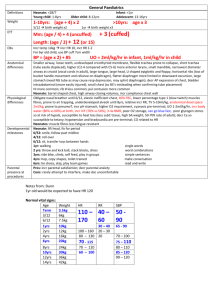
IV fluids fact sheet
advertisement

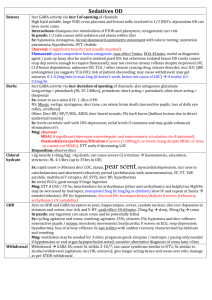
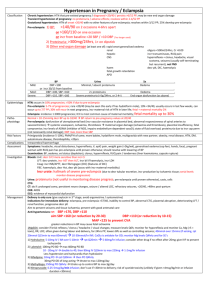
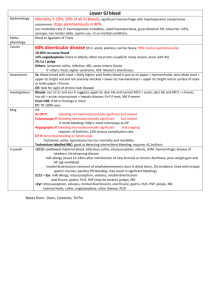
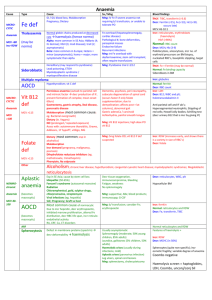
IV fluids Function N saline Hypertonic saline (7.5%) 0.45% saline Hartmann’s Ringer’s lactate 5% dex 10% dex NaHCO3 Gelofusin 4% Albumin 20% Albumin Mannitol Crystalloids vs colloids PRBC 300ml bags (500ml in whole blood) Restore IV vol sufficient for critical organ perfusion; maintain O2-carrying capacity of blood for adequate delivery; correct derangement in coag Na 150 Cl 150 Osm 300 pH 5.3 Indications: replacement of ECF losses, hypoNa, shocked paeds SE: hyperCl metabolic acidosis if large amounts CI: hyperNa, hyperCl, maintenance in paeds Na Cl Osm pH Draws water from ISF to IVF rapid expansion of intravascular space in minimal time; decr SVR (due to vasoD); interstitial dehydration decr ICP and cerebral oedema Indication: HI Dose: 250ml dose (equivalent of 2L saline) SE: phelbitis, fluid overload, hyperNa, osmotic demyelination syndrome Na 75 Cl 75 Osm pH nd Indication: in 2 hr of trt of DKA (avoid hyperCl), trt of hyperNa due to ECF loss Na 131 Cl 111 K5 Ca 2 Osm 278 pH 6 Lactate 29 Physiological electrolyte replacement CI: lactic acidosis, hyperCa/K, hypothermia, clots with blood transfusion Pros: buffers acidaemia Cons: hyperK if renal insufficiency Na Cl Osm 278 pH Glu 50g/L Indications: DM, hyperNa, most effective for establishing urine flow in euvolaemic patient Na Cl Osm pH Glu 100g/L Indications: DKA where normoG but still incr ketones; persistent hypoG unable to eat; sick neonate See below Na 154 Cl 120 Osm 274 pH; vascular expansion lasts 3-4hs; anaphylactoid reactions Na 140 Cl 128 K 0.12 Osm 250 pH 7 Alb 40g/L Indications: hypoV with incr cap perm or hypoAlb; burns after 12hrs; shock and alb <20; therapeutic plasma exchange SE’s: fluid overload, infection, expensive Na 5.5 Cl Osm 80 Alb 20g/100ml Indications: diuresis in hypoproteinaemia; shock and alb <20; haemolytic disease of newborn 0,.5-1g/kg over 30mins SAFE study: No significant difference between albumin (colloid) and saline (crystalloid) in fluid resus of ICU patients in terms of ICU/hospital LOS, duration of mechanical ventilation; subset showed decr mortality in sepsis (statistically insignificant), incr mortality in HI Interstitial dehydration may be good in some circumstances (eg. ARDS, HI) Indications: Hb <7, Hb <10 and symptoms or active bleeding O neg low titre: immediate Group specific: 10mins; O 46% > A 39% > B 11% > AB 3.5%; Rh +ive 80%, Rh-ive 20% XM: 30mins; clinically significant ab’s present in 2% ED patients (5% haem/onc patients), incr with age Effects of storage: incr pH, K, rigidity of cell membrane, citrate decr T, Ca (due to citrate), 2,3,DPG L shift no factor V/VIII activity, no plts Technique: infuse no faster than 5ml/min for 1st 15mins; compatible only with N saline and 4% alb; slowest rate is 1iu/4hrs; can be stored for up to 30/7; Hct 60-70% (35-40% in whole blood) Pros: longer life, less storage problems, less Ags Cons: slower flow, smaller vol, higher viscosity; can’t give meds through same line Complications: Microaggregates (activate coagulation cascade and complement, impairs microcirculation and O2 delivery) ABO incompatibility (usually misidentification error) Citrate toxicity (if >100ml/min; decr ionised Ca, metabolic acidosis, metallic taste / perioral paraesthesia) HyperK (usually if blood >2/52 old); hyperNa Hypothermia (shifts curve to L, decr CO) Febrile non-haemolytic reaction (incidence 0.1-1%; often in multip/multiple transfusions; recipient ab to donor RBC; dose related, towards end of transfusion 30-120mins in or after transfusion; stop transfusion, check pt and blood details if mild (T change <1.5, no rash), restart / if mod (T incr >1.5, urticaria), give anti-histamines and paracetamol, restart after 20mins / if severe stop, send rpt sample; more common with plts) Allergy (recipient reaction to pp’s in donor blood; most common with FFP; 1-3% incidence mild reaction, 1:2050,000 anaphylaxis; trt as fever) FFP 180ml bags Cryo Plt 50ml bags PTX Factor VIIa Haemolysis (1:12-77,000; shock, fever, headache, pain, Hburia, ARF, DIC) Tranfusion related acute lung inj (1:5-10,000; can be fatal; donor ab’s to patient’s WBC’s pul damage SOB, cough, fever, APO within 1-6hrs) Bacterial contamination (1:500,000; more common with plt) Immune suppression Jaundice (30% transfused RBC don’t survive) Transfusion related disease (eg. HIV 1:5400000, Hep C 1:2700000, Hep B 1:739000, malaria etc..) GVHD (transfusion of immunocompetent WBC to immunosupp patient; onset 10-14/7 fever, skin rash, pancytopenia, diarrhoea, abnormal LFT’s; prevent by irradiating blood products) Available in 30mins; do require ABO compatibility; contains all CF’s + fibrinogen; give at 10ml/min (ie over <1hr); give 4-6iu per 5L blood Indications: haemorrhage and coagulopathy; reversal of warfarin OD; factor def; AT III def; TTP Available in 30mins; better if ABO compatibility; contains VIII/XIII, fibrinogen, vWF; give at 10ml/min (ie over <1hr); give 1iu / 10kg body weight Indications: bleeding and fib <1 Available in 15-30mins; do not require ABO compatibility; can only be stored 3/7; 1iu incr plt 5; give 12 units per 5L blood Indications: plt <10 <20 and fever / antibiotics / evidence of systemic haemostatic failure <50 and bleeding (or skin bleeding time >2x normal) or OT (<100 if eye / neuro); neurosurg OT on antiplt DIC / ITP with life-threatening haemorrhage Contains II/V/VII/IX/X, anti-thrombin and heparin; DOA 12-24hrs; give 3ml/min; give 25-50iu/kg (50iu if INR >6, 35iu if INR 4-6, 25iu if INR 2-4) Indications: congenital CF def, warfarin OD and significant bleeding Pros: small vol, rapid admin, no time delay in thawing (unlike FFP), no ABO typing (unlike FFP), INR reversal within 15mins, no disease transmission Not demonstrated to improve any clinically significant outcomes in trials; incr mortality in blunt trauma in CONTROL trial, expensive, requires normal pH and T to be effective; 5% absolute incr risk of VTE; give 90-120mcg/kg Indications: last resort in generalised bleeding only after control of bleeding obtained; inhibitors to CF VIII/X; congenital CF VII def; Glanzmann’s thrombasthenia Notes from: Dunn MOA Indications Use of NaHCO3 8.4% = 1mmol/ml Bicarbonate load buffer H, alkaline urine Na load additive effect to above to help with Na channel blockade Hydrofluoric acid toxicity Correction of severe metabolic acidosis: 0.5mmol/kg for each desired incr in HCO3; endpoint HCO3 >8, clinical improvement of shock / dysrhythmias; incr pH to no greater than 7.2 HCO3 <3, pH <7.2, severe hyperchloraemic acidaemia Cyanide poisoning Isoniazid OD Ethylene glycol, methanol, other toxic alcohols Prolonged cardiac arrest (evidence unclear): Cons: doesn’t improve ability to defib / survival rates in animals; can compromise coronary perfusion pressure; shifts Ox-Hb curve to L (Hb holds on to O2 tissue hypoxia); produces CO2 intracellular acidosis; causes hyperosm and hyperNa; exacerbates central venous acidosis; may inactive adrenaline given; precipitates with Ca; does not correct causes of acidosis Cardiotoxicity 2Y to fast Na channel blockade (cardiac arrest, VF/VT, hypoT): repeated doses of 2mmol/kg IV until stability achieved 100mmol diluted in 1000ml N saline at 100-250ml/hr; aim pH 7.5-7.55; stop when no longer cardiotoxic; will likely need K supplementation TCA, Type 1a and 1c antiarrhythmics: flecainide, quinidine Chloroquine / hydroxychloroquine Antihistamines Antimalarials (quinine) Phenothiazines (eg. Stemetil, chlorprom) Cocaine, carbamazepine Propanolol, LA, type IV, amantadine Urinary alkalinisation in OD enhanced elimination: 1-2mmol/kg IV bolus 100mmol in 1L 5% dex at 250ml/hr; add 20mmol KCl to infusion to maintain normal K; aim urinary pH >7.5 Salicylate – moderate severity not requiring haemodialysis (pH <7.1) Phenobarbitone – if continued toxicity despite MDAC Methotrexate Methanol Rhabdo and myoglobinuria renal failure Urinary sepsis, RTA type 1 Prevention of drug redistribution to CNS – incr unionized amount of drug Salicylate SE’s CI’s Severe hyperK: 50-100mmol slow IV (1mmol/kg in children) Extravasation, gastric distension, hyperNa, hyperosmolality, vol overload, pul oedema, alkalosis (pH >7.6 bad for CV function), L shift of O2-Hb diss curve (impaired O2 unloading), hypoK, hypoCa (usually not clinically significant); incr lactate production (decr citrate and lactate metabolism); resp acidosis (ventilation must account for incr CO2 production) HypoK, hypoCa, alkalosis, acute pul oedema, renal failure, severe hyperNa tone