Generic Risk Assessment - Epilepsy
advertisement
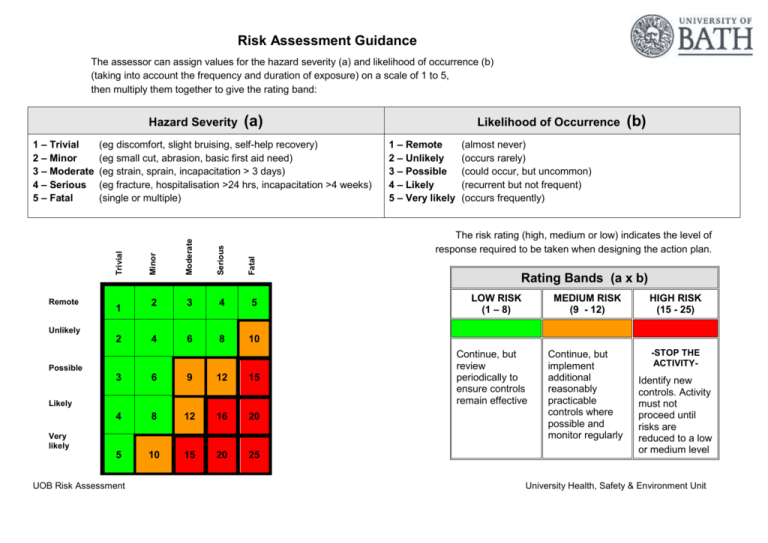
Risk Assessment Guidance The assessor can assign values for the hazard severity (a) and likelihood of occurrence (b) (taking into account the frequency and duration of exposure) on a scale of 1 to 5, then multiply them together to give the rating band: Hazard Severity (eg discomfort, slight bruising, self-help recovery) (eg small cut, abrasion, basic first aid need) (eg strain, sprain, incapacitation > 3 days) (eg fracture, hospitalisation >24 hrs, incapacitation >4 weeks) (single or multiple) Serious Fatal 1 Moderate Remote Likelihood of Occurrence 1 – Remote 2 – Unlikely 3 – Possible 4 – Likely 5 – Very likely (b) (almost never) (occurs rarely) (could occur, but uncommon) (recurrent but not frequent) (occurs frequently) The risk rating (high, medium or low) indicates the level of response required to be taken when designing the action plan. Minor Trivial 1 – Trivial 2 – Minor 3 – Moderate 4 – Serious 5 – Fatal (a) 2 3 4 5 4 6 8 10 Rating Bands (a x b) LOW RISK (1 – 8) MEDIUM RISK (9 - 12) HIGH RISK (15 - 25) Continue, but implement additional reasonably practicable controls where possible and monitor regularly -STOP THE ACTIVITY- Unlikely 2 Possible 3 6 9 12 15 4 8 12 16 20 5 10 15 20 25 Likely Very likely UOB Risk Assessment Continue, but review periodically to ensure controls remain effective Identify new controls. Activity must not proceed until risks are reduced to a low or medium level University Health, Safety & Environment Unit U:\safety\Working off site\Risk Assessment\Risk assessments generic\risk assessments drafts\epilepsy_staff_v3_2013.docx Risk Assessment Record Risk Assessment of: Assessor(s): Date: Generic risk assessment for epileptic members of staff. Overview of activity / location / equipment / conditions being assessed: This assessment is limited to staff with epilepsy whose condition may affect or be made worse by their work. It is likely that the University population includes about 180 people with epilepsy. However, in the majority of cases the condition is likely well controlled and will never be a work issue. This assessment provides a starting point for completing a risk assessment for activities that involve a Member of staff with epilepsy. The assessment includes prompts for line managers to gather further information to aid the assessment and decision making process. As each person will likely experience epileptic seizures in a unique way, each case must be considered individually and a personalised assessment made. Some of the issues identified may be applicable only rarely – the photo-epileptic section being a prime example. Issues that are not relevant to the final personalised assessment should, after enquires and consideration, be deleted. Generic or specific assessment? Generic risk assessment UOB Risk Assessment Context of assessment Generic assessment / Starting point for a personalised assessment University Health, Safety & Environment Unit # Hazard(s) identified Persons affected PREAMBLE – GENERAL PRINCIPLES For persons whose medical condition has a ‘substantial’ and ‘long-term’ negative effect on their ability to do normal daily activities, their disability must be considered in the light of the Equalities Act 2010 and the University has a legal duty to make ‘reasonable adjustments’ to allow them to enter or maintain employment. Further information about this can be obtained from the HR Manager for your department. Member of staff with epilepsy About 1 in 100 people have epilepsy. This equates to about 180 people with epilepsy in the University population. SEIZURE EFFECTS Each person affected will experience epilepsy in a way that is unique to him or her. The seizures may manifest in different ways, depending on the area of the brain affected. 1A FOCAL SEIZURES (also called partial or local seizures). The epileptic activity is in just part of the brain. The member of staff may remain alert during the seizure or may not be aware of what is happening. The member of staff may experience uncontrolled movements or unusual sensations and feelings. Onlookers may not be aware that they are having a seizure. Focal seizures can escalate to generalised seizures. GENERALISED SEIZURES. The epileptic activity involves large sections of the brain. The member of staff will probably lose consciousness, may stiffen or jerk and may fall down. Sometimes these types of seizure can be extremely brief. UOB Risk Assessment Member of staff with epilepsy Persons who may be affected by work performed by person with epilepsey Existing controls & measures Employees should report if they have epileptic condition that may affect their work. The purpose of reporting is to enable the University to: Make a risk assessment; Make reasonable adjustments; and Make a personalised care plan. Employees should report epileptic conditions / changes in their condition to their line managers. If employees have uncontrolled seizures, then some activities will not be suitable for them on health & safety grounds. Examples include: Work at height with unprotected falls (eg ladder work); Work with high voltage electricity or live electrical work; Work on or near moving vehicles; Work with unguarded fires, ovens or hot plates; and Work at isolated locations. If seizures are well controlled / activities are less hazardous, it will be a matter of judgement what precautions are needed. A B A x B Additional controls required Manager to take further action Complete a personalised risk assessment; Identify and implement any reasonable adjustments needed for the workplace or job; and Identify and implement a personalised care plan. Manager to make further enquires. Possible avenues for investigation are: Do you have seizures? What type of seizures do you have? How often do you have seizures? What usually happens when you have a seizure? How long does it usually take you to recover from a seizure? What time of day do you usually have seizures? Do you get a warning before a seizure starts? Is there any part of your workplace or job that concerns you? University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures A B A x B Additional controls required SEIZURE EFFECTS 1B Seizures may manifest in different ways. In some instances, people nearby may not even realise that the member of staff is having a seizure. In other instances, the effects may be obvious and distressing. Some staff members may be stressed by others suffering seizures or the threat that they might suffer a seizure. Some staff members may have difficulty coping with this. This may be detrimental to the everyone. Difficulties arising from this may increase seizure risks. SEIZURE THRESHOLDS & TRIGGERS 2 Most people with epilepsy have a ‘seizure threshold’ - the point at which the brain’s natural resistance to seizures is passed, triggering a seizure. People with a low threshold have frequent seizures, whereas people with a high threshold experience less frequent seizures and triggers will have less effect on them. Many people with epilepsy find certain circumstances or substances can trigger a seizure. Common triggers are: Stress; Lack of sleep; Alcohol consumption, particularly binge drinking and during a hangover; Illegal drugs and some pharmaceuticals, especially stimulants (amphetamines, cocaine, etc) and opiates (heroin, methadone, codeine, etc); Illness or health conditions that cause a fever; and Flashing or flickering lights (photo-epilepsy). Some women may be more prone to seizures just around the time of their period. Common epilepsy triggers that are within the control of the University are considered below. UOB Risk Assessment Member of staff with epilepsy Persons working in the vicinity Dependent upon the personalised assessment findings, consider providing information, instruction & training to staff & any other support as might be needed. Information and support can be accessed via the HR web site. Member of staff with epilepsy Most of the common triggers are outside the control of the University (eg alcohol consumption, illegal drugs, etc). University to make reasonable adjustments to workplace and job to remove or reduce known triggers within its control. Manager to make further enquires. Possible avenues for investigation are: Are there any specific circumstances or substances that trigger your seizures? Is there any part of your workplace or job that exposes you to these triggers? What adjustments need to be made to the workplace to eliminate or control triggers? University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures 2A B A x B Additional controls required Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS - STRESS & EPILEPSY Stress does not cause epilepsy, but it can causes changes to the way nerve cells in the brain respond, making a seizure more likely. Stress can cause changes in lifestyle that make a seizure more likely. For instance, stress may cause someone to miss anti-epileptic mediations or suffer sleep disturbances. Additionally, worrying about seizures can add to stress. This can become a vicious circle, with stress causing seizures and the seizures causing more stress. A Member of staff with epilepsy See University “Stress Management” policy and associated guidance - the Universities arrangements for assessing and managing stress. If the stress of a new job, or significant changes to your role, is an issue, are temporary adjustments needed for the start period? Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS - LACK OF SLEEP & EPILEPSY 2A Lack of sleep or irregular sleep patterns can lower thresholds, making a seizure more likely. Irregular sleep patterns may disturb anti-epileptic mediations regimes, making a seizure more likely. Member of staff with epilepsy University to make reasonable adjustments to workplace and job to allow sufficient sleep / avoid sleep disturbance. Is stress a known trigger of your seizures? Is a stress assessment needed? Is lack of sleep a known trigger of your seizures? Does your shift pattern interfere with any anti-epileptic medication regime? Does your shift pattern interfere with normal sleeping patterns? Are there any disturbances in your work-life balance that interferes with sleep patterns (eg new baby, change in travel arrangements, etc)? NOTE: An additional assessment may be needed if the employee is involved in any occasional activity that may disturb normal sleep patterns eg attendance on field trips, travelling for business, being on call, etc. UOB Risk Assessment University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures 3 SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY - CEILING FANS 3A A light seen through a fast-rotating ceiling fan may trigger a seizure. UOB Risk Assessment B A x B Additional controls required Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY Photosensitive epilepsy is a type of epilepsy, in which all or most seizures are triggered by flashing or flickering light. The seizure will usually happen at the time or shortly after exposure. The seizure may be focal or generalised. The instance of photo epilepsy in the general population is about 3 in 10,000. There are likely to be about 2 members of the University population who are photo-epileptic. Specific common photo-epilepsy triggers are considered below. A Members of staff with photoepilepsy Members of staff with photoepilepsy University to make reasonable adjustments to workplace and job to remove or reduce known triggers within its control. Do you suffer from photosensitive epilepsy? Is there anything within your workplace or job that might trigger a photo epileptic seizure? Is there anything within your workplace or job that might increase the risk of having a photo epileptic seizure? If ceiling fans are installed, they must be slow rotating. (Any flickering should be <=4Hz) University Health, Safety & Environment Unit # Hazard(s) identified Persons affected SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY - IT EQUIPMENT 3B Flashing or flickering lights on the screen may trigger seizures. Rapidly changing images on the screen may trigger seizures. Members of staff with photoepilepsy Contrasting or moving patterns on the screen may trigger seizures SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY - LIGHTING 3C Fluorescent strip lighting and bulbs may trigger seizures if they flicker because they are faulty. UOB Risk Assessment Members of staff with photoepilepsy Existing controls & measures COMPUTER SCREENS Make sure the workroom is well lit and provide a desk lamp near to the screen (to lessen high contrast patterns). If possible, use a LCD or Plasma screen. If you use a CRT screen make sure that the refresh rate is set to >70 Hz. Most business applications (eg word processing) are unlikely to generate flashing lights or high contrast patterns. INTERACTIVE WHITEBOARDS Interactive whiteboards are unlikely to cause problems unless they are used to project flashing or flickering lights or contrasting patterns Faulty lighting to be reported and replaced in the work area. Whilst awaiting repair of the light, persons with photo-epilepsy should work elsewhere. A B A x B Additional controls required Manager to make further enquires. Possible avenues for investigation are: Is using a computer screen with business applications likely to trigger an epileptic seizure? Is using an interactive white board with business applications likely to trigger an epileptic seizure? Photo epileptics who experience any discomfort, such as dizziness, blurred vision, loss of awareness, or muscle twitching while using IT equipment should stop looking at the screen immediately and leave the area. The problem should be reported to the manager and the risk assessment updated accordingly. University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures A B A x B Additional controls required ENTERTAINMENT VENUES SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY - STROBE LIGHTING Strobe lights in places such as nightclubs may trigger 3D seizures. Members of staff with photoepilepsy Strobe lights used during the course of research may trigger seizures. Follow HSE guidelines1 and any conditions imposed by Local Authority Licensing Authority. In brief: Warning at entrance Flicker rates =< 4Hz Synchronised flashing Mount above head height Diffuse strobe light Not in corridors / stairs Limit period of use RESEARCH VENUES Manager to make further enquires. Possible avenues for investigation are: Follow HSE guidelines where possible. Where not, produce a separate assessment to control use and exposure. Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY - HIGH CONTRAST PATTERNS 3E Some high contrast or moving patterns can trigger seizures in some people. Some examples would be: 1 Black and white stripes; Some patterned materials and wallpaper; Large areas of floor and ceiling tiles with high contrast lines; and Looking down a moving escalator. Is there anything within your workplace or job that might trigger a photo epileptic seizure? Is there anything within your workplace or job that might increase the risk of having a photo epileptic seizure? What measures need to be taken to eliminate triggers or control exposure? Members of staff with photoepilepsy Is there anything within your workplace or job that might trigger a photo epileptic seizure? Is there anything within your workplace or job that might increase the risk of having a photo epileptic seizure? What measures need to be taken to eliminate triggers or control exposure? The Event Safety Guide. A guide to health, safety and welfare at music and similar events. HSG195. See Chapter 17 special effects, fireworks and pyrotechnics, paragraphs 614-616 UOB Risk Assessment University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures A B A x B Additional controls required Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS PHOTOSENSITIVE EPILEPSY - SUNLIGHT EFFECTS 3F Sunlight alone is unlikely to trigger photosensitivity. However, sunlight interacting with the workplace can create patterns or flickering light sources that can trigger a seizure. Examples might be: Sunlight coming through slatted blinds Sunlight coming through railings as you walk past them Members of staff with photoepilepsy SEIZURE THRESHOLDS & TRIGGERS - ANTI-EPILEPTIC MEDICATIONS (AED) - MAINTAINING REGIME 4 The Member of staff with epilepsy may take AED; these will not cure epilepsy, but can reduce or prevent seizures. Generally, AED are taken one – three times per day. It is important that AED are taken as prescribed as missing a dose can sometimes trigger a seizure. Some users of AED may have regular blood tests at their Doctors to monitor AED levels or other indicators. UOB Risk Assessment Member of staff with epilepsy on AED regime University to make reasonable adjustments to workplace and job to permit AED regime to be adhered too. This includes: Ensuring the person has sufficient time to adhere to AED regime during the working day; Ensuring the persons working patterns are conducive to adhering to the AED regime; and Ensuring that the person can attend AED monitoring session as required. Is there anything within your workplace or job that might trigger a photo epileptic seizure? Is there anything within your workplace or job that might increase the risk of having a photo epileptic seizure? What measures need to be taken to eliminate triggers or control exposure? Manager to make further enquires. Possible avenues for investigation are: Are you able to maintain your AED regime with your current working arrangements? What measures need to be taken to enable you to maintain your current AED regime? University Health, Safety & Environment Unit # Hazard(s) identified Persons affected SEIZURE THRESHOLDS & TRIGGERS - ANTI-EPILEPTIC MEDICATIONS (AED) - CHANGING REGIME 4A A doctor may occasionally suggest a different dosage or dosing pattern to improve seizure control or reduce side effects. For medical reasons, the member of staff may have to switch from one AED to another (eg side effects, change in epilepsy, etc). The staff member may be more prone to seizures during the transition. Changing regime may also cause side effects, although these may reduce or disappear with time. Member of staff with epilepsy on AED regime Existing controls & measures A B A x B Additional controls required Employees should report if they are changing their AED regime / AED medication if this is may affect their work. The purpose of reporting is to enable the University to: Manager to make further enquires. Possible avenues for investigation are: Update the health & safety risk assessment; Update any reasonable adjustments are made; and Update the personalised care plan. Are temporary adjustments needed for the transition period? Are permanent adjustments needed for the new AED regime? See 4 for instance Employees should report changes to their line manager. SEIZURE THRESHOLDS & TRIGGERS - ANTI-EPILEPTIC MEDICATIONS (AED) -INTERACTION WITH OTHER DRUGS Some medications may increase the seizure risk. These 4B medicines include many of the antidepressants, some types of anti-histamine, some antibiotics and some anti-malarial treatment. The increased risk may arise because the medications interact with AED or they may lower the seizure threshold. Member of staff with epilepsy on AED regime This will normally be outside the control of the University. The interaction of some medications with the AED / seizure threshold may cause problems for some activities (eg travelling on a field trip to an area where malaria is prevalent). Medical advice will be required Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS - ANTI-EPILEPTIC MEDICATIONS (AED) - SIDE EFFECTS Some AED may interfere with memory functioning as they 4C affect the speed at which the brain can process information. This may be worse during changes between different AED regimes. The risk of side effects will depend on a number of things, including the AED taken and any other medications. UOB Risk Assessment Member of staff with epilepsy on AED regime How can information and instructions be presented to be of most use? If you suffer from AED side effects, what adjustments need to be made to your workplace or job to enable you to cope with them? The Epilepsy Action pamphlet Memory and epilepsy presents some strategies for coping with this aspect of epilepsy. University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures 5 6 Enabling and assisting a person with learning difficulties can be stressful if the enabler/assistant/line manager has not been trained in how to do it, or is unable to understand or carry out the training Without support and enabling by knowledgeable colleagues, a person with epilepsy and a learning difficulty might find it disadvantageous to their employment. UOB Risk Assessment A x B Additional controls required Member of staff with epilepsy with VNS device Magnetic fields (eg around an NMR unit) may interfere with the VNS unit. LEARNING DIFFICULTIES Around one in every four people with epilepsy has learning difficulties. Therefore, of the potential 180 employees with epilepsy, 45 may have some form of learning difficulty. B Manager to make further enquires. Possible avenues for investigation are: SEIZURE THRESHOLDS & TRIGGERS - ANTI-EPILEPTIC TREATMENT – VAGUS NERVE STIMULATION Vagus Nerve Stimulation (VNS) is a treatment for epilepsy where a small device is implanted under the skin, near the collarbone. This device stimulates the vagus nerve at regular intervals during the day, helping to prevent seizures. A Member of staff with epilepsy Person supervising / managing member of staff with epilepsy Dependent upon the personalised assessment findings, consider providing information, instruction & training to staff & any other support as might be needed. Information and support can be accessed via the HR web site. Do you use a VNS unit? What advice have you been given regarding working in or around strong magnetic fields? Does your VNS trigger automatically? Should we trigger your VNS manually if you have a seizure? Manager to make further enquires. Possible avenues for investigation are: How can information and instructions be presented to be of most use? The Epilepsy Action pamphlet Memory and epilepsy presents some strategies for coping with this aspect of epilepsy University Health, Safety & Environment Unit # Hazard(s) identified Persons affected PROVISION OF FIRST AID - FOCAL SEIZURES 7A Member of staff may suffer a focal seizure and require first aid assistance. Likely symptoms are: The person is not aware of their surroundings or of what they are doing, this may manifest as Plucking at their clothes Smacking their lips Swallowing repeatedly Wandering around UOB Risk Assessment Member of staff with epilepsy First aid providers Colleagues in the vicinity. Existing controls & measures Provide first aid treatment as recommended – see first aid information sheet Guide the person away from danger Stay with the person until recovery is complete Be calmly reassuring Explain anything that they have missed During a seizure do not Restrain the person Act in a way that could frighten them (such as shouting or being overly forceful) Assume the person is aware of what is happening or what has happened Give them anything to eat or drink until they are fully recovered Attempt to bring them around A B A x B Additional controls required First Aid at Work qualified first aiders are unlikely to be routinely trained in epilepsy awareness. It is advisable for the person with epilepsy to contact their local first aiders to make them aware of possible need for action. (Managers can do this on behalf of a staff member if they so wish). The person’s regular work colleagues would also benefit from having information about what to do in case of a seizure. University Health, Safety & Environment Unit # Hazard(s) identified PROVISION OF FIRST AID - GENERALISED SEIZURES 7B Member of staff may suffer a generalised seizure and require first aid assistance. The member of staff will probably lose consciousness, may stiffen or jerk and may fall down. Sometimes these types of seizure can be extremely brief. UOB Risk Assessment Persons affected Member of staff with epilepsy First aid providers Colleagues in the vicinity. Existing controls & measures Provide first aid treatment as recommended – see first aid information sheet Protect the person from injury (remove harmful objects from nearby etc) Cushion their head Aid breathing by placing them in the recovery position when the seizure has finished Stay with them until recovery is complete Be calm and reassuring During a seizure do not Restrain the persons movements Put anything in their mouth Try to move them unless they are in imminent danger Give them anything to eat or drink until they are fully recovered Attempt to bring them around A B A x B Additional controls required First Aid at Work qualified first aiders are unlikely to be routinely trained in epilepsy awareness. It is advisable for the person with epilepsy to contact their local first aiders to make them aware of possible need for action. (Managers can do this on behalf of a staff member if they so wish). The person’s regular work colleagues would also benefit from having information about what to do in case of a seizure. University Health, Safety & Environment Unit # Hazard(s) identified Persons affected Existing controls & measures CONTACT SECURITY TO SUMMON AMBULANCE At the University, Security are responsible for requesting an ambulance and managing its arrival. PROVISION OF ASSISTANCE AFTER A SEIZURE – CARE PLAN 7C The University may need to summon an ambulance following a seizure. To prevent unnecessary emergency calls, a care plan should be formulated that outlines normal seizure patterns and what response should be made. Note that some persons with epilepsy may become incontinent during a seizure. The care plan should address any need for providing privacy during recovery. Member of staff with epilepsy Generally, an ambulance will be summoned if: First aid providers Colleagues in the vicinity Security Officers Persons first seizure; Seizure continues for more than five minutes; One seizure follows another without the person regaining consciousness; or The person is injured during the seizure. PERSONALISED RESPONSE Personalised care plans to be identified between the epileptic staff member and manager. A B A x B Additional controls required Manager to make further enquires. Possible avenues for investigation are: What happens when the employee has a seizure? What assistance might be needed during a seizure? What assistance might be needed after a seizure? Will you need privacy after a seizure? Seizures are usually the same for a person each time they happen. If recovery time is brief, the person may just need a quiet place to rest before returning to work. Decide in advance a suitable resting place(s). If recovery is lengthy and the person needs to go home, decide how they will get there. Bear in mind that some people may be dazed and confused after a seizure and may not be safe to travel alone. Information sources consulted: Epilepsy Action publications available from www.epilepsy.org.uk Assessor signature: UOB Risk Assessment Print name: Review date: University Health, Safety & Environment Unit Risk Assessment Action Plan Action Plan in respect of: Ref no. Prepared by: Action to be taken, incl. Cost Responsible manager’s signature: Print name: UOB Risk Assessment By whom Target date Review date Outcome at review date Responsible manager’s signature: Date: Print name: Date University Health, Safety & Environment Unit