Northern Health/ DHS powerpoint slides.
advertisement
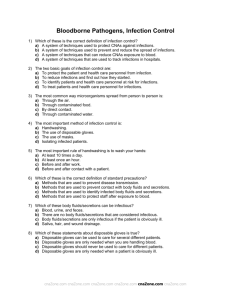
Ebola Virus Disease (EVD) Infection Prevention Guidelines Adapted from the CDC and the CDNA Hayden McDonald – Infection Prevention & Surveillance CNC Jane Tomlinson – Infection Prevention & Surveillance Nurse Coordinator What is Ebola? • Q: What is Ebola? • A: Ebola virus is the cause of a viral haemorrhagic fever disease. Symptoms include: fever, headache, joint and muscle aches, weakness, diarrhoea, vomiting, stomach pain, lack of appetite, and abnormal bleeding. Symptoms may appear anywhere from 2 to 21 days after exposure to Ebola virus although 8-10 days is most common. Transmission • Q: How is Ebola transmitted? • A: Ebola is transmitted through direct contact with – – – – Blood Secretions Organs Other bodily fluids. And Through indirect contact with; – Environments contaminated with such fluid • Transmission through sexual contact may be possible for up to 7 weeks after clinical recovery. • Q: Can I get Ebola from a person who is infected but doesn’t have any symptoms? • A: No. Individuals who are not symptomatic are not contagious. In order for the virus to be transmitted, an individual would have to have direct contact with an individual who is experiencing symptoms. Signs and Symptoms to watch for • Sudden onset of symptoms – – – – – Influenza like illness Fever > 38°C Myalgia Fatigue Headache • 2nd stage – – – – GIT – Vomiting, diarrhoea Neuro – headaches, confusion Vascular cutaneous – maculopapular rash Respiratory – sore throat, cough • Additionally – Septic shock-like syndrome – Multi organ failure – Profuse internal and external bleeding Questions for Triage Patients presenting to ED with fever >=38°C 1. Have you been travelling outside Australia in the last 21 days? 2. If YES, did you travel to Africa? 3. If YES, did you visit any of the following countries – – – – Liberia Nigeria Guinea Sierra Leone IF YES then take IMMEDIATE ACTION! 1) IMMEDIATELY – Patient to wear N95 mask (include any accompanying family/carer) 2) Admit patient immediately to ISOLATION (Resus 3 – negative pressure) and commence Contact & Droplet precautions as designated 3) Notify Director of Emergency or designated deputy 4) Director of Emergency to notify 1) 2) 3) 4) Department of Health 1300 651 160 Infectious Diseases Specialist (via switch) Admitting officer CEO during business hours, After Hours – Exec on call IF YES then take IMMEDIATE ACTION! Part 2 5. Isolate Ambulance entrance - Hospital to go on Bypass (is this necessary at TNH??) 6. Transfer to RMH as soon as safe to do so. 7. ONLY if clinically indicated and ONLY after notification to Department of Health should Pathology tests be taken. 8. DO NOT under any circumstances use a Blood Gas Machine for pathology testing General principles for managing EVD 1) If patient’s condition requires immediate intervention to preserve life then manage in isolation in Emergency with an aim of stabilisation for transport. 2) If the patient is clinically stable arrange immediate transfer to Royal Melbourne Hospital. (we do not have appropriate Critical Care isolation rooms) 170ml / 1 Litre water Provides 5000ppm Possible EVD 1) Personal Protective Equipment – – – – – – – – Scrubs Balaclava Eye protection N95 (P2) mask Plastic Apron Disposable Gown Gloves – 2 pairs (1 long, 1 regular) Long disposable over boots Ensure dedicated or disposable equipment is used for the patient e.g. stethoscope, thermometer etc. • Waste – – – • Designated yellow bin with liner (for incineration) All waste including lined to be bagged inside room and placed in bin for incineration Decontaminate external surfaces with Divercleanse solution (possible ‘sprayer’ to ensure full coverage) Cleaning – – – Divercleanse (bleach/detergent 5000ppm = 170ml / 1 Litre) Ensure all surfaces are disinfected using Divercleanse solution on entry and exit of room Utilise disposable equipment whenever possible Donning PPE 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) Change into surgical scrubs (top and pants for men and women – no dresses Apply disposable Balaclava Apply disposable impervious long sleeve gown Apply plastic apron Apply disposable overshoes Apply N95 (P2) mask – Fit check Apply protective googles Apply non sterile gloves Apply 2nd pair of gloves - long sleeve gloves (use sterile gloves in the interim) Enter patient room Note that details of all persons entering the isolation room must be recorded by a dedicated staff member who will assist staff in donning and doffing PPE. Doffing PPE In patient room 1) Remove external (long sleeve) glove 2) Remove Plastic Apron 3) Remove overshoes In Ante room 1) Remove gown from shoulders and neck turning inside out and finally remove gloves and roll into a bundle 2) Discard into clinical waste 3) Perform hand hygiene 4) Remove balaclava 5) Remove goggles or face shield from behind head 6) Remove mask from behind head (do not touch front of mask) 7) Perform hand hygiene Pathology sampling • • • • • • • Collect only after discussion with Department of Health Collect blood (EDTA) and respiratory swab (Ebola and Malaria testing) 2 person procedure Pre-label specimens Immediately double bag and place into rigid transport container (supplied from Healthscope) and label Hand deliver to Pathology Specimen Reception – pre notification required Healthscope to package and send to VIDRL