Size: 184 kB Oct 9th 2014 UCSD Ebola Management Plan Draft
advertisement
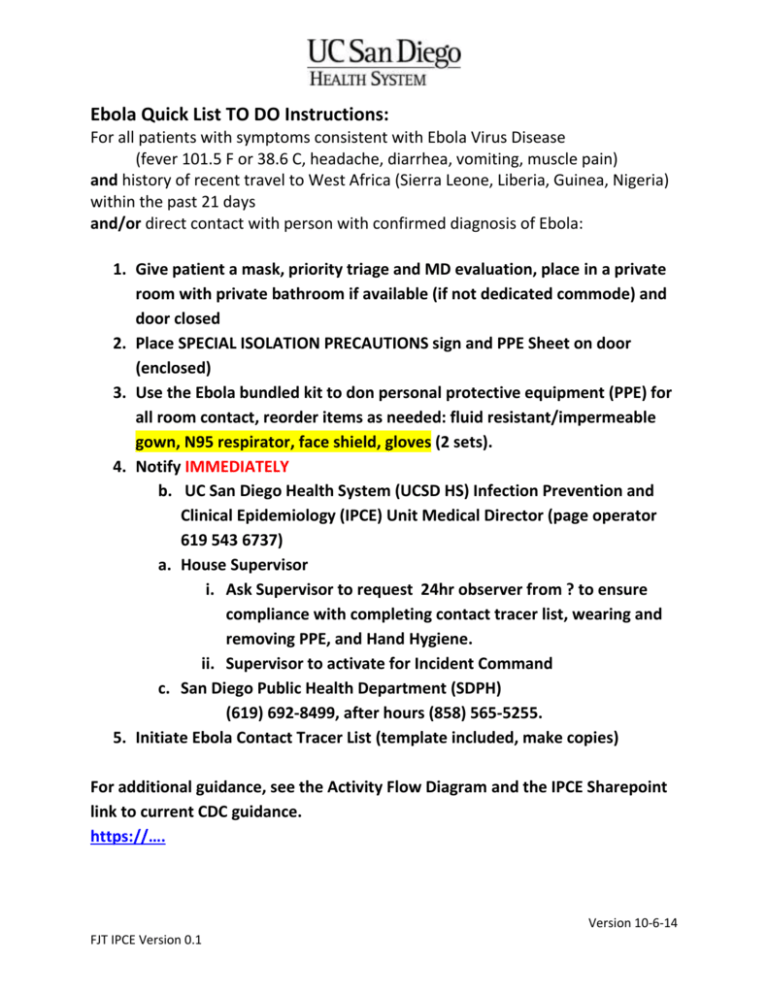
Ebola Quick List TO DO Instructions: For all patients with symptoms consistent with Ebola Virus Disease (fever 101.5 F or 38.6 C, headache, diarrhea, vomiting, muscle pain) and history of recent travel to West Africa (Sierra Leone, Liberia, Guinea, Nigeria) within the past 21 days and/or direct contact with person with confirmed diagnosis of Ebola: 1. Give patient a mask, priority triage and MD evaluation, place in a private room with private bathroom if available (if not dedicated commode) and door closed 2. Place SPECIAL ISOLATION PRECAUTIONS sign and PPE Sheet on door (enclosed) 3. Use the Ebola bundled kit to don personal protective equipment (PPE) for all room contact, reorder items as needed: fluid resistant/impermeable gown, N95 respirator, face shield, gloves (2 sets). 4. Notify IMMEDIATELY b. UC San Diego Health System (UCSD HS) Infection Prevention and Clinical Epidemiology (IPCE) Unit Medical Director (page operator 619 543 6737) a. House Supervisor i. Ask Supervisor to request 24hr observer from ? to ensure compliance with completing contact tracer list, wearing and removing PPE, and Hand Hygiene. ii. Supervisor to activate for Incident Command c. San Diego Public Health Department (SDPH) (619) 692-8499, after hours (858) 565-5255. 5. Initiate Ebola Contact Tracer List (template included, make copies) For additional guidance, see the Activity Flow Diagram and the IPCE Sharepoint link to current CDC guidance. https://…. Version 10-6-14 FJT IPCE Version 0.1 Ebola Kit Contents: 1. Ebola Information Packet (UCSD reprographic ?) a. Ebola Quick List To Do Instructions (this document) b. CDC Ebola fact sheet c. PPE Guidance Sheet (Post at room entrance) d. SPECIAL ISOLATION PRECAUTIONS sign (Post at room entrance) e. Ebola Activity Flow diagram f. Ebola Contact Tracer TEMPLATE (Please make copies) g. Ebola Fever Monitor Form TEMPLATE (Please make copies) h. Ebola Lab testing Guidance Sheet i. Ebola Cleaning, handling of trash and linen Guidance Sheet j. Ebola Patient Placement Guidance Sheet k. Ebola Patient Transport Guidance Sheet 2. Initial set of disposable PPE, UCSD Reorder guide below: 1 ??? N-95 Respirator Mask 2 ??? Full face shield with eye protection 3 ??? Regular nitrile gloves, all sizes, 2 sets of each 4 ??? Impermeable gown, 2 sets 5 ??? Knee length booties 6 ???? Biohazard Trash Bag, red 7 ????? Specimen transport Biohazard bag 8 Version 10-6-14 FJT IPCE Version 0.1 Personal Protective Equipment (PPE) Use for Ebola patient: All persons entering the patient room must wear: Leg/shoe covers UCSD Reorder ???? Knee-length booties Gown Fluid Resistant/Impermeable UCSD Reorder ??? Respirator N95 UCSD Reorder ??? Eye/face protection UCSD Reorder Full face shield with eye protection Gloves UCSD Reorder ???? Regular nitrile gloves, all sizes Removing (Remove IN the Patient’s Room Donning (Don OUTSIDE the Patient Room) or Anteroom when available) o o o o o 1. Clean and Dry hands 1. Remove 1st pair of Gloves 2. Leg/Shoe Covers (under the Gown) IF INDICATED: BLOOD/STOOL/VOMIT on Floor 3. Impermeable Gown 2. 3. Face Shield Gown and 2nd pair of gloves. Hand hygiene. 4. If Leg/Shoe covers used remove and 2nd pair of gloves. Hand hygiene. 4. N95 Respirator 5. N95 Respirator 6. Clean hands 5. Full Face Shield 7. Dispose of all PPE in biohazard waste 6. 2 sets of gloves to cover sleeve’s cuffs Version 10-6-14 FJT IPCE Version 0.1 PPE must be carefully removed without contaminating one’s eyes, mucous membranes, or clothing with potentially infectious materials, and must be discarded in a biohazard red trash bag/can. Hand hygiene must be performed immediately after removal of PPE.If at anytime you believe you have contaminated your hands, hand hygiene is recommended prior to the next step. STOP (Assigned/Dedicated Personnel Only) Gown, Impermeable N95 Respirator Full Face shield Gloves, 2 pairs Shoe/Leg covers (if Version 10-6-14 FJT IPCE Version 0.1 stool/blood/vomit on floor) Door closed Suspect Ebola Patient Contact Tracer Name of Contact Observer:______________________________________________ Any person entering patient room must be listed below, list names once per day. Date and Print Full Name clearly Type of Service/Department Time contact: MD/RN/Visitor, etc. Version 10-6-14 FJT IPCE Version 0.1 Staff Ebola Exposure 21 day Fever Monitor Any person with unprotected exposure to a confirmed Ebola patient must monitor their fever twice a day for 21 days. If temperature is 99.0°F or above identified, staff should contact Occupational Health (858) 6571604 Staff: Return form to Occupational Health when completed Name: Department: Name of index Patient: AM Date/ Time / Temperature Contact Number: ( Date Exposed: ) PM Date/ Time / Temperature 1 2 3 4 5 6 7 8 9 10 11 12 Version 10-6-14 FJT IPCE Version 0.1 13 14 15 16 17 18 19 20 21 UC San Diego Health System Clinical Laboratories Enhanced Precautions for Collection, Transport, and Testing of Clinical Specimens from Patients with Suspected Ebola Virus Disease (EVD) Introduction The largest Ebola Virus outbreak in history is currently taking place in West Africa. Ebola is caused by an enveloped RNA virus, which is sensitive to all standard laboratory disinfectants. It can only be spread through direct contact of broken skin or mucous membranes with infectious bodily fluids (blood, urine, feces, saliva, or vomit) from a symptomatic patient. It is not spread by airborne contact like the most infectious viruses such as measles when a patient is asymptomatic. It is less infectious than bloodborne HIV or hepatitis C virus so OSHA bloodborne pathogens precautions will protect laboratory workers. To date, only two health care workers and one patient from Liberia have been hospitalized in the US with no additional spread. General Considerations: Routine clinical diagnostic testing should be limited to the absolute minimum necessary to provide effective and timely treatment to the patient in order to minimize potential exposure of health care workers to blood, body fluids, or other potentially infectious materials. Maintain communication among all members of the treatment team, including laboratory workers, to ensure proper safety measures are taken to protect health care workers and other patients from potential Ebola virus exposure. This includes notification of laboratory staff PRIOR to specimen collection, clear labeling of specimens from patients with suspected EVD, and documentation in hospital and laboratory information systems. Version 10-6-14 FJT IPCE Version 0.1 All health care workers must maintain proper hand hygiene (washing hands with soap and water for at least 20 seconds, or using an approved hand sanitizer). In addition, all health care workers should take measures to cover any cuts, sores, or other breaks in the skin at all times, or limit high-risk activities when these conditions are present. Each laboratory section should perform a risk assessment of individual specimen collection, transport, and testing activities that may pose an increased risk of exposure to laboratory workers, and identify specific modifications of existing policies and procedures to mitigate those risks. UNDER NO CIRCUMSTANCE will testing be performed on any clinical specimen in the UC San Diego Health System Clinical Laboratories to directly diagnose or “rule out” potential EVD. Requests for EVD diagnostic testing will be referred to the San Diego County Public Health Laboratory, which will coordinate specimen collection, packaging, and transport. Specimen Collection and Transport Considerations: Clinical specimens may be safely collected from patients suspected of having EVD by STRICT ADHERENCE to the OSHA standard precautions for bloodborne pathogens. o Wear gloves and a fluid repellent or disposable lab coat or gown. DO NOT touch face, mouth, nose, or eyes with gloved hands. o Wear a full face shield or goggles. ENHANCED PRECAUTIONS: wear a surgical mask or N95 respirator covering the nose and mouth. o Dispose of all gloves and collection materials (wrappers, tubing, etc.) in biohazard (contaminated) waste. Dispose of all sharps in an approved biohazard sharps container. o Wash hands thoroughly with soap and water for at least 20 seconds immediately after removing PPE. For specific Ebola testing, collect a minimum of 4 mL whole blood with EDTA, SPS or citrate in plastic tubes. Wipe each tube with a 10% bleach solution immediately after collection. Place specimens in double biohazard specimen bags and store at 4oC until San Diego County Public Health Service Laboratory personnel arrive. CDC submission forms and a Primary Specimen Contact List will be required. DO NOT split, aliquot, transfer, or otherwise process the specimen. Clinical specimens from patients known or suspected of having EVD may be safely transported by STRICT ADHERENCE to the OSHA standard precautions for bloodborne pathogens. o Transport clinical specimens in individual sealed specimen bags marked with the biohazard symbol with sufficient absorbent material to absorb the entire contents of the specimen. Version 10-6-14 FJT IPCE Version 0.1 ENHANCED PRECAUTIONS: wipe each individual tube with a 10% bleach solution immediately following collection. EHNANCED PRECAUTIONS: double-bag specimens for transport to the appropriate laboratory for testing. UNDER NO CIRCUMSTANCE should clinical specimens from patients with EVD be transported through the pneumatic tube system. o Place bagged specimens inside a hard-sided container for transport in a vehicle or by a commercial shipping company (NOTE: all Federal and international regulations must be followed for clinical specimens shipped commercially). Testing Considerations – General: Routine testing of clinical specimens from patients with suspected or confirmed EVD may be safely performed by STRICT ADHERENCE to the OSHA standard precautions for bloodborne pathogens. o Wear gloves and a fluid repellent or disposable lab coat or gown when handling clinical specimens. DO NOT touch face, mouth, nose, or eyes with gloved hands. ENHANCED PRECAUTIONS: double-glove for high-risk manual procedures, as determined by each laboratory section. o Gloves should be changed frequently to avoid contamination of the laboratory environment and other clinical specimens. Immediately remove PPE that becomes grossly contaminated with blood or other potentially infectious materials and immediately wash hands thoroughly with soap and water for at least 20 seconds. Dispose of contaminated PPE in biohazard waste. o Wear a full face shield or goggles during procedures that may produce splashes or sprays. Acrylic or Plexi-glass splash guards may also be used. ENHANCED PRECAUTIONS: perform tasks that may generate aerosols in a certified Class II biological safety cabinet (BSC). If a BSC is not available, then wear a surgical mask or N95 respirator covering the nose and mouth during procedures that may generate splashes or sprays (e.g. uncapping tubes, vortexing or mixing specimens, pipetting or transferring liquid specimens, etc.), or any other high-risk activity. ENHANCED PRECAUTIONS: use a gauze pad saturated with 10% bleach solution to open any tube or specimen container. ENHANCED PRECAUTIONS: use a certified Class II biological safety cabinet if MANUAL testing is performed on clinical specimens from patients with EVD. o All manufacturer-installed safety features must be in place for instruments used for automated testing of clinical specimens. Department-Specific Testing Considerations: Version 10-6-14 FJT IPCE Version 0.1 Hematology, Coagulation, and Chemistry: testing should be limited to point-of-care testing whenever possible; urinalysis may be limited to manual dipstick testing. Hematology and Microbiology: whole blood smears for malaria, Gram stain, or other microscopic testing should be air dried, fixed in methanol for 30 minutes and allowed to air dry, and fixed on a heat block at 95oC for 1 hour in order to inactivate the specimen. Microbiology: o Bacterial testing of clinical specimens (other than blood cultures) from patients suspected of having EVD should be restricted unless critically necessary for patient care. o Disinfect blood culture bottles with 10% bleach solution upon receipt, and before and after sampling bottles flagged as positive for bacterial growth. DO NOT perform Verigene testing on positive blood cultures from patients with known or suspected EVD. Perform Gram stains and subcultures in the BSC. o Perform centrifugation only inside sealed centrifuge cups. Disinfect the cups after each use with 10% bleach with a contact time of at least 5 minutes, followed by distilled water or 70% ethanol. o Seal all culture plates with tape and place inside labeled biohazard bags prior to incubation. o Perform all culture work-up inside a BSC. Laboratory Disinfection and Waste Disposal Considerations: NOTE: All clinical specimens from patients known to have confirmed EVD or other hemorrhagic fever disease must be destroyed in accordance with Federal regulations. UNDER NO CIRCUMSTANCE WILL ANY CLINICAL MATERIALS FROM A PATIENT WITH CONFIRMED EVD OR OTHER HEMORRHAGIC FEVER DISEASE BE STORED, ARCHIVED, FROZEN, OR OTHERWISE PRESERVED FOR LONG-TERM STORAGE. ENHANCED PRECAUTIONS for disposal of laboratory waste associated with testing clinical specimens from patients suspected of having EVD include: o Wrap all waste (blood tubes, culture plates, etc.) in absorbent pads soaked with fullstrength bleach. o Place wrapped waste in double red bags. o Place red bags in rigid, hard sided container. o Autoclave prior to disposal. REPORT SPILLS/EXPOSURES IMMEDIATELY to a Lead Technologist, Supervisor, or Manager. Isolate the area and alert other staff of the spill in order to limit potential exposure. Wear all necessary PPE (gown, double gloves, goggles or face shield, and surgical mask or N95 respirator). Working from the outside of the spill inward, contain the spill with absorbent material soaked in full-strength bleach until the spill is fully absorbed. Remove absorbent material, and clean the area again with 10% bleach with a contact time of at least 5 Version 10-6-14 FJT IPCE Version 0.1 minutes, followed by distilled water or 70% ethanol. Dispose of cleaning materials and PPE in double red bags and autoclave prior to disposal. Immediately wash hands with soap and water for at least 20 seconds. Decontaminate work areas with a solution of 10% bleach with a contact time of at least 5 minutes, followed by a rinse of distilled water or 70% ethanol. Dispose of all cleaning materials in biohazard waste. Wash hands thoroughly with soap and water for at least 20 seconds before leaving the laboratory. Laboratory workers should maintain awareness of their own health conditions and report any symptoms of fever, headache, nausea, vomiting, or diarrhea to a Supervisor or Manager. Laboratory workers who report these symptoms to a Supervisor or Manager after working with specimens from a known or suspected EVD patient may be advised not to report for work, and referred to the Center for Occupational and Environmental Medicine (COEM) for evaluation. Ebola Lab Testing Guidance DO NOT DRAW lab specimens for Ebola testing until the following are notified SD Public Health Department (619) 692-8499, after hours (858) 565-5255 UCSD Microbiology laboratory ( Timeline of Infection Within a few days after symptoms begin Diagnostic tests available (will be sent to CDC) Antigen-capture enzyme-linked immunosorbent assay (ELISA) testing IgM ELISA Polymerase chain reaction (PCR) Virus isolation Later in disease course or after IgM and IgG antibodies recovery Retrospectively in deceased Immunohistochemistry testing patients PCR Virus isolation Suggest testing for other conditions with similar presentation: 6. Malaria 7. Lassa fever Version 10-6-14 FJT IPCE Version 0.1 Personal Protective Equipment Specimen Collection: Wear all recommended protective gear (gown, N95 respirator, face shield) PLUS double gloves Specimen Transport: No need for person hand carrying specimens to wear PPE for specimen transport. Double bag all specimens, ensuring outer bag is clean and has not come into contact with exposed surfaces. Contact courier service for transportation of specimens to the microbiology laboratory DO NOT use the pneumatic tube system to transport these specimens, hand carry only. Ebola Cleaning, handling of Trash/Linen Guidance CDC Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus should be followed (http://www.cdc.gov/vhf/ebola/hcp/environmental-infection-control-inhospitals.html). Trash and Linen will be managed by EVS dedicated personnel and should be separate from other clinical linen and waste. Dedicated medical equipment (preferably disposable, when possible) should be used for patient care. All non-dedicated, non-disposable medical equipment used for patient care should be thoroughly cleaned and disinfected with hospital approved disinfectants and according to manufacturer’s recommendations. All disposable items and linen in the patient’s room must be managed as biohazardous waste. Version 10-6-14 FJT IPCE Version 0.1 o When removing from room, place biohazard bag in a second clean red bag held by another staff member with clean gloves (i.e. double bag), to assure the outer bag is clean. Before exiting the patient room or care area, personal protective equipment (PPE) should be carefully removed without contaminating one’s eyes, mucous membranes, or clothing with potentially infectious materials. Disposed of in a red biohazard trash bag/can. Daily and terminal cleaning is per usual hospital protocol by the dedicated/assigned personnel. o If gross contamination of the room is present, contact EVS for blood/body fluid management. o Health care workers or EVS workers performing environmental cleaning and disinfection must wear all recommended PPE. Patient Placement for suspected/known Ebola disease Isolation Precautions: CONTACT and DROPLET PRECAUTIONS with eye protection Place patient into: Burn Intensive Care Unit (room #? Negative pressure, dedicated commode) or SCVC ICU (room#?/negative pressure room) Version 10-6-14 FJT IPCE Version 0.1 Patient Transport for suspected/known Ebola disease Patient Precautions: Cover patient from neck to toe with clean linen. Transport with two biohazardous bags to use in case of vomiting (one bag to contain emesis, second bag to double-bag) In addition to clinical staff involved in the medical care of the patient, TWO transport personnel are recommended: 1. Transporters having contact with the patient or patient bed must wear personal protective equipment (PPE) during transport as additional precaution. PPE must include the following: gown, N95 respirator, face shield, gloves. 2. One “designated chaperone” should accompany the transport team to assist with opening doors, pushing elevator buttons, etc. This individual should remain “clean” by not having contact with the patient or the bed/equipment during transport. No PPE is to be worn by this individual. 3. All clinical staff caring for the patient will wear PPE as described above. Version 10-6-14 FJT IPCE Version 0.1