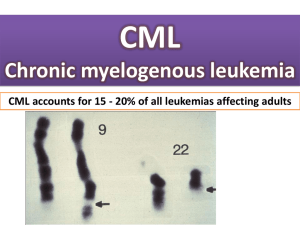
Chronic Myelogenous Leukemia (CML)
advertisement

Usama Ur Rehman (14-10532) Biot 412 L. Johnson Chronic Myelogenous Leukemia Chronic Myelogenous Leukemia (CML) is the cancer of white blood cells. It is a bone marrow stem cell disorder in which proliferation of mature granulocytes such as neutrophils, eosinophils, basophils and their precursors are observed. It causes unregulated and rapid growth of myeloid cells in bone marrow which are inevitably released in blood. Molecular cause CML occurs due to the translocation of chromosome 9 with chromosome 22, which in 95% of CML cases result in the formation of Philadelphia chromosome (Ph+). (A)1 This translocation directly effects ABL gene, which is a proto-oncogene. ABL gene is responsible for the synthesis of certain tyrosine kinase known as Abelson tyrosine kinase. This kinase is associated with cell functions such cell differentiation, cell division and stress signals. 1 http://en.wikipedia.org/wiki/File:Philadelphia_Chromosom.svg it shows the formation of Ph+ CML In CML, this ABL gene is fused with BCR (break cluster region) due to translocation and results in the formation of BCR-ABL oncogene. Mutated protein synthesized, without being regulated by cytokines, causes disordered growth and proliferation of cell. All CML cases are related to mutation in this ABL gene. Symptoms Patients often don't have any specific condition related at diagnosis. They might present sometimes with high white blood cell count on a regular laboratory test. Symptoms of CML usually include: malaise, enlarged spleen causing pain on the left side, joint and hip pain, anemia, low-grade fever, increased susceptibility to infections, and thrombocytopenia with easy bruising Stages The process of staging in CML shows us the amount of cancer spread in patient which is extremely important for treatment in any cancer. These stages are typically associated with the total amount of cancerous cells which are present, as blast cells, in the body. The stages are: Chronic phase In chronic phase, less than 10% of the cells found in the blood and bone marrow are blast cells. Accelerated phase In accelerated phase, 10%-19% of the cells in the blood and bone marrow are blast cells. Blastic phase In blastic phase, 20% or more of the cells in the blood or bone marrow are blast cells.2 Diagnostics As explained before CML doesn't have any particular symptom and can be indicated by a routine lab test. The best test for verifying CML either Ph+ or Ph- is through FISH (Fluorescent in situ hybridization). This test verifies the mutation in ABL gene through fluorescent marker. CML patients often are more susceptible for more genetic mutations in cancerous region. Identification of these mutations are done through PCR and Scorpion assay etc. 2 http://www.cancer.gov/cancertopics/pdq/treatment/CML/Patient/page2 Treatment The basic treatment for CML are tyrosine kinase inhibitors. One molecular level, CML is caused by disordered and unregulated activity of Abelson tyrosine kinase. These inhibitors slow down or stop this unregulated activity of kinase by competing for attachment to Abl kinase active site. first drug used successfully in treating CML was imatinib which proved extremely useful initially but it was seen that more than 80% of CML patients relapsed and stopped responding to imatinib. Result regarding the affectivity of imatinib showed that cancerous cells in relapsed CML patients have gained mutations which have made these cells resistant to imatinib. 3 The above given graph shows several of mutations seen in post-imatinib treatment CML patients. It also shows the frequency of these mutations in such patients. 3 It has been shown through research that the T315I and E255K mutations confer IL-3 independence as well as biochemical and biological resistance to imatinib in CML. 4 A majority of these relapsed patients have several point mutations at and around the ATP binding pocket of the ABL kinase domain in BCR-ABL. In order to address the resistance of 3 S. Soverini et.al, Contribution of ABL Kinase DomainMutations to Imatinib Resistance in Different Subsets of Philadelphia-Positive Patients: By the GIMEMA Working Party on Chronic Myeloid Leukemia, Clinical Cancer Research, 2006;12(24) 4 Neil P. Shah et al., Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia, CANCER CELL : VOL. 2, 2002. mutated BCR-ABL to imatinib, 2nd generation inhibitors such as dasatinib, and nilotinib were developed. These compounds were approved for the treatment of CML patients who are resistant to imatinib. All of the BCR-ABL mutants are inhibited by the 2nd generation inhibitors with the exception of the T315I mutant. T315I happens to be more frequent in the latter stages of CML hence making cancer resistant to kinase inhibitors. A lot of research is still going on in finding a drug that can be effective against T3151 mutant CML but for now there is no cure for CML.5 Further readings Michele Modugno, Elena Casale, Chiara Soncini, et al., Crystal Structure of the T315I Abl Mutant in Complex with the Aurora Kinases Inhibitor PHA-739358, Cancer Res 2007; 67: (17). 2007 Jorge Cortes, Elias Jabbour, Hagop Kantarjian, C. Cameron Yin, Jianqin Shan, Susan O'Brien,Guillermo Garcia-Manero, Francis Giles, Megan Breeden, Nubia Reeves, William G. Wierda and Dan Jones., Dynamics of BCR-ABL kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors, blood journal, 2011 5 http://www.ncbi.nlm.nih.gov/pubmed/18673174