Bilirubin 1
advertisement
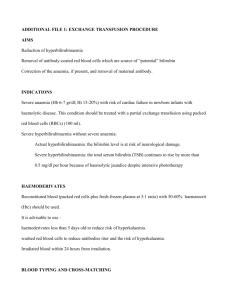
Bilirubin, Total and Direct Bilirubin metabolism can be considered in terms of the following stages: pre-hepatic stage hepatic stage post-hepatic stage Pre-hepatic stage Eighty percent of all bilirubin is derived from the metabolism of haemoglobin released from senescent red blood cells and any compound containing a haem nucleus may be a precursor e.g. catalase, myoglobin.Haemoglobin released from red blood cells is converted to unconjugated (indirect) bilirubin in the reticuloendothelial system. o o o Daily production of unconjugated bilirubin is 250 to 350 mg. Because this bilirubin is water insoluble, it must be transported to the liver bound to albumin. The circulating half-life of unconjugated bilirubin is <5 minutes. If not taken up by the liver or if produced in excess, unconjugated bilirubin is deposited in extrahepatic tissues. This results in pre-hepatic jaundice. Pre-hepatic jaundice is the consequence of inability of the liver to handle an increased bilirubin load. The limiting factor is the saturation of the enzyme glucuronyl transferase. Hepatic stage In the liver, unconjugated bilirubin is transferred from albumin into hepatocytes where it is conjugated with glucuronic acid. Conjugated bilirubin (direct) is then excreted in the bile and transported to the intestine. Conjugated bilirubin is essentially absent from the blood of healthy individuals. Hepatic jaundice is caused by damage or disease in the liver. Heme enters the liver but it does not take out as much bilirubin as is normal. Bilirubin builds up in the blood and spills over into the kidneys which filter it out into the urine. The amount of urobilinogen in the urine will be either normal or low if not enough bilirubin is being removed by the liver into bile and the intestines. Post-hepatic stage In the distal ileum and colon, bacteria covert conjugated bilirubin to stercobilinogen. A small fraction is reabsorbed into the portal circulation and excreted in the urine as urobilinogen. This metabolic pathway accounts for the bilirubin detected in the plasma of healthy individuals. If bilirubin cannot reach the intestinal area because of a blockage in the bile duct, than bilirubin builds up in the blood because it cannot get out of the liver. Bilirubin is then removed by the kidneys into the urine. Little if any, urobilinogen will be found in the urine since little or no bilirubin is reaching the intestines. Jaundice is the clinical manifestation of an elevated plasma bilirubin level. It occurs when bilirubin production exceeds the liver's excretory capacity. This may occur because (1) Too much bilirubin is being produced eg. Haemolytic anaemia (2) Hepatocytes are injured and cannot metabolize or excrete bilirubin eg. Acute viral hepatitis (3) The biliary tract is obstructed blocking the flow of conjugated bilirubin into the intestine. E.g. obstructive biliary tract disease Unconjugated bilirubin Unconjugated Bilirubin is insoluble in water. It is not found in tears or Saliva. Unconjugated Bilirubin cannot be excreted by kidney. It concentrates in high albumin containing tissues. Skin (especially face and trunk): Jaundice Sclera: Scleral Icterus Haemolysis- Haemolytic Anaemia (mild Hyperbilirubinemia)Causes: malaria,sickle cell crisis, spherocytosis,thalassemia,glucose-6-phosphate dehydrogenasedeficiency (G6PD),drugs or other toxins, and autoimmune disorders. Other possibilities include ineffective erythropoiesis, resorption of a large hematoma, pulmonary embolism with infarction, Crigler-Najjar syndrome, neonatal jaundice, and shunts. Gilbert syndrome affects ~5% of the population and causes mild hyperbilirubinemia because of impaired UDP-glucuronyltransferase. Because unconjugated bilirubin is water insoluble and bound to albumin, these patients do not have bilirubinuria. Testing of urine for bilirubin is a simple way to determine if elevated bilirubin is unconjugated or conjugated. Increases in conjugated bilirubin are highly specific for disease of the liver or bile ducts. Hepatocellular injury or cholestasis is suspected when more than 50% of total bilirubin is conjugated bilirubin (direct: total ratio > 0.4). Increased Conjugated Bilirubin: Adults Intrahepatic Causes Hepatocellular disease -Viral Hepatitis, Alcoholic Liver Disease, Biliary Tract Obstruction- Drug induced cholestasis, Prolonged Total Parenteral Nutrition, Sarcoidosis, Pregnancy, Primary Biliary Cirrhosis, Primary Sclerosing Cholangitis Extrahepatic Causes –Cholelithiasis, Pancreatitis, Cryptosporidium infection (immunocompromised patient), Cytomegalovirus infection, Cholangiocarcinoma, Pancreatic Cancer. Increased Conjugated Bilirubin: Neonatal Patients o Sepsis, Intrauterine viral infections o Neonatal hepatitis o Biliary tract obstruction - Intrahepatic and extrahepatic biliary atresia, Choledochal cyst, Annular pancreas, Trisomy 18, , Galactosemia, Tyrosinemia, o Hereditary - Dubin-Johnson Syndrome, Rotor's syndrome , Hypermethioninemia, Alpha-1 antitrypsin deficiency, Cystic Fibrosis o Following Hemolytic Disease of the Newborn syndrome Hypopituitarism Hypothyroidism In common bile duct obstruction due to gallstones, total bilirubin seldom exceeds 15 mg/dL and usually remains below 6 mg/dL because obstruction is often incomplete and conjugated bilirubin is water soluble and excreted by the kidneys. Bilirubin excretion is able to keep pace with production. Total bilirubin levels >25 mg/dL usually indicate intrahepatic cholestasis. The following table may help to differentiate the various causes of jaundice. Lab Test Hemolysis Hepatocellular Intrahepatic cholestasis Extrahepatic cholestasis Total bilirubin <6 mg/dL Variable Variable, may be >30 mg/dL <30 mg/dL Direct bilirubin <20% >50% >50% >50% ALT Normal >5 fold increase 2-5 fold increase 2-3 fold increase cholangitis higher ALP Normal 2-3 fold increase 3-5 fold increase 3-5 fold increase PT Normal Prolonged Prolonged Prolonged PT corrected by vitamin K Not Done No Variable Yes Hepatitis in adults, jaundice develops in 70% of cases of acute hepatitis A, 33 - 50% of cases of acute hepatitis B and 20 - 33% of cases of acute hepatitis C. Peak bilirubin is usually < 15 mg/dL in viral hepatitis; Bilirubin peaks a week later than ALT and AST and then gradually decreases. In adults with viral hepatitis, bilirubin remains increased for 30 +/- 20 days after peak concentrations are reached. In approximately one third of adults with hepatitis B virus infections, jaundice remains elevated more than 6 weeks. Significantly elevated bilirubin is uncommon in toxic and ischemic hepatic injury. In the full-term infant, serum bilirubin levels peak at 48 to 72 hours after birth. Major risk factors for hyperbilirubinemia in full-term newborns include: Jaundice within first 24 hours after birth A sibling who was jaundiced as a neonate ABO or Rh incompatibility Nonoptimal nursing G6PD deficiency Infection Cephalo-hematoma or bruising East Asian or Mediterranean descent How to investigate an isolated case of slightly raised bilirubin in an asymptomatic adult? Values up to 20% above ULN are likely to be statistical rather than clinical abnormals. Values <1.5 times ULN: interval retest in 1–3 months unless clinical suspicion of disease. Values >1.5 ULN: confirm proportion of indirect (unconjugated) bilirubin. If >70%, unconjugated, probable Gilbert syndrome: no further testing needed if non‐progressive on interval retesting, unless haemolysis is clinically suspected. If rising on restesting, consider haemolysis and test haptoglobin, lactate dehydrogenase and blood count with reticulocyte count. Values >3 times ULN: clinical disease probable, further investigation required. Consider ultrasound (conjugated >50%) or haemolysis (unconjugated >70%). Reference range is 0 to 1.1 mg/dL for total and 0.0 to 0.3 mg/dL for direct bilirubin. Specimens should be protected from light and analyzed as soon aspossible; grossly hemolyzed specimens should be rejected because hemoglobin inhibits the diazo reaction and falsely low results may be seen. Bilirubin levels are 33% lower beginning with the second trimester of pregnancy. The specimen should be protected from light, because unconjugated bilirubin is unstable. One hour of light exposure can cause a 50% decrease. Reference Paul D. Berk, Robert B. Howe, Joseph R. Bloomer, Nathaniel I. Berlin Studies of bilirubin kinetics in normal adults Published in Volume 48, Issue 11 J Clin Invest. 1969; 48(11):2176–2190 Tietz Textbook of Clinical Chemistry, Second edition. Edited by CA Burtis, ER Ashwood. Philadelphia, WB Saunders Company, 1994 Scharschmidt BF, Blanckaert N, Farina FA, et al: Measurement of serum bilirubin and its mono- and diconjugates: Applications to patients with hepatobiliary disease. Gut 1982;23:643-649 DAVID E. JOHNSTON, M.D. Special Considerations in Interpreting Liver Function Tests AAFP April 15 1999 2223-2233 D. Robert Dufour,John A. Lott, Frederick S. Nolte,David R. Gretch,Raymond S. Koff,and Leonard B. Seeff Diagnosis and Monitoring of Hepatic Injury. I. Performance Characteristics of Laboratory Tests Clinical Chemistry 46:12 2027–2049 (2000) American Gastroenterological Association Medical position statement: evaluation of liver chemistry tests. Gastroenterology 2002. 1231364–1366 Useful for Assessing liver function Evaluating a wide range of diseases affecting the production, uptake, storage, metabolism, or excretion of bilirubin Monitoring the efficacy of neonatal phototherapy