chapter 5 conditions affecting children`s health
advertisement
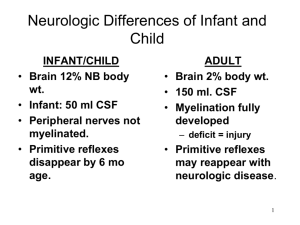
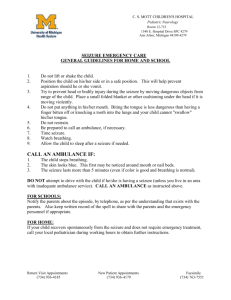
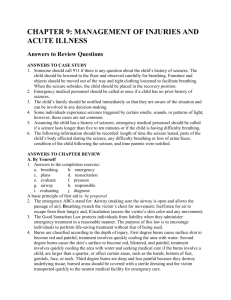
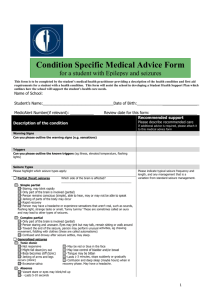
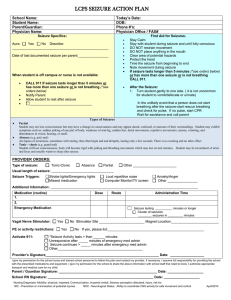
CHAPTER 4: COMMON CHRONIC MEDICAL CONDITIONS AFFECTING CHILDREN’S HEALTH Answers to Review Questions ANSWERS TO CASE STUDY 1. Tonic-clonic. 2. Most likely, the child’s shriek was an early indication of the impending seizure. 3. The child will lose consciousness, experience uncontrollable contractions of the entire body. Additionally, the child may lose control of bowel and/or bladder function during the seizure. When the seizure ends, the child may wake up briefly and then fall into a deep sleep. 4. Yes, Mr. Lui was correct in calling for emergency medical assistance given the circumstances (e.g., location, unknown cause of the child’s seizure, not familiar with the child’s medical condition). If Mr. Lui had known about the child’s history of seizures, he might have waited a few minutes to see if the seizure would end. However, he made a wise decision based on his assessment of the situation at the time. 5. Mr. Lui should place the child in a recovery position (on her side) and encourage her to rest quietly, contact the child’s family, and record information regarding his observations and response. 6. This event provides an excellent opportunity for teaching children about seizures, about children who may have medical conditions, and how to respond in an emergency. ANSWERS TO CHAPTER REVIEW A. By Yourself 1. Have students write a sentence and define each of the terms listed. 2. There are many reasons why this may occur. Families may not intentionally ignore a child’s health problem. However, because some conditions develop slowly over a period of time, changes in a child’s health may be difficult to recognize. Some families may not be sure that a problem exists or where to go for help. Others may be in denial or hope the child will eventually outgrow the problem. 3. Febrile seizures are experienced primarily by infants and toddlers when they have a high fever. The convulsive episodes are not harmful and this type of seizure activity is usually outgrown around two years of age. Absence seizures (petite mal) are characterized by momentary loss of consciousness, whereas tonic-clonic seizures (grand mal) usually begin with an aura and involve a complete loss of consciousness followed by convulsive movements of the entire body. Partial seizures (focal) are the most common form of seizure activity and are characterized by involuntary movements of various body parts (e.g., arm flailing, tongue clicking, inappropriate outbursts of laughter). The child may/may not lose consciousness and often has no recall of the event. 4. Early signs of diabetes include weight loss despite eating, fatigue or weakness, frequent urination, excessive thirst, and dry, itchy skin. Each community has unique resources that teachers can turn to for help in understanding and supporting children who have diabetes, including the child’s pediatrician, health clinics, public health departments, visiting nurses, hospital dieticians, and local diabetes support groups. 5. Refer to Table 4-1. Colds are usually accompanied by fever, cough, generalized discomfort and last 7-10 days. Allergies do not cause fever, may cause a non-productive cough, and do not go away until the offending allergen is no longer present (seasonal). B. As a Group 1. There are many chronic medical conditions that students can use for this activity. 2. An emergency plan should include having complete information about the child’s condition on file (e.g., type of seizure the child experiences, conditions that may trigger seizure activity, how the child generally responds before/following a seizure, if the child takes medication to control seizures). Emergency contact information (e.g., parent’s home/work/cell telephone numbers, child’s physician, other persons to be contacted in the event parents can not be reached, hospital preference) should also be obtained and reviewed frequently. School personnel should know how to manage a child’s seizure (lower to the floor, protect the child’s head, observe breathing closely, call 911 if this is a first seizure or it lasts longer than five minutes) and be trained to administer CPR. An emergency plan should also address communication—which school personnel should be notified, who contacts the child’s family, who calls for emergency medical assistance (EMT), and who administers medications if they are needed. 3. Factors that may be linked to an increasing incidence of allergies and asthma among young children include exposure to an increasing number of environmental pollutants (air, water, chemicals, additives), poor environmental sanitation, introducing infants to solid foods too early, not breastfeeding an infant, being born to a mother who smokes, repeated exposure to second-hand smoke, and childhood obesity. Researchers have also suggested that children may be growing up in environments that are being kept too clean. As a result, children’s immune systems begin responding to many environmental substances as if they were allergens. 4. The environment begins to influence a child’s health shortly after conception. Substances to which a mother is exposed and her lifestyle practices during pregnancy affect a child’s developmental outcome. Following the infant’s birth, environmental factors continue to have a direct effect on children’s well-being: where they live; the family’s financial resources; exposure to environmental toxins (air, water, food, chemicals); exposure to stress and/or domestic violence; disruptions in the family unit (e.g., death, divorce, abandonment); dietary quality; and access to medical and dental care. 5. When a child who has undergone treatment for cancer is ready to return to school, it is important that teachers work closely with the child’s family to determine what accommodations (e.g., dietary, opportunities for rest, seating arrangements) are needed. It may also be necessary to modify classroom activities for the child to address potential memory lapses, difficulties with concentration, and low energy levels. Attention must also be paid to maintaining careful hand washing and sanitation practices to reduce the child’s exposure to infectious organisms.