the diabetes hub - Mangere Community Health Trust
advertisement
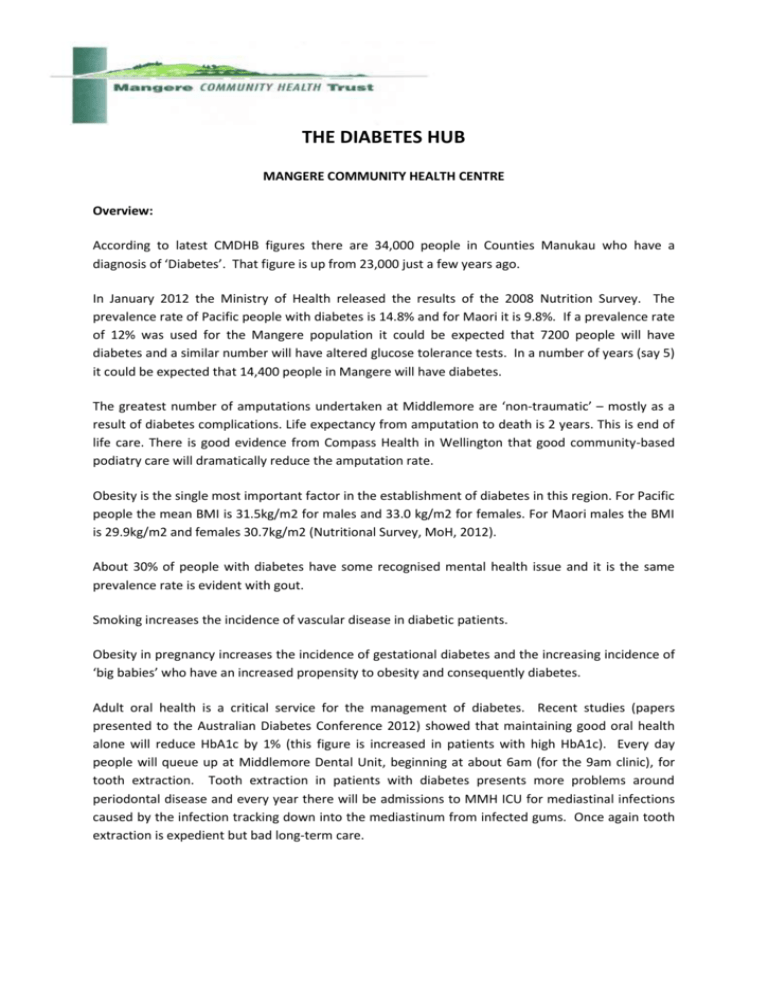
THE DIABETES HUB MANGERE COMMUNITY HEALTH CENTRE Overview: According to latest CMDHB figures there are 34,000 people in Counties Manukau who have a diagnosis of ‘Diabetes’. That figure is up from 23,000 just a few years ago. In January 2012 the Ministry of Health released the results of the 2008 Nutrition Survey. The prevalence rate of Pacific people with diabetes is 14.8% and for Maori it is 9.8%. If a prevalence rate of 12% was used for the Mangere population it could be expected that 7200 people will have diabetes and a similar number will have altered glucose tolerance tests. In a number of years (say 5) it could be expected that 14,400 people in Mangere will have diabetes. The greatest number of amputations undertaken at Middlemore are ‘non-traumatic’ – mostly as a result of diabetes complications. Life expectancy from amputation to death is 2 years. This is end of life care. There is good evidence from Compass Health in Wellington that good community-based podiatry care will dramatically reduce the amputation rate. Obesity is the single most important factor in the establishment of diabetes in this region. For Pacific people the mean BMI is 31.5kg/m2 for males and 33.0 kg/m2 for females. For Maori males the BMI is 29.9kg/m2 and females 30.7kg/m2 (Nutritional Survey, MoH, 2012). About 30% of people with diabetes have some recognised mental health issue and it is the same prevalence rate is evident with gout. Smoking increases the incidence of vascular disease in diabetic patients. Obesity in pregnancy increases the incidence of gestational diabetes and the increasing incidence of ‘big babies’ who have an increased propensity to obesity and consequently diabetes. Adult oral health is a critical service for the management of diabetes. Recent studies (papers presented to the Australian Diabetes Conference 2012) showed that maintaining good oral health alone will reduce HbA1c by 1% (this figure is increased in patients with high HbA1c). Every day people will queue up at Middlemore Dental Unit, beginning at about 6am (for the 9am clinic), for tooth extraction. Tooth extraction in patients with diabetes presents more problems around periodontal disease and every year there will be admissions to MMH ICU for mediastinal infections caused by the infection tracking down into the mediastinum from infected gums. Once again tooth extraction is expedient but bad long-term care. The very clear message from the Ministry of Health is ‘Clinical integration’. The Mangere Diabetes Hub is providing clinical integration for people with diabetes. Shortly there will be a single shared clinical note system across all providers. Diabetes Eye Clinic: The retinal screening (photography) service operates in a standalone contract with CMDHB. This is a mobile service and extends across the Counties Manukau area however its 'home' is at the Diabetes Hub. The service is provided on referral from general practice (usually, however referrals accepted from all sources such as, optometrist, diabetes nurse, and SMO clinics). Referrals are triaged by CMDHB and allocated to the most appropriate clinic (one of two clinics) for retinal review. Last year 12,500 people were screened by the service. There is an issue in that not all the 34,000 people who have diabetes in the CMDHB area are being referred. This needs to improve if eye health is to improve. Particularly in low socio-economic communities the screening service picks up a full range eye disease the most common incidental findings are glaucoma, hypertensive retinal disease, emboli, vein occlusions, pterygia and cataract. Consultant SMO Ophthalmology clinics began in February 2013, these are at least 2 clinics weekly, in some weeks there are up to 4 clinics operating. The clinics are operated by CMDHB SMO and technical staff with equipment provided by MCHT. The initial phase of the clinic is to conduct clinical examinations for Mangere patients, in the local setting, and who are on an expired planned appointment at MSC. Podiatry service: The Community ‘Foot Clinic’ Podiatry Service has been established to maintain or improve the foot health status of patients with diabetic foot-related pathologies. The service is accessible to patients within the Mangere catchment and enrolled with a local general practitioner. The aims of the service are to: Reduce the number of lower limb amputations within the Counties Manukau district. Decrease hospital admissions for foot-related complications associated with diabetes Identify and educating High Risk patients Provide a comprehensive assessment service Provide a free, appropriate and accessible service for Diabetic patients within the Mangere area Initiate preventive measures when necessary Provide podiatric management as appropriate Educate health professionals, patients, whanau, and members of the community in aspects of podiatry and diabetic foot pathology. The ‘Foot Clinic’ service is free to all diagnosed diabetic patients who meet the referral criteria and who are not currently in a hospital podiatry treatment programme. The Community Podiatry Service offers an initial assessment/screening to all patients that meet the referral criteria. Following the initial assessment, the service may: Refer on to hospital-based care, Recall the patient for a course of treatment, Manage the patients as set out by the New Zealand guidelines for diabetic foot screening. All patients seen within the service have a summary of their visit sent to the initial referrer and/or primary care provider to ensure continuity of care. Many of the PHO’s within the Mangere area have had Podiatry services offered in-house to manage their Diabetic populations in the past. However a change to the funding structure has meant that these services are no longer available within many PHO/Primary Care settings or the frequency of the service has reduced to once a month or once every second month, this is a significant limitation for many patients in Mangere The diabetes foot clinic runs 5 days a week with regular evening and Saturday clinics. It is currently staffed by 1.2 FTE podiatrists. This community clinic has strong links with the hospital service at MSC, with the community podiatrist attending the podiatry meetings with the consultants at MSC (ours are the only community podiatrists to do so). Copy of the Annual report is attached, along with some snapshots of the community feet first presentation given to some local GP clinical networks. Dietetics: The Healthy Kai clinic runs 5 days a week with regular evening and Saturday clinics. It is currently staffed by 2 Dieticians to provide 1.0 FTE. The focus groups for this clinic are all patients with diabetes and expectant mums who are obese. Access to this service is via referral from GP/Nurse, Diabetes Team referrals or selfreferrals. The DHB KPI’s set for these services are not especially helpful as they look specifically at weight (kg) reduction by patient per month. Weight reduction is a long term goal and should be measured over a number of months not just 4 weeks. Research is now suggesting that success may also be defined as preventing weight gain. Weight is not the entire focus of the clinic, more importantly we need to look at better management of diabetes, compliance with medication and physical activity as indicators of success. Some of the case studies from January cohort of patients identify the variety of patients seen and the complications faced by the dietetic team. Having been operating now for 12 months the service is seeing and referring to the hospital renal a number of patients who were completely unaware of their impaired renal function and who were clearly (given the medication lists) not being actively managed for significant renal impairment. January 2013 Case Studies - Some typical patient stories from the dietitians Non-compliant or not enough attention??? 1. Large Samoan man (2 prior DNAs), had stopped taking meds, HbA1c up to 111. Friends advice and cultural beliefs led him to believe that the government benefitted ($) from people taking meds and had stopped taking his. (Also his mother had dark skin pigment upon death which family attributed to meds, reinforcing his decision?!) Dietitian spent time to explain what DM is, how meds work and the importance of taking them – to which the patient responded, “my friends have been telling me bull**** (lies)”. Once this issue was resolved, he was happy to take on board and commit to further nutrition changes/advice to improve blood glucose. Also avoided meat due to pain in knees (gout) and Dn addressed this as well. He finished the session extremely thankful & responsive to dietitian. This took 90mins (but we often have the time to spend with people to get it right). 2. Maori woman, single mother of one son, unemployed and looking for work – feeling low at times. Recently stopped meds as she thought they were causing hay fever & headaches. Further investigation showed that she had not been taking meds with food (and often 3-4 hours outside of meals times). Attitude was “I missed today so might as well miss tomorrow too”. The Dietician’s approach was to overview Diabetes & meds, and also focus on better food choices/ strategies on days that she felt low. Corrected misconception that healthy foods are expensive or take a long time (or skills) to prepare. Pt left apologising for missing a prior appointment. 3. Older Samoan man: limited English, 2 prior DNAs, poor HbA1c. Attended with wife & daughter. Pt took no ownership of his own diabetes (he felt fine, had regular meals & PA, was not overweight & didn’t see it was an issue for him). Dietician could see visible evidence of deterioration in eyes and cued eye & pod checks. Patient acknowledged changes in these areas and once he understood the relationship, he fully engaged in the appointment. Nutrition input was focused around role of CHO, portions and healthy plate model – with food models used extensively. (The pt was required to bring in his passport to receive eye and pod input – and he went home and brought it back within 30mins!) Success stories 4. 40+ Maori male, first seen July 2012, with regular input for weight loss. In addition to large portions, regular snacks and binge eating episodes, pt also ate extreme amounts of ‘good’ foods (6-8 eggs/ 3-4c milk/day). We worked through these ideas, increasing fibre intake and satiety, and then decreasing between meal snacks, leading towards three regular meals daily with wider variety, decreased carbohydrate and increased vegetables. We’ve had the time for him to trust me – and he has lost 14kg in past 7 months – and is starting to accept that he is building new habits for the rest of his life. 5. Tongan woman, 28/40 gestation (5th pregnancy) and 24kg weight gain. Ate three large meals daily – lots of meat & carbohydrate but insufficient vegetables. Also enjoyed biscuits, chips, ice-cream, and fruit between meals and drank 3-4c juice and 1c fizzy daily (i.e. 30-40tsp sugar/day!) Pt was amazed by this and very motivated to make changes for whole family and continue to review after baby born. Recommendations included drinking water, smaller portions, nutritious snacks between meals (if any) and 30mins PA most days. 6. 70yr+ Maori man, seen in Oct 2012 for II DM and high cholesterol (Chol 7.0mmol/L, TG 3.4, HDL 1.17, LDL 4.3, Ratio 6.0). Worked as a driver, snacked a lot, eating lots of seafood, pies and other high salt/fat/sugar foods. Advised to eat regular meals, choose high fibre carbohydrates at each and limit portion sizes – esp. shellfish and animal fats. Reviewed in January and significant improvement in cholesterol as a result of following advice; Lipids: TC 4.1mmo/L, HDL 1.12, LDL 1.9, TG 2.4, and Ratio 3.7. Our most common issues & conversations in the Healthy Kai Clinic Background & understanding; what is diabetes, SMOBG, compliance & function of meds, challenges in managing DM??? Regular meals – including importance of high fibre (low GI) carbohydrates at each meal (and avoid snacks where practical). Portion sizes; healthy plate – a fist, a palm and half a plate! Fizzy drinks, fruit juice & drinks (Raro, etc). Physical activity; 30-60mins moderate PA on most days of the week! Smoking cessation service: This a separate contract held with the Ministry of Health. There are 3.5FTE quit coaches and they cover all of CMDHB with a focus on the pregnant women and their whanau. They also support families who have small children or patients with a chronic illness. The service is offered onsite, however predominantly the patients are seen off-site at their homes. NRT is delivered directly to the patients attempting to quit, we do not provide the quit card which needs to be taken to a pharmacy. All quit coaches are fully qualified to dispense NRT. Mental Health Service: A range of diagnoses are managed by a Samoan Mental Health Nurse. She interacts with patients both onsite and at a place which is comfortable for them (usually home). Patients are referred by GPs or via CMDHB mental health services. The mental health nurse spends a lot of time ensuring adherence to medication – both for their mental health disorder and diabetes. Midwifery service: MMH Community Midwives operate clinics on Tuesdays and Fridays. The diabetes midwife clinic operates on a Wednesday afternoon. Midwives take advantage of the onsite smoking cessation and dietetics services. Oral health service: Oral health is vital to the good glycaemic management of the diabetic patient. Periodontal disease is now being called the 6th complication of diabetes. Current service models do not include oral health as a prerequisite of good diabetic care (i.e. within CCM – primary care must report on Eye and foot check dates only). Additionally, the oral care provided in this community is a fee-for-service – i.e. the patient must pay. In a low socio economic area this creates a barrier to good health. The Mangere Diabetes Hub is the only clinically integrated diabetes service in New Zealand. Appendix 1. MCHT Podiatry mini casestudies 12.pdf