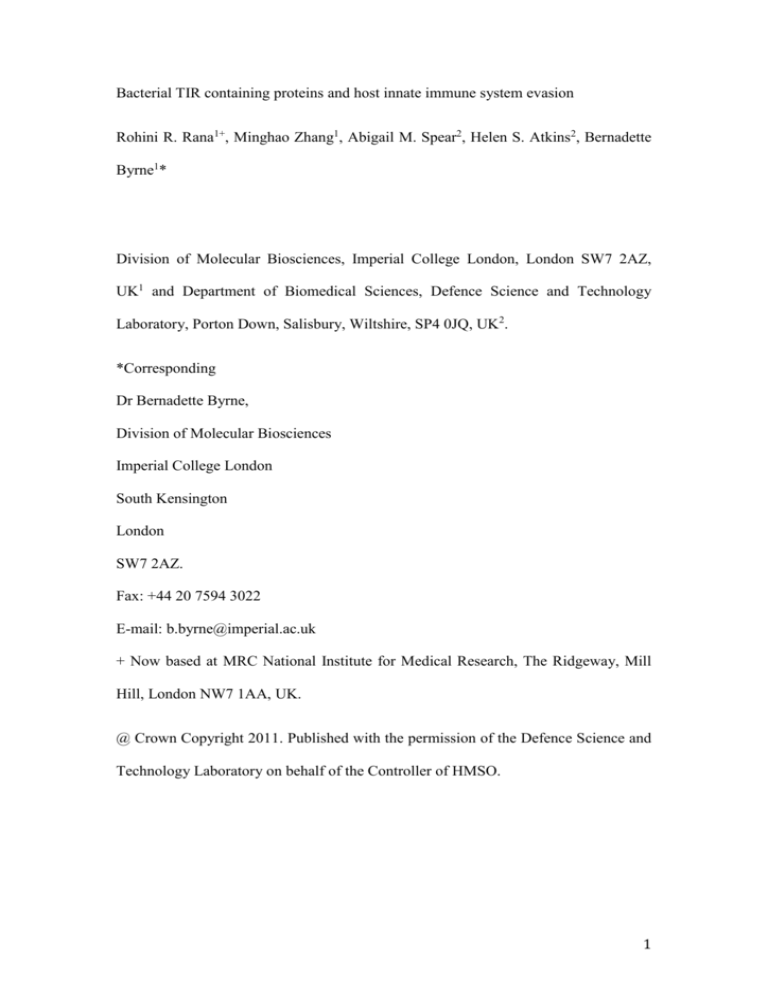
Bacterial TIR containing proteins and host innate immune system evasion Rohini R. Rana1+, Minghao Zhang1, Abigail M. Spear2, Helen S. Atkins2, Bernadette Byrne1* Division of Molecular Biosciences, Imperial College London, London SW7 2AZ, UK1 and Department of Biomedical Sciences, Defence Science and Technology Laboratory, Porton Down, Salisbury, Wiltshire, SP4 0JQ, UK2. *Corresponding Dr Bernadette Byrne, Division of Molecular Biosciences Imperial College London South Kensington London SW7 2AZ. Fax: +44 20 7594 3022 E-mail: b.byrne@imperial.ac.uk + Now based at MRC National Institute for Medical Research, The Ridgeway, Mill Hill, London NW7 1AA, UK. @ Crown Copyright 2011. Published with the permission of the Defence Science and Technology Laboratory on behalf of the Controller of HMSO. 1 Abstract The innate immune system provides the first line of host defence against invading pathogens. Key to upregulation of the innate immune response are Toll-like receptors (TLRs) which recognise pathogen-associated molecular patterns (PAMPs) and trigger a signaling pathway culminating in the production of inflammatory mediators. Central to this TLR signaling pathway are heterotypic protein-protein interactions mediated through Toll/Interleukin-1 receptor (TIR) domains found in both the cytoplasmic regions of TLRs and adaptor proteins. Pathogenic bacteria have developed a range of ingenuous strategies to evade the host immune mechanisms. Recent work has identified a potentially novel evasion mechanism involving bacterial TIR domain proteins. Such domains have been identified in a wide range of pathogenic bacteria and there is evidence to suggest that they interfere directly with the TLR signaling pathway and thus inhibit the activation of NFB. The individual TIR domains from the pathogenic bacteria Salmonella enterica serovar Enteritidis, Brucella sp, uropathogenic E. coli and Yersinia pestis have been analysed in detail. The individual bacterial TIR domains from these pathogenic bacteria seem to differ in their modes of action and their roles in virulence. Here we review the current state of knowledge on the possible roles and mechanisms of action of the bacterial TIR domains. Keywords: TLR signaling pathway, TIR domain, innate immunity, pathogenic bacteria, bacterial TIR domain, virulence 2 The innate immune system and TLRs Upregulation of the innate immune system provides the first line of host defence against invading pathogens. Key components of the innate immune system are pattern recognition receptors (PRRs) which recognise pathogen-associated molecular patterns (PAMPs) and initiate an intracellular signaling cascade culminating in a host immune response [1]. The best-studied PRRs are the Toll-like receptors (TLRs), type I transmembrane sensory receptors that recognise a range of PAMPs from pathogenic bacteria, fungi, viruses and parasitic-protozoa [1]. The principal role of the TLRs is in regulation of the innate immune system however there is evidence to show that they also play important functions in shaping adaptive immune responses, particularly in combination with other PRRs [2]. TLRs are expressed on immune cells such as phagocytes, B cells and certain T cells, and on non-immune cells including fibroblasts and epithelial cells. They can be located on the cell surface (TLR1-2, TLR4-6 and TLR10) or in intracellular compartments such as endosomes (TLR3 and TLR7-9) [1,3]. Ten TLRs are encoded in the human genome, each of which has evolved to recognise certain PAMPs from a broad range of microbes. For instance, TLRs signal the presence of triacyl lipopeptides (Pam3CSK4; TLR1/2), peptidoglycan and zymosan (TLR2), double-stranded ribonucleic acid (ds RNA; TLR3), lipopolysaccharides (LPS) of Gram-negative bacteria (TLR4), flagellin (TLR5), single-stranded RNA (ss RNA; TLR7 and TLR8) and unmethylated CpG DNA (TLR9) [3,4]. The ligand for TLR10 is currently unknown. The expression of the different TLRs is subject to change and is regulated by rapid cellular responses to pathogens, various cytokines and environmental stresses [1]. 3 The TLRs contain an extracellular leucine-rich repeat (LRR) domain that recognises and binds to specific microbial ligands [5]. Linked to the LRR domain by a single transmembrane domain [6] is a cytoplasmically located Toll/Interleukin-1 receptor (TIR) domain that mediates downstream signaling [7]. TLRs are thought to exist as dimers, which can be heterotypic, homotypic or both depending of the receptor [8,9]. Upon interaction with a PAMP the TLR dimer undergoes a molecular rearrangement of the intracellular TIR domains to form an active interaction domain allowing recruitment of adaptor molecules [4,8,9]. TLR signalling pathways converge to activate transcription factors that regulate the induction of proinflammatory cytokines and co-stimulatory molecules [5]. This in turn elicits innate immune responses against the invading pathogens. One of the key features of TLR signaling is that the signal is both initiated and propagated by heterotypic TIR-TIR interactions (Fig 1). In addition to the TIR domains of the TLR receptors there are five TIR containing adaptor proteins [10]; myeloid differentiation factor 88 (MyD88), TIR domain containing adaptor protein including interferon- (TRIF), MyD88-adaptor like (MAL, also called TIRAP), TRIF-related adaptor molecule (TRAM) and sterile - and armadillo-motifcontaining protein (SARM). The MyD88-mediated pathway leads to the activation of NFκB and MAP kinase pathways inducing the production and release of proinflammatory cytokines [5]. The TRIF-mediated pathway leads to activation of interferon response factors (IRFs) inducing the production of type I interferon [11]. All TLRs and IL-1Rs, except TLR3, signal through the MyD88-dependent pathway while TLR3 and TLR4 function through the MyD88-independent pathway (TRIF; [12]). TLR1, TLR2, TLR4 and TLR6 additionally recruit the TIR domain bridging adaptor MAL, which mediates the interactions between the TIR domains of TLRs and 4 MyD88 [13]. Similarly, TLR4 recruits the alternative TIR domain bridging adaptor, TRAM, in addition to TRIF to link between the TIR domain of TLR4 and TRIF [14] (Fig 1). The final TIR containing adaptor, SARM, acts as a negative regulator of TRIF signaling [15]. TIR domains The cytoplasmic TIR domains of TLRs typically contain 150-200 amino acid residues [16]. As mentioned the principal role of TIR domains is the mediation of heterotypic protein-protein interactions between receptor and adaptor molecules in the signal transduction process. TIR domains share common sequence motifs, called box 1 (F/Y)-DAFISY), box 2 (GYKLC-RD-PG) and box 3 (a conserved W surrounded by basic residues), of which boxes 1 and 2 are vital for mediating signalling [12,17] (Fig 2). One of the most functionally important regions of the TIR domains is the BB loop (Fig 2 and Fig 3), part of the Box 2 region. This motif is comprised of the sequence RDxPG (where x is any residue and is a hydrophobic residue). Site-directed mutagenesis studies have revealed that several residues within this loop are important for TLR signal transduction. This is most notable in the case of the Pro residue. Mutation of this residue, Pro712, to His in TLR4-TIR results in a loss of TLR signalling in response to lipopolysaccharide [18]. A summary of all the current solved structures of TIR domains is given in Table 1. The structure of the human TIR domain of TLR1 reveals a central fivestranded parallel β-sheet (βA - βE) surrounded by five helices (A - E) and the connecting loops (Fig 2 and Fig 3) [19]. The functionally relevant BB loop (Fig 2 and Fig 3) connects strand βB and helix B, which protrudes out from the main core of the protein in most structures of TIR domains [16,19-22]. Whilst the core structure is 5 maintained in most TIR domains, some conformational differences are observed even in the case of the TIR domains of TLR1 and TLR2 which share 50% sequence identity [19]. The regions of the proteins that exhibit the largest variation include the helices B and D and the loops BB, CD and DD. Such structural diversity is suggested to be crucial for the specificity of signal transduction from different receptors [19,23]. The recent structure of MAL lacks the helix connecting the B and C strands. This region of the protein is present as a long flexible loop which links the A helix and the B strand [22]. It is not clear precisely why there is less order in this region of MAL compared to the other TIR domains however it seems likely that this is important for function. Microbial targeting of the TLR signaling pathway Research over the last decade or so has highlighted that the TLR signaling pathway is a key target of pathogen mechanisms of host immune system evasion. One of the strategies for successful host evasion involves manipulation of the TLR signaling pathway via modification of microbial PAMPs so that they are less effective at stimulating the TLRs. An example of this can be seen with the modification in Lipid A content of Yersinia pestis with changing growth temperature [24]. Alternatively, by co-stimulating host carbohydrate binding receptors as well as TLRs it has been shown that Mycobacterium tuberculosis [25] is able to initiate anti-inflammatory mechanisms counteracting the effects of TLR signaling. Viruses have been shown to target various levels of the TLR signaling pathway. The A46R and A52R proteins from vaccinia virus reduce TLR signaling by forming interactions with a range of host TIR containing proteins including MyD88, MAL, TRIF and TRAM [26] as well as 6 TLR4 [27]. Based on sequence homology to the Box2 region of TIR domains it was thought that A46R and A52R function as negative regulators of the heterotypic TIRTIR interactions involved in upregulating the TLR signaling pathway through competitive binding with host TIR domain proteins. However A52R has also been shown to form direct association with Interleukin-1 receptor-associated kinase-like 2 (IRAK2) [28], a component of the TLR signaling pathway which does not contain a TIR domain, so it may be that the role of this protein is more general. The suggestion that the viral proteins are not TIR containing proteins, is supported by analysis using bioinformatics tools which were unable to find known TIR domains using A46 as a search protein or find TIR domains using A46 as a search protein [29]. There are proteins in other viruses such as Hepatitis B that also interact with components of the TLR signaling pathways probably in a similar way to the vaccinia proteins [30]. In contrast, the Karposi’s sarcoma virus replication and transcription activator (RTA) causes degradation of TRIF [31]. Bacterial TIRs and their prevalence throughout bacterial species A new potential host evasion mechanism involving TLRs came to light with the identification of bacterial TIR homologues. The first report described the identification >200 TIR homologues in a wide range of bacterial species including Staphylococcus aureus, Brucella melitensis and Salmonella enterica serovar Enteriditis [32]. Sequence alignment of the so-called TIR-like protein A (TlpA) from S. enterica serovar Enteriditis with the TIR domains of human TLR6, TLR4 and MyD88, revealed high sequence homology in the box 1 region [32]. Subsequent work identified Paracoccus denitrificans TIR-like protein (PdTLP) as a homologue of S. 7 enterica serovar Enteriditis tlpA, sharing 39% sequence similarity over 255 residues [33]. Cirl et al. [34] identified bacterial TIR domains in the CFT073 strain of uropathogenic Escherichia coli and in Brucella species, which were termed TIR domain containing proteins C (TcpC) and B (TcpB, also known as Btp1). A more comprehensive bioinformatics analysis by Spear et al. [29] identified 922 bacterial TIR domains in a wide range of both pathogenic and non-pathogenic bacterial species including the plague-causing bacterium, Yersinia pestis. More recently a study identified a substantially lower number of 483 bacterial TIR domains proteins [35]. It is possible that this is due to subtle differences in the search methodologies used to find the proteins. An intriguing finding was revealed by recent research by Zhang et al [35] demonstrating that animal SARM is more closely related to the bacterial TIR domain proteins than it is to the other animal TIR adaptors suggesting a common origin for these proteins. The bacterial TIR proteins are approximately 230 to 310 amino acids long with the conserved TIR domain comprised of 150-200 amino acids. The TIR domain can be located in either the C-terminal or the N-terminal region and the remaining region of the protein can be highly variable. In the TlpA and PdTLP proteins the TIR domain is located within the C-terminal region with an N-terminal region postulated to comprise a highly -helical coiled coil domain. The presence of a coiled coil domain was supported by circular dichroism analysis on the N-terminal region of PdTLP indicating a high -helical content [33]. In contrast in the case of TcpC the Nterminal region has been annotated as a putative transmembrane segment while the Nterminal domain of TcpB has been identified as a lipid binding domain with specificity for phosphoinositide phosphates. The recent bioinformatic analysis highlights the co-occurrence of the TIR domains with a range of different domains 8 [29]. Examples include the presence of an N-terminal TIR domain followed by Cterminal tetratricopeptide repeats (TPR), common protein-protein interaction domains, in Frankia sp. [29]. Bacterial TIR containing proteins in Beggiatos sp. contain an N-terminal Mettallophos domain involved in phosphorylation, while in Clostridium thermocellum it contains C-terminal trypsin, a serine-protease domain, and in Mariprofundus ferroxydans it contains a C-terminal Mrr-cat, a type IV restriction endonuclease domain [29]. Bacterial TIR proteins and the TLR signaling pathway The majority of studies on bacterial TIR proteins have focused on their potential role as virulence factors that directly subvert host TLR signaling. Newman et al. [32] in the first studies on a bacterial TIR showed that S. enterica serovar Enteritidis TlpA suppresses the induction of NFB activation by the mammalian TIRcontaining proteins TLR4, IL-1R and MyD88 but does not suppress NFB activation induced by the cytokine TNF in cultured mammalian cells. Most notably, mice infected with genetic knockouts of S. enterica serovar Enteritidis lacking the TlpA encoding gene showed increased time to death compared to mice infected with the wild-type strain. The TlpA knockout strain also demonstrated a reduced ability to survive in cultured mammalian cells [32]. These data strongly suggested that the TlpA was important for virulence of S. enterica serovar Enteritidis via a mechanism of inhibition of the TLR signaling pathway responsible for activation of NFB. Support for both a role in virulence and the general mechanism of action of bacterial TIR proteins came from further studies on homologues from Brucella melitensis (TcpB [also known as Btp1]; [34,36]) and the uropathogenic E. coli strain CFT073 (TcpC; [34]). One study revealed that both TcpB and TcpC suppress TLR2- 9 and TLR4-mediated activation of NFB but do not suppress the activation of NFB induced by the TIR-independent cytokine TNF and that a TcpC knockout strain showed a reduced ability to survive in mouse RAW264.7 macrophage cells compared to wild-type CFT073 [34]. It was possible to achieve wild-type accumulation rates in RAW264.7 cells when the TcpC knockout was complemented with a plasmid borne copy of TcpC. In addition, a comparison using a mouse model of urinary tract infections revealed that the TcpC knockout strain had reduced virulence compared to wild-type [34]. A further in-depth analysis of the precise sites of activity of the bacterial TIR proteins revealed that TcpB and the purified TIR domain of TcpC (TcpC-TIR) interacted with endogenous MyD88 in mammalian cell lines [34]. Pulldown assays confirmed the interaction of TcpC-TIR directly with MyD88 but revealed a lack of interaction with two other TIR containing mammalian proteins TLR2-TIR and TRIF, or two non-TIR domain containing components of the TLR signaling pathway, IRAK1 and IRAK4 [34]. More recently there is some evidence to suggest that TcpC also interacts with TLR4 [37]. Other TIR containing proteins involved in TLR signaling, for example MAL and TRAM, have not been tested so far for interaction with TcpC. Based on sequence similarity, plasma membrane localization profile and the ability to inhibit MAL-induced NFkB activation it has been suggested that TcpB acts as a MAL mimic and competes with MAL for binding of MyD88 [36]. However more recent research suggests that TcpB only interacts with MAL and not MyD88 and does not block the interaction between these two proteins [38]. Instead, data indicate that TcpB interaction results in a reduction in the cellular levels of MAL in mammalian cells expressing TcpB [38]. It has been suggested that interaction with TcpB results in ubiquitination and targeting of MAL for degradation. Since TcpB is unlikely to act 10 directly as a ubiquitin ligase it is possible that TcpB binding causes degradation by indirect means [38]. Studies on TcpB from Brucella abortus have identified a role in inhibition of maturation of infected dendritic cells, suggested to act as key cellular environments for pathogen proliferation [39]. Most recently research has focused on the TIR protein from the plague causing bacterium, Yersinia pestis (YpTdp). In an in vitro reporter assay YpTdp inhibits activation of NFB, although the TIR domain only (YpTIR) has no effect [40]. However, pull-down assays show that YpTIR does form interactions with MyD88-TIR [40] suggesting that in this case the N-terminal, non-TIR, domain of the YpTdp also plays a role in inhibition of the TLR signaling pathway. Both inhibition of NFκB by YpTdp and interaction of YpTIR with MyD88-TIR are dependent upon the proline residue located on the BB loop [40]. This indicates that YpTdp mediates the downregulation of the innate immune system through competitive interaction with MyD88 as described for TcpC [34]. Studies with a genetic deletion mutant of Y. pestis indicate that YpTdp does not have a role in virulence of the organism. It is possible that any effects on virulence in this case are minor. Y. pestis employs a very sophisticated system of infection and evasion mechanisms. For example YopJ, a protease delivered into host cells via the type III section system (TTSS) is known to block NFB activation by TLR receptors [41]. Since it appears that in Y. pestis there is some redundancy in the mechanisms employed to inhibit NFB activation it is possible that the YopJ is masking the effects of YpTdp on the virulence of Y. pestis. The data reported so far on bacterial TIR proteins strongly indicates that there is no one clear mechanism by which they act to subvert the host immune system. 11 TcpC and TlpA show direct interactions with components of the TLR signaling pathway and are likely to directly block the pathway whereas TcpB seems to trigger the degradation of one key component and thus reduce signaling. While it seems clear that in some cases the bacterial TIR domains play a role in virulence in the case of YpTdp, the protein lacks any clear relevance for virulence despite inhibiting NFB activation. It seems likely that the TIR proteins from these pathogenic bacteria have different roles which means that only by studying a range of these can we really understand the full breadth of functions. TIR domains in non-pathogenic bacteria As mentioned above TIR domains have been identified in a range of both pathogenic and non-pathogenic bacterial species [29]. To account for this it has been suggested that the TIR domain is a generic protein-protein interaction domain which has subsequently been adapted to function as a mechanism of host immune system evasion [29]. However, whilst the roles of the TIR domains in the non-pathogenic bacteria remain uncharacterized there is evidence to show that these can be used to understand the mechanism of action of the TIR domains from pathogenic bacteria. This is illustrated by research carried out on the TIR domain protein from Paracoccus denitrificans (PdTdp). Intriguingly this protein interacts with both MyD88 and TLR4 [33] and is the only bacterial TIR protein for which there is a high resolution structure ([42]; see below for a more detailed discussion). This has allowed the first insights into the domains involved in bacterial TIR domain interaction with MyD88. Anecdotal reports and our own experiences indicate that bacterial TIR domain proteins are challenging to express and purify. However the data from the P. denitrificans studies indicates that PdTdp is a suitable homologue for studying some aspects of the function of TIR domains in pathogenic bacteria. 12 How do the bacterial TIR proteins localise to the host cell cytoplasm Sequence analysis of the regions around tlpA revealed a phage origin for tlpA as well as links with pilin-related domains [32]. Since pilins are extracellular proteins playing roles in cell adhesion, it was suggested that proteins encoded within this genomic region including TlpA are secreted [32]. However further links with the type III or type IV secretion systems could not be made on the basis of gene location due to discontinuous genome sequence of S. enterica in this region [32]. To date, no more direct evidence of secretion of TlpA has been reported. TcpC has been reported to be secreted into the media of cultured bacterial cells and taken up into host macrophages in a cholesterol-dependent manner to interfere with TLR-mediated TNF induction [34]. The secretion mechanism has yet to be identified for TcpC as the protein does not contain a recognizable signal sequence. As mentioned previously, TcpB has been shown to contain an N-terminal lipid binding domain which is suggested to important for cell permeability. Indeed purified MBP-TcpB internalizes into mouse macrophages in a dose dependent manner [43]. The YpTdp does not contain any known signal sequences and no mechanism of secretion has yet been identified [40]. As yet there is no clear consensus on the mechanism by which TIR domains localize to the host cytosol and the data so far indicates that there may be different mechanisms depending on the pathogen. Further studies are needed to clarify this issue perhaps by performing real-time imaging and co-localisation studies. 13 Biophysical characterization of bacterial TIR proteins Preliminary biophysical characterization of bacterial TIR proteins by molecular modelling indicated that they share considerable structural homology with the TIR domain of TLR1 [34]. This was confirmed by the first crystal structure of a bacterial TIR protein, PdTIR (Table 1), which revealed an overall fold identical to the known structures of the human TIR domains [42]. The asymmetric unit of the PdTIR crystals contains four molecules that form two equivalent dimers [42]. Unlike the homodimer interface observed in the structure of the human TLR10-TIR [20] involving mainly the BB loops (Figs 2 and 3; Table 1), the dimer interface in PdTIR involves the D-helix, the DD- and EE-loops leaving the BB-loops largely exposed on the surface of the molecules [42]. A large network of hydrogen bonds mediates dimerisation of the PdTIR protomers in the crystal structure. The crystal structures of a number of TIR domains [16,19,20,22,42] indicates the formation of dimers in the crystal lattice. In contrast, the purified proteins are all present as monomers in solution although there is some evidence to suggest that TIR domains function as weakly associated dimers [44]. In contrast to all the other biochemically characterized TIR domains YpTIR forms dimers in solution which are likely to be disulphide bond dependent [45]. Mutation of one of the two Cys residues to Ser present in YpTIR retains the dimeric form of the protein whereas mutation of both results in highly unstable protein not suitable for analysis. Interestingly this study showed that mutation of Cys132 to Ser abolished interaction with MyD88 suggesting that the disulphide bonds may be key in maintaining an active confirmation of YpTIR [45]. 14 The structure of PdTIR indicated that the highly exposed BB loop is the region of PdTIR which interacts with human TIR proteins of the TLR signaling pathway [42]. The importance of the BB loop region in interactions between bacterial TIR domains and human adaptor proteins has been demonstrated by mutagenesis studies. Pull-down studies on a Pro173His mutant of YpTIR shows no detectable interaction with GST-MyD88-TIR in contrast to the wild-type protein [40]. In addition, mutation of another highly conserved residue of the BB loop Gly158 to an Ala resulted in a TcpB with reduced activity in a NFkB reporter assay [36]. However it should be noted that there is variability in this region of the bacterial TIR domains with TcpB and YpTdp lacking the conserved Pro and Gly residues respectively. While these studies strongly suggest that the BB loop is essential for bacterial TIR activity only a structure of a bacterial TIR domain in complex with a human adaptor protein will provide definitive characterization of the interaction domain. Other roles of bacterial TIR domains While the majority of studies have focused on the role of bacterial TIR domains in direct inhibition of the TLR signaling pathway through competitive binding of human adaptor proteins recent research has highlighted another possible function. Radhakrishnan and colleagues [46] have shown that exposure of microtubules to TcpB expression results in improved nucleation and growth of microtubules in vitro. Preliminary results show that this activity is mediated by the BB loop. The significance of this effect of TcpB in terms of immune system evasion remains to be clarified although the authors of the study speculate that this may be a 15 further mechanism by which the upregulation of the NFkB signaling pathway is inhibited. The first study on bacterial TIR proteins indicated that expression of TlpA from S. enterica serovar Enteritidis resulted in activation of caspase-1, a host protease [32]. Activation of this protease results in cleavage, activation and secretion of the proinflammatory cytokine IL-1. An increase in IL-1 secretion was observed in cultured cells expressing TlpA and in macrophages infected with wild-type S. enterica serovar Enteritidis compared to the tlpA deletion strain. This rather surprising finding suggests that TlpA is capable of both simulating and inhibiting proinflammatory cytokine production. Recent research has indicated that YopJ from Y. pestis also has such a dual role [47]. It has been suggested that the upregulation of caspase-1 may represent a mechanism of host defence against pathogens able to inhibit the NKB pathway. It will be interesting to see if bacterial TIR domain proteins in addition to TlpA are able to stimulate this host cell response. The YpTdp deletion mutant shows some interesting phenotypes including increased auto-aggregation and reduced ability to survive in high salt conditions when compared to wild-type Y. pestis [40]. These features may contribute to the ability of the Y. pestis to survive in the host and thus increase pathogenicity. They also suggest functions of the YpTdp in addition to inhibition of TLR signaling. Overall, the widespread distribution of TIR domains in non-pathogenic bacterial species as well as the diversity of the associated protein domains [29] is strongly indicative that these TIR containing proteins have roles other than in immune system evasion. However it remains to be seen what these other possible roles are. 16 Microbial TIR domains as therapeutic agents Upregulation of the innate immune response is highly advantageous to host survival although anomalous upregulation has been implicated in a number of autoimmune and inflammatory diseases including multiple sclerosis and rheumatoid arthritis [48]. In addition, research has also highlighted the role of NFB in cancer. Overactivation of NFB as the result of mutagenesis of proteins in the TLR signaling pathway may contribute to cell proliferation [49]. Recently, highly potent TLR signaling inhibitors have been generated based on the A46R protein from vaccinia virus [50]. Previous studies have shown it is possible to make cell-penetrating peptides based on the BB-loops of the TIR domains [51] of both adaptor proteins and TLRs which inhibit TLR signaling pathways. The wide variety of ways in which bacterial TIR domains modulate the TLR signaling pathway means that it may be possible to design peptides which target different components of the pathway and thus have subtly different effects on the innate immune system. These represent a means of tuning the innate immune response to possibly alleviate some of the symptoms of debilitating auto-immune diseases and potentially treat some cancers. Conclusion The current evidence strongly suggests that bacterial TIR domains represent a novel mechanism by which pathogens can subvert the host immune system. However questions remain regarding how the bacterial TIR domains are taken up into host cells and at what points in the TLR signaling pathway they can form negatively regulating interactions. Some of the studies seem to indicate that while the bacterial TIR domains share some common features there is a certain amount of individuality in 17 their interaction profiles and precise functions. Further research is required in order to elucidate the precise mechanism of action of these interesting molecules. Acknowledgements This work was funded by the UK Ministry of Defence. References 1. Akira S, Uematsu S, Takeuchi O (2006) Pathogen recognition and innate immunity. Cell 124:783–801. 2. Fritz JH, Le Bourhis L, Sellge G, Magalhaes JG, Fsihi H, Kufer TA, Collins C, Viala J, Ferrero RL, Girardin SE, et al. (2007) Nod1-mediated innate immune recognition of peptidoglycan contributes to the onset of adaptive immunity. Immunity 26:445–459. 3. Kumar H, Kawai T, Akira S (2009) Pathogen recognition in the innate immune response. Biochem J 420:1–16. 4. Gay NJ, Gangloff M (2007) Structure and function of Toll receptors and their ligands. Annu Rev Biochem 76:141–165. 5. Akira S, Takeda K (2004) Toll-like receptor signalling. Nat Rev Immunol 4:499–511. 6. Hashimoto C, Hudson KL, Anderson KV (1988) The Toll gene of Drosophila, required for dorsal-ventral embryonic polarity, appears to encode a transmembrane protein. Cell 52:269–279. 7. Gay NJ, Keith FJ (1991) Drosophila Toll and IL-1 receptor. Nature 351:355– 356. 8. Triantafilou M, Gamper FGJ, Haston RM, Mouratis MA, Morath S, Hartung T, Triantafilou K (2006) Membrane sorting of toll-like receptor (TLR)-2/6 and TLR2/1 heterodimers at the cell surface determines heterotypic associations with CD36 and intracellular targeting. J Biol Chem 281:31002–31011. 9. Latz E, Verma A, Visintin A, Gong M, Sirois CM, Klein DCG, Monks BG, 18 McKnight CJ, Lamphier MS, Duprex WP, et al. (2007) Ligand-induced conformational changes allosterically activate Toll-like receptor 9. Nat Immunol 8:772–779. 10. O'Neill LAJ, Bowie AG (2007) The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling. Nat Rev Immunol 7:353–364. 11. Núñez Miguel R, Wong J, Westoll JF, Brooks HJ, O'Neill LAJ, Gay NJ, Bryant CE, Monie TP (2007) A dimer of the Toll-like receptor 4 cytoplasmic domain provides a specific scaffold for the recruitment of signalling adaptor proteins. PLoS ONE 2:e788. 12. Brown V, Brown RA, Ozinsky A, Hesselberth JR, Fields S (2006) Binding specificity of Toll-like receptor cytoplasmic domains. Eur. J. Immunol. 36:742–753. 13. Horng T, Barton GM, Flavell RA, Medzhitov R (2002) The adaptor molecule TIRAP provides signalling specificity for Toll-like receptors. Nature 420:329– 333. 14. Rowe DC, McGettrick AF, Latz E, Monks BG, Gay NJ, Yamamoto M, Akira S, O'Neill LA, Fitzgerald KA, Golenbock DT (2006) The myristoylation of TRIF-related adaptor molecule is essential for Toll-like receptor 4 signal transduction. Proc Natl Acad Sci USA 103:6299–6304. 15. Carty M, Goodbody R, Schröder M, Stack J, Moynagh PN, Bowie AG (2006) The human adaptor SARM negatively regulates adaptor protein TRIFdependent Toll-like receptor signaling. Nat Immunol 7:1074–1081. 16. Khan JA, Brint EK, O'Neill LAJ, Tong L (2004) Crystal structure of the Toll/interleukin-1 receptor domain of human IL-1RAPL. J Biol Chem 279:31664–31670. 17. Slack JL, Schooley K, Bonnert TP, Mitcham JL, Qwarnstrom EE, Sims JE, Dower SK (2000) Identification of two major sites in the type I interleukin-1 receptor cytoplasmic region responsible for coupling to pro-inflammatory signaling pathways. J Biol Chem 275:4670–4678. 18. Poltorak A, He X, Smirnova I, Liu MY, van Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, et al. (1998) Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282:2085– 2088. 19. Xu Y, Tao X, Shen B, Horng T, Medzhitov R, Manley JL, Tong L (2000) Structural basis for signal transduction by the Toll/interleukin-1 receptor domains. Nature 408:111–115. 20. Nyman T, Stenmark P, Flodin S, Johansson I, Hammarström M, Nordlund P (2008) The crystal structure of the human toll-like receptor 10 cytoplasmic domain reveals a putative signaling dimer. J Biol Chem 283:11861–11865. 21. Ohnishi H, Tochio H, Kato Z, Orii KE, Li A, Kimura T, Hiroaki H, Kondo N, 19 Shirakawa M (2009) Structural basis for the multiple interactions of the MyD88 TIR domain in TLR4 signaling. Proc Natl Acad Sci USA 106:10260– 10265. 22. Valkov E, Stamp A, Dimaio F, Baker D, Verstak B, Roversi P, Kellie S, Sweet MJ, Mansell A, Gay NJ, et al. (2011) Crystal structure of Toll-like receptor adaptor MAL/TIRAP reveals the molecular basis for signal transduction and disease protection. Proc Natl Acad Sci USA 108:14879–14884. 23. Watters TM, Kenny EF, O'Neill LAJ (2007) Structure, function and regulation of the Toll/IL-1 receptor adaptor proteins. Immunol. Cell Biol. 85:411–419. 24. Kawahara K, Tsukano H, Watanabe H, Lindner B, Matsuura M (2002) Modification of the structure and activity of lipid A in Yersinia pestis lipopolysaccharide by growth temperature. Infect Immun 70:4092–4098. 25. Nigou J, Zelle-Rieser C, Gilleron M, Thurnher M, Puzo G (2001) Mannosylated lipoarabinomannans inhibit IL-12 production by human dendritic cells: evidence for a negative signal delivered through the mannose receptor. J Immunol 166:7477–7485. 26. Stack J, Haga IR, Schröder M, Bartlett NW, Maloney G, Reading PC, Fitzgerald KA, Smith GL, Bowie AG (2005) Vaccinia virus protein A46R targets multiple Toll-like-interleukin-1 receptor adaptors and contributes to virulence. J Exp Med 201:1007–1018. 27. Bowie A, Kiss-Toth E, Symons JA, Smith GL, Dower SK, O'Neill LA (2000) A46R and A52R from vaccinia virus are antagonists of host IL-1 and toll-like receptor signaling. Proc Natl Acad Sci USA 97:10162–10167. 28. Harte MT, Haga IR, Maloney G, Gray P, Reading PC, Bartlett NW, Smith GL, Bowie A, O'Neill LAJ (2003) The poxvirus protein A52R targets Toll-like receptor signaling complexes to suppress host defense. J Exp Med 197:343– 351. 29. Spear AM, Loman NJ, Atkins HS, Pallen MJ (2009) Microbial TIR domains: not necessarily agents of subversion? Trends Microbiol 17:393–398. 30. Lang T, Lo C, Skinner N, Locarnini S, Visvanathan K, Mansell A (2011) The Hepatitis B e antigen (HBeAg) targets and suppresses activation of the Tolllike receptor signaling pathway. J Hepatol doi:10.1016/j.jhep.2010.12.042. 31. Ahmad H, Gubbels R, Ehlers E, Meyer F, Waterbury T, Lin R, Zhang L (2011) Kaposi sarcoma-associated herpesvirus degrades cellular Toll-interleukin-1 receptor domain-containing adaptor-inducing beta-interferon (TRIF). J Biol Chem 286:7865–7872. 32. Newman RM, Salunkhe P, Godzik A, Reed JC (2006) Identification and characterization of a novel bacterial virulence factor that shares homology with mammalian Toll/interleukin-1 receptor family proteins. Infect Immun 74:594– 601. 20 33. Low LY, Mukasa T, Reed JC, Pascual J (2007) Characterization of a TIR-like protein from Paracoccus denitrificans. Biochem Biophys Res Comm 356:481– 486. 34. Cirl C, Wieser A, Yadav M, Duerr S, Schubert S, Fischer H, Stappert D, Wantia N, Rodriguez N, Wagner H, et al. (2008) Subversion of Toll-like receptor signaling by a unique family of bacterial Toll/interleukin-1 receptor domain-containing proteins. Nat Med 14:399–406. 35. Zhang Q, Zmasek CM, Cai X, Godzik A (2011) TIR domain-containing adaptor SARM is a late addition to the ongoing microbe–host dialog. Develop Comp Immunol 35:461–468. 36. Radhakrishnan GK, Yu Q, Harms JS, Splitter GA (2009) Brucella TIR Domain-containing Protein Mimics Properties of the Toll-like Receptor Adaptor Protein TIRAP. J Biol Chem 284:9892–9898. 37. Yadav M, Zhang J, Fischer H, Huang W, Lutay N, Cirl C, Lum J, Miethke T, Svanborg C (2010) Inhibition of TIR domain signaling by TcpC: MyD88dependent and independent effects on Escherichia coli virulence. PLoS Pathog 6:e1001120. 38. Sengupta D, Koblansky A, Gaines J, Brown T, West AP, Zhang D, Nishikawa T, Park S-G, Roop RM, Ghosh S (2010) Subversion of innate immune responses by Brucella through the targeted degradation of the TLR signaling adapter, MAL. J Immunol 184:956–964. 39. Salcedo SP, Marchesini MI, Lelouard H, Fugier E, Jolly G, Balor S, Muller A, Lapaque N, Demaria O, Alexopoulou L, et al. (2008) Brucella control of dendritic cell maturation is dependent on the TIR-containing protein Btp1. PLoS Pathog 4:e21. 40. Spear AM, Rana R, Jenner DC, Flick-Smith HC, Oyston PCF, Simpson P, Matthews S, Byrne B, Atkins HS (2012) A TIR domain protein from Yersinia pestis interacts with mammalian IL-1/TLR pathways but does not play a central role in the virulence of Y. pestis in a mouse model of bubonic plague. Microbiology 158:1593-606. 41. Zhang Y, Ting AT, Marcu KB, Bliska JB (2005) Inhibition of MAPK and NFkappa B pathways is necessary for rapid apoptosis in macrophages infected with Yersinia. J Immunol 174:7939–7949. 42. Chan SL, Low LY, Hsu S, Li S, Liu T, Santelli E, Le Negrate G, Reed JC, Woods VL, Pascual J (2009) Molecular mimicry in innate immunity: crystal structure of a bacterial TIR domain. J Biol Chem 284:21386–21392. 43. Radhakrishnan GK, Splitter GA (2010) Biochemical and functional analysis of TIR domain containing protein from Brucella melitensis. Biochem Biophys Res Comm 397:59–63. 44. Dunne A, Ejdeback M, Ludidi PL, O'Neill LAJ, Gay NJ (2003) Structural complementarity of Toll/interleukin-1 receptor domains in Toll-like receptors 21 and the adaptors Mal and MyD88. J Biol Chem 278:41443–41451. 45. Rana RR, Simpson P, Zhang M, Jennions M, Ukegbu C, Spear AM, Alguel Y, Matthews SJ, Atkins HS, Byrne B (2011) Yersinia pestis TIR-domain protein forms dimers that interact with the human adaptor protein MyD88. Microb Pathog 51:89–95. 46. Radhakrishnan G, Harms J, Splitter G (2011) Modulation of microtubule dynamics by a TIR domain protein from the intracellular pathogen, Brucella melitensis. Biochem J 439:79-83. 47. Zheng Y, Lilo S, Brodsky IE, Zhang Y, Medzhitov R, Marcu KB, Bliska JB (2011) A Yersinia effector with enhanced inhibitory activity on the NF-κB pathway activates the NLRP3/ASC/caspase-1 inflammasome in macrophages. PLoS Pathog 7:e1002026. 48. Beutler B (2004) Inferences, questions and possibilities in Toll-like receptor signalling. Nature 430:257–263. 49. Ngo VN, Young RM, Schmitz R, Jhavar S, Xiao W, Lim K-H, Kohlhammer H, Xu W, Yang Y, Zhao H, et al. (2011) Oncogenically active MYD88 mutations in human lymphoma. Nature 470:115–119. 50. Lysakova-Devine T, Keogh B, Harrington B, Nagpal K, Halle A, Golenbock DT, Monie T, Bowie AG (2010) Viral inhibitory peptide of TLR4, a peptide derived from vaccinia protein A46, specifically inhibits TLR4 by directly targeting MyD88 adaptor-like and TRIF-related adaptor molecule. J Immunol 185:4261–4271. 51. Toshchakov VY, Fenton MJ, Vogel SN (2007) Cutting Edge: Differential inhibition of TLR signaling pathways by cell-permeable peptides representing BB loops of TLRs. J Immunol 178:2655–2660. 52. Chan SL, Mukasa T, Santelli E, Low LY, Pascual J. (2010). The crystal structure of a TIR domain from Arabidopsis thaliana reveals a conserved helical region unique to plants. Protein Science, 19:155–161. 53. Bernoux M, Ve T, Williams S, Warren C, Hatters D, Valkov E, Zhang, X., et al. (2011). Structural and functional analysis of a plant resistance protein TIR domain reveals interfaces for self-association, signaling, and autoregulation. Cell Host Microbe 9:200–211. Figure Legends 22 Figure 1 Overview of TLR/ IL-1R signalling through TIR domain containing adaptors The receptors IL-1R, TLR1, TLR2, TLR4, TLR5 and TLR6 are expressed on the cell surface while receptors TLR3, TLR7, TLR8 and TLR9 are expressed on endosomal membranes. The cytoplasmic TIR domain containing adaptors MyD88, Mal, TRIF and TRAM are differentially recruited by TLR/ IL-1R complexes to positively regulate the activation of transcription factors NF-κB and IRFs while SARM negatively regulates TRIF. The evidence so far indicates that bacterial TIR proteins can also act as negative regulators through interaction with MyD88, MAL and the TIR domain of TLR4 (indicated by the white asterisks; see main text for more details). However the interaction profile differs for individual bacterial TIR domains. Figure 2 Primary sequence alignment of a range of bacterial TIR domains with some mammalian TIR domains of known structure. The regions corresponding to the TIR motifs, Box1, 2 and 3, are indicated by the solid rectangles above the alignment. The regions of the sequence of TLR1-TIR corresponding to secondary structure elements as determined by X-ray crystallographic analysis (Pdb accession code: 1FYV) are shown below the alignment. Some of the residues involved in dimer formation are shown in bold for both the TIR domain of TLR10 and PdTIR. The alignment was generated using ClustalW. Figure 3 Structure of a) the TIR domain of TLR1 (Pdb accession code, 1FYV) and b) PdTIR (Pdb accession code, 3H16). The positions of the BB (red), DD (green) and EE (cyan) loops with key roles in dimer formation are indicated. c) Superposition of the TIR domain of TLR1 (dark blue) and PdTIR (magenta). Space-filling model of the structure of the dimer of d) TIR domain of TLR10 (Pdb accession code, 2J67) and e) PdTIR. In each case monomer 1 is shown in dark blue with the region forming the 23 interaction in red while monomer 2 is shown in cyan with the regions forming the interaction in gold. Some of the key residues involved in dimer formation are individually labeled. In d) the residues indicated all form part of the BB loop while in e) the residues are part of the DD and EE loops as indicated in a) and b). See also Figure 2 for more details. Figure 1 24 Figure 2 25 Figure 3 26 27