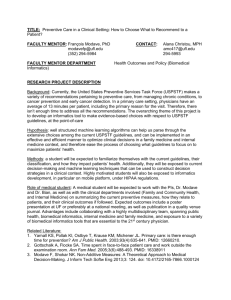
downloading - University of Kansas Medical Center
advertisement
Barohn, Richard J. SECTION 3: BIOMEDICAL INFORAMTICS A. INTRODUCTION AND SPECIFIC AIMS Biomedical Informatics accelerates scientific discovery and improves patient care by converting data into actionable information. Pharmacologists and biologists receive improved molecular signatures; translational scientists use tools to determine potential study cohorts; providers view therapeutic risk models individualized to their patient; and policy makers can understand the populations they serve. Informatics methods also lower communication barriers by standardizing terminology describing observations, integrating decision support into clinical systems, and connecting patients with providers through telemedicine. The Heartland Institute for Clinical and Translational Research (HICTR) has catalyzed the development and integration of informatics capabilities to specifically support translational research in our region and to address issues and needs like those identified above. Our vision is to provide rich information resources, services, and communication technologies across the spectrum of translational research. We will: a) adopt methods which facilitate collaboration and communication both locally and nationally, b) convert clinical systems into information collection systems for translational research, c) provide innovative and robust informatics drug and biomarker discovery techniques, d) work with state and regional agencies to provide infrastructure and data management for translational outcomes research in underserved populations, and e) measure clinical information systems’ ability to incorporate translational research findings. Our specific aims complement the novel methods and technologies of our region and target translational needs requiring further investment. Specific Aims: 1. Provide a HICTR portal for investigators to access clinical and translational research resources, track usage and outcomes, and provide informatics consultation services. 2. Create a platform, HERON (Healthcare Enterprise Repository for Ontological Narration), to integrate clinical and biomedical data for translational research. 3. Advance medical innovation by linking biological tissues to clinical phenotype and the pharmacokinetic and pharmacodynamic data generated by research in phase I and II clinical trials (addressing T1 translational research). 4. Leverage an active, engaged statewide telemedicine and Health Information Exchange (HIE) to enable community based translational research (addressing T2 translational research). B. BACKGROUND The University of Kansas has a wide range of informatics capabilities, developed over decades of research and service. Through the National Center for Research Resources (NCRR) IDeA Networks for Biomedical Research Excellence (INBRE), the Kansas’ KINBRE has created a ten campus network of collaborative scientists using common bioinformatics resources. Kansas has pioneered the use of telemedicine since the early 1990s, providing inter-state connectivity at over 100 sites and conducting thousands of clinical consultations and hundreds of educational events for health care professionals, researchers, and educators. The Center for Health Informatics’ Simulated E-hEalth Delivery System, a jointly funded program between the University of Kansas and Cerner Corporation, creates an equitable partnership to fully integrate applied clinical informatics into an academic setting and supports over 40 international academic clients. These existing efforts are complemented by more recent investments in clinical research informatics and medical informatics. B.1. Medical Informatics In 2010, KU committed $3.5 million dollars over the next 5 years towards medical informatics academics and service and recruited Russ Waitman, PhD to lead the Division of Medical Informatics in the Department of Biostatistics, to integrate clinical research informatics, and to provide overall leadership for the HICTR Biomedical Informatics program. Dr. Waitman was previously responsible for directing the development, implementation, commercialization, and operation of the inpatient clinical systems used at Vanderbilt University Medical Center––both internally developed applications by the Computerized Provider Order Entry team (the WizOrder project, medication reconciliation) and commercial nursing documentation and barcode medication administration systems. Dr. Waitman conducted research to extend education and decision support into 1 Barohn, Richard J. clinical systems as well as NIH funded research to discover medication-laboratory result relationships, measure the utility of preadmission medication data for post-marketing surveillance of adverse drug events, and build surveillance systems for acute kidney injury. Over time, his team’s clinical research database combined ten years of clinical, administrative, social security death index, and user activity log data to support three National Library of Medicine (at NIH) funded grants (R01 LM007995; R01 LM009965; R01 LM007995). Concidental with Dr. Waitman’s recruitment, this year the University of Kansas Hospital will complete their fiveyear, $50 million investment to implement the Epic Electronic Medical Record, concluding with Computerized Provider Order Entry in November. This effort has transformed the inpatient environment. The University of Kansas Physicians have now begun adoption of Epic across all ambulatory clinics. Since arriving in February 2010, Dr. Waitman has conducted extensive interviews across our campuses to define a vision for biomedical informatics with clinical and translational research at the forefront. He has worked closely with Gregory Ator, MD (Chief Medical Information Officer, Senior Medical Director, and Professor of Otolaryngology), Chris Hansen (hospital Chief Information Officer), James Bingham (KUMC Chief Information Officer) and his Information Resources organization, Judith Warren, PhD, RN (Center for Health Informatics), Matthew Mayo, PhD, Chair of the Department of Biostatistics and his project management staff, and other informatics staff to establish medical informatics and a clinical data repository described in Aim 2 below. Dr. Ator participates in the Epic Corporation’s Research Council, ensuring our efforts are aligned with other academic medical center’s using the Epic clinical information system. Arvinder Choudhary is project director responsible for our clinical data repository. Mr. Choudhary was previously with the Medical College of Georgia and the University of Pittsburgh and has over 17 years of software engineering, database administration, and project management experience in healthcare and biomedical informatics. He previously constructed bio-surveillance data warehouses. Daniel Connolly is the biomedical informatics software engineer responsible for establishing the development environment and integration. For over 15 years, Mr. Connolly chaired the working groups defining technical standards for web and prototyped semantic web technologies at the Massachusetts Institute of Technology and the World Wide Web Consortium (W3C). Four additional personnel or faculty will be recruited as part of establishing the medical informatics division. Since April, the team has deployed a data repository with i2b2 integration, contributed to the i2b2 community code for integration with the Central Authentication Service (an open source project used by many universities for “single sign-on”), worked with other CTSA institutions to use the UMLS as a source terminology for i2b2, and established a software development environment for the team using Trac and Mercurial. B.2. Clinical Research Informatics Starting in 2005, KU selected Velos e-Research for our Comprehensive Research Information System (CRIS). CRIS is a web application, supports Health Level 7 messaging for systems integration, and complies with industry and federal standards (CFR Part 11) for FDA regulated drug trials. It consists of a management component for patients, case report forms, and protocols, and allows financial management for conducting studies with administrative dashboards and milestones for measuring research effectiveness. KU has invested over $2 million, with another $750,000/yr investment for support and staffing (6 research staff), to not only support KU investigators but also to provide enterprise licensing for HICTR investigators to conduct multicenter, cooperative group, and investigator-initiated research with CRIS across unlimited participating locations without additional license fees. CRIS has been deployed throughout our institution and the team has experience supporting multicenter trials as outlined in Table 3.1. In fiscal year 2010, CRIS was used to register 199 new studies, enroll 2331 new subjects, and enter data on 11,098 electronic case report forms. The CRIS team reports to Dr. Waitman and consists of three clinical information specialists, three clinical application administrators, and a information technology project manager. Approximately 2.5 FTE is devoted towards initiatives that expand clinical research informatics capabilities. Examples include deploying Velos financial management modules this year and working as a development partner with Velos to transform Institutional Review Board (IRB) review and approval into a paperless process. Investigators’ applications are validated in real time and then routed through the appropriate review mechanisms. This successful pilot will be integrated into the Velos product release in 2011 and our contribution to this eIRB initiative will benefit other organizations that have adopted Velos software. With the incorporation of financial and IRB tracking, CRIS provides greater capabilities to account for all research projects conducted in the enterprise. The KU Department of Biostatistics, in which the Division of Medical Informatics and CRIS reside, is also an alpha partner with Velos in developing a web-based project management system (eProject) for project registrations, tracking statuses, and creating budgets. Further details on CRIS and eProject operations are provided in the 2 Barohn, Richard J. Biostatistics section (Section 4). Additional planned CRIS initiatives (clinical data, administrative systems, and biological tissue repository integration) are discussed in the specific aims of this section below. Table 3.1. 2010 Examples of Trials using CRIS for Multi Site, Multi Sponsor, and Community Outreach Title PI Description (T1, clinical, T2) Phase II Trial of Methotrexate in Myasthenia Gravis Breast Cancer Prevention by Letrozole R. Barohn, Neurology Secoisolariciresinol (SDG) for Breast Cancer Prevention Enhancing Tobacco Use Treatment for African American Light Smokers Safety and Tolerability Trial of Arimoclomol for Sporadic Inclusion Body Myositis Azacitidine in newly diagnosed Acute myelogenous leukemia C. Fabian, Oncology Determine if oral methotrexate is an effective therapy for myasthenia gravis patients who are prednisone dependent. (FDA R01 FD003538-01) Multisite study Assess the potential efficacy of Letrozole as a chemopreventive agent in high risk postmenopausal women on hormone replacement therapy. (NIH CA122577-01A1) SDG (flax seed) as a prevention strategy for pre-menopausal women at high risk for developing breast cancer. Conducted in eight universities. (Komen Promise Grant) Evaluate the efficacy of bupropion plus health education versus placebo plus health education for smoking. Have enrolled over 540 participants. (NIH R01 CA091912-09) Assess the safety and tolerability of arimoclomol as compared with placebo over four months of treatment in patient with Inclusion Body Myositis. Multisite Kansas and London. (Sponsor: CytRx) Evaluate response rates of Azacitidine in elderly veteran population with untreated acute myelogenous leukemia (AML) where intensive chemotherapy is not appropriate. Department of Veterans Affairs multi-site study. (Sponsor: Celgene) Evaluate the pharmacokinetics, maximally tolerated dose, toxicities, and in a preliminary manner for any anti-tumor activity using RECIST criteria. (Sponsor: Crititech, Inc.) Create a registry of smokers in rural hospitals and examine the impact of a disease management program for smoking cessation. Conducted in 30 rural critical access hospitals. (NIH R01 CA101963-07) Phase I Study of Intraperitoneal Nanoparticle Paclitaxel Centralized Disease Management for Rural Smokers (KANQUIT II) C. Fabian, Oncology L. Cox, KUMC Preventive Med Y. Wang, Neurology S Kambhampati, KU Cancer Center S. Williamson, KU Cancer Center E. Ellerbeck, Preventive Med B.3. Bioinformatics Bioinformatics is a critical technology for translational (T1) research that systematically extracts relevant information from sophisticated molecular interrogation technologies. Analytical techniques–such as microarray experiments, proteomic analysis and high throughput chemical biology screening–can probe disease etiology, aid in development of accurate diagnostic and prognostic measures, and serve as a basis for discovering and validating novel therapeutics. HICTR institutions benefit from strong molecular bioinformatics research expertise distributed across three synergistic entities: the Center for Bioinformatics at KU-Lawrence (CBi), the Bioinformatics and Computational Life Sciences Research Laboratory (BCLSL), and the K-INBRE (Kansas IDeA Network for Biomedical Research Excellence) Bioinformatics Core (KBC). CBi (an internationally recognized structural biology modeling research program, focusing on computational structural biology) and BCLSL (a research program, led by the School of Engineering at KU-Lawrence and focusing on development of sophisticated algorithms for mining biological data) will be important HICTR collaborative partners. Examples of nationally funded research led by these two centers include: - Integrated Resource for Protein Recognition Studies, PI: I. Vakser; Improve understanding of fundamental properties of protein interaction and facilitate development of better tools for prediction of protein complexes. NIH R01GM074255-06, and - Mining Genome-wide Chemical-Structure Activity in Emergent Chemical Genomics Databases, PI: J. Huan; Advance the underlying theoretical and computational principles of data mining in the emergent chemical genomics databases. NSF IIS 0845951 3 Barohn, Richard J. Bioinformatics activities within HICTR will be coordinated by the K-INBRE KBC (an NCRR-funded multiinstitutional research support core serving basic and translational biomedical research in Kansas via computational resources, informatics consultation, collaboration and education). The KBC administers a broad range of bioinformatics software and data management utilities for biomedical researchers and strong computational hardware holdings are already in place. The BCLSL and KBC collaboratively led a successful $4.6 million NCRR G20 proposal (1G20 RR031125) aimed at enhancing a regional life sciences research data center, for which HICTR is a key target client. Gerald Lushington, PhD, who leads the KBC, will be the assistant director for bioinformatics within HICTR. Housed at KU-Lawrence, KBC has faculty-level satellite directors at KU medical center and Kansas State University. It employs three full-time PhD-level bioinformatics specialists for research support, plus a full-time bioinformatics outreach coordinator. KBC also partially supports five other staff positions and multiple graduate research assistants for bioinformatics research support. KBC has a strong background of successful collaboration with other molecular-oriented HICTR services such as those in the Translational Technologies Resource Center (Section 8) and the Institute for Advancing Medical Innovations (Section 6), an extensive collaborative network with experimental biologists, and a growing suite of clinical interactions. The KBC, in partnership with other bioinformatics entities, has a successful history of fostering biomedical program projects (see Table 3.2) and is well positioned to address T1 translational research needs for the HICTR. Table 3.2. Federally Funded Bioinformatics Program Projects and Centers Supported by the K-INBRE Bioinformatics Core and Collaborating Centers. Title PI COBRE Center for Cancer Experimental Therapeutics B. Timmerman, School of Pharmacy COBRE Center for Molecular Regulation of Cell Development and Differentiation COBRE Center for Nuclear Receptors for Liver Health and Disease D. Abrahamson, Anatomy & Cell Biology Kansas IDeA Network for Biomedical Research Excellence Kansas Intellectual and Developmental Disabilities Research Center KU Center for Chemical Methodology & Library Development J. Hunt, Anatomy & Cell Biology KU Program Project on Aging E. Michaelis, School of Pharmacy C. Klaassen, Pharmacology, Toxicology & Therapeutics P. Smith, Molecular & Integrative Physiology J. Aubé, School of Pharmacy Description of informatics provided to the research program collaboration with high throughput screening (HTS) Lab to develop a screening database (NIH P20 RR015563) collaboration to support post-microarray pathway identification, and bioinformatics services in SNP and copy number variations, epigenetics and microRNA (NIH P20 RR024214) bioinformatics support of microarray experiments and pathway analysis; chemical informatics support of high throughput screening experiments and lead optimization (NIH P20 RR021940) broad bioinformatics support of developmental and cell biology research across a network of 9 Kansas and 1 Oklahoma universities (NIH P20 RR016475) Informatics support of microarray experiments and pathway analysis (NIH P30 NICHD HD 002528) data mining techniques for prioritizing chemicals according to bioavailability, bioactivity against specific pharmacological targets, and data management (P50 GM069663) collaboration to facilitate prototype file sharing and tissue sample tracking systems in a newly funded program project grant (NIH NIH P01AG012993) B.4. Health Informatics The University of Kansas Center for Health Informatics (KU-CHI), established in 2003, is an interdisciplinary center of excellence designed to advance health informatics through knowledge integration, research, and education of faculty and students in the expanding field of biomedical science and information technology. Like many funded CTSA programs, KU is a founding member of the American Medical Informatics Association’s (AMIA) Academic Forum. Graduate health informatics education, continuing education, AMIA 10x10 program, consultation, and staff development workshops/seminars designed to advance health 4 Barohn, Richard J. informatics are sponsored or co-sponsored through KU-CHI. Graduate education in health informatics began in 2003 in the School of Nursing and is now a multidisciplinary master’s degree program offered by the Office of Graduate Studies and managed by the KU-CHI. Helen Connors, PhD, RN, FAAN (executive director of KUCHI) chairs the State of Kansas E-Health Advisory Council that oversees the development of the state’s health information exchange strategic and operational plans and is a board member of the Kansas City Bi-state Health Information Exchange, the metropolitan area’s Regional Health Information Organization. Dr. Waitman serves as the director of medical informatics for the KU-CHI. Under the direction of Dr. Ryan Spaulding, The University of Kansas Center for Telemedicine & Telehealth (KUCTT) is a leader in telehealth services and research. The program began in 1991 with a single connection to a community in western Kansas. The Kansas telehealth network now is used to connect 60 health facilities in Kansas each year. It also is the basis for several national and international collaborations, demonstrating significant potential of telehealth technologies to eliminate distance barriers. Over the last 19 years, nearly 30,000 clinical consultations have been conducted across numerous allied health, nursing and medical specialties, making the KUCTT one of the earliest and most successful telehealth programs in the world. In 2009, over 5000 Kansas patients benefited from telemedicine services that included clinical consultations, community education, health screenings and continuing education for health professionals. Through the Midwest Cancer Alliance (MCA) alone, the KUCTT supported numerous second opinion cancer consultations, multidisciplinary tumor board conferences, chemotherapy administration courses and routine patient consultations. Other specialties facilitated by the KUCTT include cardiology, psychology, psychiatry, neurology, wound care, etc. The KUCTT also has been very active integrating numerous technologies to support clinical and research activities, including telehealth systems, electronic health records, data registries and patient management systems. Examples of telemedicine support for clinical research is highlighted in Table 3.7 and in specific aim C.4.2. These core competencies will enhance HICTR and national CTSA activity. Judith Warren, PhD, RN, BC, FAAN, FACMI (Director of Nursing Informatics, the Center for Health Informatics) will serve as assistant director of health informatics for HICTR. She has extensive experience developing health informatics standards and terminologies, teaching informatics, and developing national policy for health information technology. Dr. Warren, a member of the National Committee on Vital and Health Statistics (NCVHS) since 2004, co-chairs the NCVHS Standards Subcommittee. She served on the task forces that developed the recommendations on the initial technical and functional requirements for the Nationwide Health Information Network (NHIN), recommendations on E-Prescribing, and observations on Meaningful Use. Dr. Warren also serves on the International Health Terminology Standards Development Organization’s Quality Assurance Committee and has been an active member of Health Level 7 (HL7) since 2000. Dr. Warren’s secondary appointment in the Department of Biostatistics has focused on aligning our clinical trials management with National Cancer Institute terminology standards defined by the cancer Biomedical Informatics Grid (caBIG). Dr. Warren’s involvement with the federal policy structure and extensive collaboration with Drs. Connors and Spaulding positions HICTR to exploit existing telemedicine capabilities and regional health information exchange developments, and to apply appropriate standards for communicating research findings nationally. Dr. Warren will lead our strong focus on use of standards to promote data integration and reuse. C. PROGRAM DESCRIPTION C.1. Aim #1: Provide a HICTR portal for investigators to access clinical and translational research resources and provide informatics consultative services. C.1.1. Establishing the portal and integrating resources. As shown as our first aim in Figure 3.1, we are developing a web application to link all HICTR research resources and foster communication among our investigators. It will provide investigators with direct access to the Translational Technologies and Resource Center, the Participant & Clinical Interactions Resources, the Community Partnership for Health, and the Clinical Research Development Office services. It also will allow investigators to identify potential collaborators, obtain targeted internal and extramural funding opportunities, address regulatory and institutional approval processes, request biostatistics support and clinical research database construction, request and access informatics resources, access national CTSA resources, and explore educational offerings. The user focused portal will be complemented by tools to help HICTR management track projects, distribute resources, and facilitate evaluation of the HICTR by analyzing user 5 Barohn, Richard J. activity similar to efforts at Vanderbilt University1. We will expand upon the web-based project management system (eProject2) that was been developed within the Comprehensive Research Information System (CRIS) to manage project registrations, track status, create budgets, and perform other management activities for biostatistics and clinical research database development. For further details on eProject capabilities, see the Biostatistics section (Section 9) of this application. Other components of the portal will build upon the Ingeniux content management system used by the medical center’s Information Resources and other collaborative tools such as wikis currently used by medical informatics for project management and the Personalized Medicine and Outcomes Center for www.cvoutcomes.org (Section 7). An overview of planned functionality is in Table 3.3. We will conduct yearly surveys of investigators to prioritize portal development. While developed by biomedical informatics, system hardware and administration is provided in-kind by KU Information Resources under the direction of James Bingham, Chief Information Officer. Figure 3.1 Conceptual Model of Biomedical Informatics and Specific Aims. In addition to the existing capabilities of the CRIS, there are several informatics specific components currently under development. We have integrated authentication between the portal, the campus Central Authentication Service, CRIS, and i2b2 to streamline access to eIRB and our clinical data repository described in Aim C.2 below. We are desiging secure methods for the process for submitting data requests and receiving data and complementary methods to support Data Request Oversight Committee activities. Additionally, the K-INBRE Bioinformatics Core (KBC) will help to promote awareness of regional bioinformatics resources and expertise by developing and maintaining a Bioinformatics Resources section of the portal. The Bioinformatics Resources section will clarify which core resource is best equipped to meet clinical and translational research needs and simplify the process of requesting bioinformatics services. Finally, we will provide a request management system for the informatics consult service described below. C.1.2. Create an informatics consultation service to identify investigators’ information needs. 6 Barohn, Richard J. We will match investigators’ needs against current information available in HICTR resources, specifically the new repository described in Aim 2. With CTSA funds we will add a clinical informaticist who understands clinical research hypotheses and knows what relevant data and clinical processes are in the repository. He/she will assist users with tools like i2b2 and will recommend alternative approaches when required data are not integrated. He/she will be knowledgeable about data resources described in the Personalized Medicine and Outcomes Center (Section 7). Early experience from front-line consulting with translational researchers will drive prioritizing additional data sources, terminology and ontology development (Aim C.2.3), and will guide the adoption of new technologies for data retrieval and analysis. The informaticist also will support translational (T2) research outlined in Aims C.4.3 and C.4.4. As our capabilities mature, the service will be staffed, and needs addressed, by the combined biomedical informatics personnel. Requests for bioinformatics and computational biology capabilities will be facilitated by the Bioinformatics Resources section of the portal and support by Dr. Lushington and the K-INBRE Bioinformatics Core. Personal interaction with the investigator will identify the best approach to their educational goals (formal educational offerings versus existing web based informatics educational materials developed by existing CTSA programs). Table 3.3. Examples of existing and planned modules for HICTR portal Module General HICTR Information Education Collaborator Connection Find Funding Pilot funding Request TTRC Resources Request CTSU Resources CRIS Biostatistics eIRB DROC HERON Informatics Consult Service Bioinformatics Resources IT support Telemedicine National CTSA Resources Description Maintained in Ingeniux by Clinical Research Development Office Status Planned Connect to offerings provided by the Clinical and Translation Research Education Center and other Centers (e.g. K-INBRE) Integration with Dykes Library “meet the experts” Bibapp application to allow investigators to identify potential collaborators locally and NIH VIVO project for national networking for scientists. Collect and organize funding announcements. Allow investigators to subscribe to keyword tailored updates. Submit pilot projects to HICTR for review and funding. Integration with Translational Technologies Resources Center (TTRC) request management systems as well as NIH EAGLE-I project for national resources. Integration with existing web site to request Clinical Translational Science Unit (CTSU) services and resources. Access Comprehensive Research Information System for accessing protocol management system, case report forms, and reporting. Request collaboration, obtain status, and management by eProject Submit protocols and applications to institutional review board. Investigators can also check on the status of their application. Request data access to de-identified clinical repository. de-identified clinical data repository Request assistance with information needs; using HERON, CRIS, and Bioinformatics Resources Detailed inventory of capabilities and expertise in the region with links to request systems used by the individual cores. Request network attached storage, wiki or Sharepoint from Information Resources Request telemedicine services for research purposes Researchmatch.org, www.vivo.org, www.eagle-i.org. Planned Existing Planned Planned Existing Existing Existing Existing Existing Planned Existing Planned Planned Existing/ Planned Existing Existing C.2. Aim #2: Create a platform, HERON (Healthcare Enterprise Repository for Ontological Narration), to integrate clinical and biomedical data for translational research. 7 Barohn, Richard J. Transforming observational data into information and knowledge is the cornerstone of informatics and research. The opportunity for data driven knowledge discovery has exploded as health care organizations embrace clinical information systems. However, when dealing with confidential patient information, science and technology are dependent on law, regulation, organizational relationships, and trust. HERON provides HICTR with secure methods for incorporating clinical data into standardized information aligned with national research objectives. It facilitates hypothesis generation, allows assessing clinical trial enrollment potential, and minimizes duplicate data entry in clinical trial data capture, outcomes research, and evaluation of T2 interventions for translating research into practice. While initially focused on integrating data between the KU Medical Center, the KU Hospital, and KU affiliated clinics, our methods are designed to subsequently integrate information among all HICTR network institutions. C2.1. Develop business agreements, policies, data use agreements and oversight. Beginning in April 2009, the HICTR started piloting a participant registry in the clinics which allows patients to quickly consent to be contacted by clinical researchers. The registry contains the consented patients’ demographics, contact information, diagnoses, and procedure codes. From April to July 2010, the medical center, hospital and clinics reviewed comparable practices4,5,6,7 and drafted a master data sharing agreement between the three organizations that was signed September 6, 2010. The HERON executive committee is composed of senior leadership (e.g. chief operating, financial, executive officers and chief of staff) from the hospital, clinic and medical center and provides governance for institutional data sharing. Establishing business processes and servicing research requests is conducted by the Data Request Oversight Committee(DROC) which reports to the HERON executive committee. The repository’s construction, oversight process, system access agreement, and data use agreement for investigators were approved by the Institutional Review Board. Since HERON is currently funded by the KU and contains medical center and affiliated clinics and hospital data, access requires a medical center investigator. As additional institutions and health care organizations provide support and contribute data, they will be incorporated with multi-institutional oversight provided by the HERON executive committee and DROC. As agreed upon by the HERON executive committee, HERON has four uses: cohort identification, de-identified data, identified data, and participant contact information: 1. After signing a system access agreement, cohort identification queries and view-only access is allowed and activity logs are audited by the DROC. 2. Requests for de-identified patient data, while not human subjects research, are reviewed by the DROC. 3. Identified data requests require approval by the Institutional Review Board prior to DROC review. After both approvals, medical informatics staff will generate the data set for the investigator. 4. Investigators who request contact information for cohorts from the HICTR Participant Registry have their study request and contact letters reviewed for overlap with other requests and adherence to policies of the Participant and Clinical Interactions Resources Program Data Request Committee. C.2.2. Implement open source NIH funded (i.e. i2b2) initiatives for accessing data. The utility of data for clinical research is proportional to the amount of data and the degree to which it is integrated with additional data elements and sources. However, as additional data are integrated and a richer picture of the patient is provided, privacy concerns increase. HERON receives and preserves data into an identified repository, links and transforms those data into de-identified, standardized concepts, and allows users to retrieve data from this separate de-identified repository (Figure 3.2). We recognize that certain research requires access to identified data but our approach streamlines oversight when needs are met with de-identified data. We have adopted the NIH funded i2b28 software for user access, project management, and hypothesis exploration. We have chosen Oracle as our database because of existing site licensing and i2b2 compatibility. Transformation and load activities are written in the python language and deployed onto SUSE LINUX servers. Servers are maintained in the medical center and hospital’s data center which complies with HIPAA standards for administrative, technical and physical safeguards. Access to the identified repository is highly restricted and monitored. Data exchange between source systems, HERON, and user access is handled via security socket layer communications, https with digital certificates, and 128-bit or higher public key cryptography (ex: SSH-2). We will continue to monitor federal guidance regarding appropriate security measures for healthcare information14. User access, activity logs, and project management for the de-identified repository is managed via the i2b2 framework and is integrated with the medical centers’ open source Jasig Central Authentication Service and the HICTR portal. Account creation 8 Barohn, Richard J. and access control is provided by the medical center. Audit logs are maintained for both the identified and deidentified repositories. Intrusion detection mechanisms are used and monitored by medical center Information Resources security personnel who also conduct HIPAA Security Rule reviews of the systems. Current literature highlights challenges with providing anonymity after de-identifying data9,10,11,12. While we remove all 18 identifiers to comply with HIPAA Safe Harbor, the de-identified repository is treated as limited data set, reinforced by system access and data use agreements. Dr. John Keighley, Assistant Professor in Biostatistics, will provide statistical guidance regarding de-identification methods and re-identification risk. He has done similar work with the Kansas Cancer Registry. Initially, HERON will only incorporate structured data. We will stay abreast of best practices (e.g., De-ID, the MITRE Identification Scrubber Toolkit versus only extracting concepts) prior to incorporating narrative text results which have greater risk for re-identification9,13. Figure 3.2. HERON Architecture Pilot use of HERON and i2b2 for the HICTR Participant Registry began in April 2010. The current architecture was deployed in August 2010 and populated with production data from IDX and Epic in September 2010. Initial extract, load, and transform processes obtain data files from the source system via secure file transfer methods. Over time, we will increase the frequency for incorporating source data, such as event driven HL7 listeners. This will facilitate data integration with the Comprehensive Research Information System. C.2.3. Transform data into information using the NLM UMLS Metathesaurus as our vocabulary source. From its inception, HERON has benefitted from i2b2 community expertise and will continue to work with other academic medical centers to align our terminology with CTSA institutions. Led by Dr. Warren, our approach is to rely on the National Library of Medicine Unified Medical Language System (UMLS) as the source for ontologies and to use existing or develop new update processes for the i2b2 Ontology Management Cell and other systems. The National Center for Biological Ontologies will augment the UMLS to bridge clinical data towards bioinformatics domains and to incorporate more recently authored ontologies that are not fully supported by the NLM. As we develop new mappings for going from UMLS into i2b2 and other systems, we will share our code and processes with the i2b2 community. Using i2b2 and the UMLS will streamline the HICTR’s ability to participate in national interoperable data exchange initiatives. Current and planned activities are shown in Table 3.4. We anticipate refining ontologies based on investigator feedback. We are currently evaluating an approach outlined by several CTSA organizations that shifts mapping inside i2b2 instead of in database transformation and load processes15. This preserves the original data side by side with the transformed information allowing easier review by investigators and domain experts. Standardizing information for research strengthens our relationship with the hospital and clinics. Reusing information for clinical quality improvement also requires standardization. Translational research using HERON highlights areas needing terminological clarity and consistency in source systems. Research and quality improvement goals also align with achieving “meaningful use”16 and Health Information Exchange activities. Dr. Warren will partner with Dr. Ator, Chief Medical Information Officer, and the University of Kansas 9 Barohn, Richard J. Hospital’s Organizational Improvement (which has two of their leaders on the DROC) to develop a data driven process for improving standardization. This process will be aided by Dr. Ator and the hospital’s foresight in purchasing and integrating IMO® Problem(IT) into the Epic Electronic Medical Record to support accurate collection of observations based on both ICD-9 and SNOMED CT. Table 3.4. Terminology activities Source terminology Demographics: i2b2 Extract Status Complete Completed planned April 2010 Notes caBIG: CTEP Synced October 2010 Diagnoses: ICD9 Procedures: CPT Complete Complete April 2010 June 2010 Lab terms: LOINC Medication terms: RxNorm Planned Planned November 2010 November 2010 Medication ontologies: NDF-RT Nursing Observations Planned December 2010 Ongoing July 2010- Pathology: SNOMED CT Planned February 2011 Clinical narrative Planned 2012 National Center for Biological Ontology Planned 2013 Using i2b2 hierarchy. Restricted search criteria to geographic regions (> 20,000 persons) instead of individual zipcodes Clinical Research forms for demographics, adverse event reporting, and disease progression. (Drs. Warren, Mayo, Waitman) Using i2b2 hierarchy UMLS extract scripts developed with UTHSC at Houston Plan to use i2b2 hierarchy UMLS derived. Used to map between Medispan/FDB, NDF-RT, and Multum used by current outcomes databases (Section 7). Physiologic effect, mechanism of action, pharmacokinetics, and related diseases. NDNQI pressure ulcers mapped to SNOMED CT to evaluate automated extraction of self reported activity. (Drs. Dunton and Warren.) Providing coded pathology results and patient diagnosis is a critical objective for defining cancer study cohorts in Aim 3. As the hospital restructures clinical narrative documentation to use Epic’s SmartData (CUI) concepts, will determine appropriate standard. In support of Aim 3 focus on bridging clinical and bioinformatics to advance novel methods. C.2.4. Link clinical data sources to enhance their research utility. Data sharing is a very sensitive concern among healthcare providers. We will gradually build relationships by initially focusing on linking data sources from KU Hospital and affiliated clinics. As capabilities of the team develop we will expand to other HICTR affiliated network institutions, state agencies, and our rural practice networks (outlined in C.4.4). This may require centralized and/or distributed data integration17,18. For example, Dr. Theresa Shireman, head of the Large Database Analysis Core of our Novel Methods 2 section, conducts research with Medicaid administrative claims data. We will work with her, the Kansas Health Policy Authority, the Kansas Health Information Exchange, and the Kansas City Bi-state Health Information Exchange to link clinical databases and state administrative data for research. KU institutional support will be used to construct and maintain HERON with planned data sources (see Table 3.5 which also shows preliminary statistics on the volume of data currently extracted). Data from additional sources will be integrated depending on research interest and support. Table 3.5 Timeline for Incorporating Clinical Data Sources into HERON Data source Source System HICTR Participant Registry IDX System “Go-Live” Date 2009 10 Extract Status Complete Data extraction target and prelim statistics April 2010 3173 volunteers Barohn, Richard J. Data source Source System Inpatient/Emergency demographics, “ADT” locations & services Epic Inpatient Diagnoses (ICD9) Epic 2006 In progress Laboratory Results and other Discrete Results (inpatient/outpatient) Epic/Misys 2002 backfilled In progress Electronic Medication Administration Epic 2007 Planned Outpatient visits services, diagnoses, procedures (beyond HICTR Registry) IDX/Epic 2002 In progress for IDX Vital signs, inputs, outputs and discrete nursing observations Epic 2007 Planned Clinical Research Information System Integration Provider Order Entry Other Elements of Patient Problem List Microbiology, Cardiology, Radiology CRIS 2007 Planned Epic Epic Epic/Misys Theradoc Epic NDNQI 2010 2009 2006 Planned Planned Planned 2007 2001 Planned Planned 2011 2011 2011 637,000 micro orders 2011 2011 Epic ORSOS SSDI Phillips and Datacaptor KHPA 2009 2005 Na 2007 Planned Potential Potential Potential 2012 2012 2013 2013 2005 Potential 2013 Medication reconciliation Nursing Unit Quality Indicators Provider Notes (discrete elements) Perioperative schedule and indicators Social Security Death Indicator Dense physiologic signals Medicaid databases integration System “Go-Live” Date 2006 Extract Status In progress Data extraction target and prelim statistics October 2010 1.8 million patients October 2010 215,000 inpatient November 2010 1.4 million serum K 67 million overall December 2010 1.2 million outpt orders 2.5 million inpt orders November 2010 214,000 outpt ICD9 from Epic 2011 1 million patient days 265 million total 6 million pulse 2011 C.3. Aim #3: Advance medical innovation by linking biological tissues to clinical phenotype and the pharmacokinetic and pharmacodynamic data generated by research in phase I and II clinical trials (addressing T1 translational research). We see two points where HICTR informatics must bridge between basic science resources and clinical activities to enhance our region’s ability to conduct translational research. Our region provides a wealth of biological and analytical capabilities but struggles at times to understand if our clinical environments see enough patients to support research. This leads to clinical trials which fail to accrue enough subjects19. Accurately annotating biological tissues and routine clinical pathology specimens with the patients’ phenotypic characteristics (such as diagnosis and medications from the clinical records) will provide a more accurately characterized clinical research capacity. Our second targeted area is designed to support the Drug Discovery and Development activities of the HICTR Novel Methods 1 program (Section 6) in managing information in phase I and II clinical trials. Molecular biomarker (Section 8) and pharmacokinetics/pharmacodynamics research activities (Section 9) provide high quality analysis but their results are not easily integrated with other records maintained in clinical research information systems. Reciprocally, if clinical characteristics could be provided with samples in a standardized manner it would allow improved modeling and analysis by the core laboratories. Collaboration between the bioinformatics and biomedical informatics specifically targeted at 11 Barohn, Richard J. pharmacokinetic/pharmacodynamic results and clinical trials will provide a foundation for subsequent integration and our final goal of providing molecular bioinformatics methods. C3.1. Incorporate clinical pathology and biological tissue repositories with HERON and CRIS to improve cohort identification, clinical trial accrual, and clinical trial characterization. Patients’ tissue specimens are a fundamental resource that links the majority of basic biological science analysis to clinical relevance. We need to improve our characterization of these samples to maximize our investment in maintening them for clinical research. By integrating routine clinical pathology and research specimens with clinical information in HERON researchers can quantify samples belonging to patients (e.g. aggregating all breast cancer diagnoses using the i2b2 a clinical concept “malignant neoplasm of the breast” and treated with the adjuvant therapy trastuzumab). Similarly, integration between the Biological Tissue Repository (BTR) in the Translational Technologies and Resource Center (Section 8) and the Comprehensive Research Information System (CRIS) will enhance analysis and characterization of data from clinical trials. The BTR builds upon the existing KU Cancer Center Biospecimen Shared Resource and plays a vital role in collecting and distributing high quality human biospecimens essential to research. Improving specimen management for clinical research has been identified as a high priority initiative for KU. Working with Ossama Tawfik, MD, PhD, director of the BTR, we will evaluate the new capabilities provided by Velos eSample and the National Cancer Institute’s caBIG caTissue initiative to modernize information management in the BTR. This work will be performed in-kind as a biomedical informatics initiative. We also will work with Dr. Tawfik in his role as the director of surgical pathology to integrate clinical pathology reports into the HERON repository. Source systems for this information will be Cerner CoPath and the Epic clinical information systems. We will exploit current SNOMED CT encoding of pathology results as our standard terminology. Additionally, the K-INBRE bioinformatics core will interact closely with biomedical informatics and biostatistics to evaluate the viability of proposed biomarker studies according to fundamental criteria such as whether enough participating patients or tissue samples exist under a suitable range of conditions or phenotypic characterization to form an adequate basis for meaningful analysis. C3.2. Support IAMI clinical trials by integrating and standardizing information between the bioinformatics and pharmacokinetic/pharmacodynamic (PK/PD) program and CRIS. As described in the Novel Methods 1 and PK/PD sections of this application (Section 6, 9), the Institute for Advancing Medical Innovation (IAMI) builds upon the region’s significant drug discovery capabilities and creates a novel platform for medical innovations. Dr. Gerald Lushington, Dr. Mahesh Viswanathan, and the KINBRE Bioinformatics Core (KBC) provide bioinformatics analysis across the spectrum of target discovery, compound screening, lead identification and optimization, and preclinical development. In developing these bioinformatics resources, KBC adheres to international data standards (e.g., Minimum Information About a Microarray Experiment, MIAME) to ensure consistent data format and content. These resources include references to publicly available annotation sites (e.g., as provided by National Center for Biotechnology Integration) in order to amplify the informational content of the stored data. As candidates successfully transition to a new investigational drug application, we will continue bioinformatics support into clinical trials. The KBC, the IAMI, the PK/PD program, the CRIS team, and the new clinical research building will provide the region with a state of the art environment to advance drug discovery. Collaboration between bioinformatics and the CRIS team will improve the integration of data collected during trials by the clinical research team and the analytical results generated from histology and chemistry studies. This work will be catalyzed by Drs. Timothy Welty, Greg Reed, and Maxine Stolz from the PK/PD program. Dr. Lushington and the KBC will ensure that the data and knowledge associated from the above studies is integrated into standardized format and made available for general use by both clinical and basic science collaborators. C.3.3. Apply molecular bioinformatics methods to enhance T1 translational research in areas such as molecular biomarker discovery efforts and pharmaceutical lead optimization. Establishing stronger bridges between analytical resources and clinical information allows phenotypic variables to be exploited by bioinformatics expertise in data mining by the K-INBRE Bioinformatics Core (KBC) and the Bioinformatics and Computational Life Sciences Research Laboratory. We will augment HICTR T1 translational research efforts by providing data mining algorithms that extract key information from dataintensive wet lab studies and information specification standards that enable systematic and comprehensible reporting of such information for clinical applications. KBC also has developed a number of tools that facilitate basic and clinical scientists’ ability to interact and experiment with the data. For example, KBC developed 12 Barohn, Richard J. OmicsMiner20 which encodes a broad range of machine learning and statistical techniques for feature selection, phenotype classification and molecular biomarker validation into an intuitive (i.e., non-intimidating) but comprehensive first-approach data processing engine. OmicsMiner is an open-source, platformindependent, context-insensitive analysis suite that has been applied to microarray profiling, miRNA analysis, proteomic peak assignment, bioavailability predictions, and next generation sequencing read counts analysis. This bridge between molecular-level analysis and clinical studies is a potent model for biomarker prediction and validation, PK/PD studies, and the prospective refinement of personalized medicine. KBC has already collaborated with the K-INBRE Partnership Core to promote the availability of our translationally-oriented systems biology skills to collaborative teams of basic and clinical scientists. Both the K-INBRE Partnership Core and the HICTR Translational Discovery Forums provide rich opportunities for bringing basic and clinical scientists together, a key HICTR goal. In its current K-INBRE-funded mission, the KBC employs a combination of explicit salary support from grants for large-scale collaborative or developmental efforts and fee-for-service cost recovery for small-scale activities. This model will be extended for the HICTR, with HICTR salary support provided for development of the PK/PD integration and fee-for-service for efforts specifically targeted toward a distinct translational project (e.g., biomarker discovery, chemical screening data analysis, basic consultation, etc.) While nationally recognized for achievement in basic biological sciences, the KBC has increasingly focused on translational activities. As such, the KBC has led the way in developing, acquiring, and implementing many of the bioinformatics resources currently available to HICTR investigators. A selection of recent (i.e., 2010) biomarker identification efforts and IAMI-supported projects are shown in Table 3.6. Table 3.6 Recent Biomarker identification and IAMI-supported projects Title PI MiRNA Regulation of Ovarian Function L. Christenson KUMC; co-I: O. Tawfik, KUMC Human Lung Cancer Biomarker Identification Using Informatics and Clinical Samples M. Visvanathan KBC; co-I: G.S. Sittampalam, IAMI; co-I: O. Tawfik, KUMC Development of BRCA1 expression promoters for breast cancer therapy and prevention L. Harlan Williams KU Cancer Center Oxidative defense against CYP2e1 toxicity via Keap1Nrf2 interaction blockers C. Klaassen KUMC Pharmacology, Toxicology & Therapeutics J. Barycki; U. Nebraska Dept. of Biochemistry K. Peterson; KUMC Department of Biochemistry G.S. Sittampalam; IAMI Prostate cancer treatment via UGDH modulation Sickle cell anemia therapeutic development via HbF upregulation promoters Colon cancer treatment via Wnt – Beta Catenin modulators Early Detection of Shock using Biomarker predictors C. Van Way University of Missouri Kansas City Description of informatics services provided to the research program Applies miRNA analysis and advanced machine learning algorithms to identify molecular biomarkers relevant to female reproductive health disorders based on clinical ovarian tissue and serum samples R01HD61580 KUCC Pilot Award for collection of clinical samples addressing four distinct lung carcinoma phenotypes, followed by genomic profiling and lung cancer molecular biomarker identification and validation via sophisticated machine learning algorithms high throughput screening (HTS), data mining, quantitative structure-activity-relationship (QSAR) modeling, analog identification and lead optimization, leading to promising lead and pending patent (20090170842) HTS data mining, QSAR modeling, analog identification and early-stage lead optimization HTS data mining and hit prioritization HTS data mining, QSAR modeling, analog identification and early-stage lead optimization hit analog identification and prioritization Microarray technology to identify early changes in gene expression in white blood cells that will predict favorable and unfavorable outcomes. DoD: ONR 13 Barohn, Richard J. N00014-01-1-0151; USAMRIC, W81XSH-06-1-530 We anticipate connections cultivated by the HICTR that prompt integration of bioinformatics and clinical informatics will also promote collaboration between clinical and basic researchers with data mining expertise. C.4. Aim #4: Leverage an active, engaged statewide telemedicine and Health Information Exchange (HIE) to enable community based translational research (addressing T2 translational research). 2010 will be seen as a landmark year for KU, the region, and the nation for health information technology adoption. The University of Kansas Hospital will have completed a five-year plan to implement the Epic Electronic Medical Record. Through the HICTR Personalized Medicine and Outcomes Center (Section 7), the Patient Risk Information Services Manager (PRISM; see C.4.6) developed by John Spertus, MD, and colleagues at St. Lukes Mid-America Heart Institute will be available for widespread use. Kansas and Missouri have established health information exchanges and regional extension centers. The Kansas Health Policy Authority has invested in and deployed a Data Analytic Interface (DAI) maintained by Thomson Reuters that provides a portal to more than five years of claims data from Medicaid, state employee health plans, and other private insurers. Cerner Corporation has increased the number of participating institutions in their HealthFacts repository to encompass 24 million lives, 178 million medication orders on 5,945 brand name drugs, and 1.5 billion lab results from general lab and microbiology. HealthFacts has also integrated EMR data elements such as vital signs, chief complaint, symptoms, and pain assessment with existing medication and laboratory data. These regional informatics capabilities are complemented by a long history of engaging the community through outreach via telemedicine, continuing medical education, and our extensive community research projects in urban rural and frontier settings. C.4.1. Provide health informatics leadership to ensure state and regional healthcare information exchange (HIE) and health information technology initiatives foster translational research. Under the leadership of Dr. Helen Connors, the Center for Health Informatics has been instrumental for advancing HIE for Kansas and the Kansas City Bi-state Health Information Exchange (KCBHIE). As chair of the eHealth Advisory Council, Dr. Connors guided the process to establish the Kansas HIE (KHIE)21; a nonprofit corporation incorporated by the governor in response to the federal HITECH Act. On September 2, 2010, the governor appointed Dr. Connors as a founding member of the KHIE board of directors. Allen Greiner, MD, director of the Community Partnership for Health (Section 5), participates in selecting electronic health records for the Kansas Regional Extension Center. Dr. Russ Waitman participates in coordinating exchange activities for outcomes research in underserved populations managed by the Kansas Health Policy Authority (responsible for Kansas Medicaid). In-kind participation in these activities by Drs. Connors, Greiner and Waitman will keep the HICTR engaged in state and regional infrastructure capabilities for translational research and will facilitate identifying other collaborating organizations. C.4.2. Promote existing telemedicine and clinical research informatics capabilities to conduct research in critical access hospitals and rural regional referral centers. As described in our background, and in the community engagement section (Section 5, Figure 5.2), the Center for Telemedicine and TeleHealth (KUCTT) provides enormous reach into diverse communities for implementing clinical trials and other research across the state. Telemedicine has figured prominently in a number of clinical research programs (e.g. studies of diagnostic accuracy, cost effectiveness, and patient and provider satisfaction with telemedicine) as well as studies that employ telehealth for randomized control trial interventions (e.g. for home parenteral nutrition and sleep apnea.) Complementing KUCTT, the Midwest Cancer Alliance (MCA) is a membership-based organization bringing cancer research, care and support professionals together to advance the quality and reach of cancer prevention, early detection, treatment, and survivorship in the heartland. The MCA links the University of Kansas Cancer Center with the hospitals, physicians, nurses and patients battling cancer throughout Kansas and Western Missouri. The MCA advances access to cutting-edge clinical trials as well as professional education, networking, and outreach opportunities. These clinical trials use our Comprehensive Research Information System (CRIS). Notably, the MCA critical access and rural referral centers are also the most active participants in telemedicine. The medical director of the MCA, Dr. Gary Doolittle is a pioneer user and has published telemedicine research with Dr. Ryan Spaulding, the director of the telemedicine network22,23. The network has been successfully used to facilitate clinical research and to support special needs populations (see Table 3.7). Especially in the area of smoking cessation, studies are already benefiting from the complementary technologies of telemedicine and CRIS. In 14 Barohn, Richard J. addition to statewide integration, as a national leader in telehealth operations, technology and research, Dr. Spaulding is well-positioned to support CTSA research activities and collaborations across the U.S. and world using the latest telehealth technologies. Dr. Spaulding has previously partnered with Internet2 leadership on the Federal Communication Commission’s Rural Healthcare Pilot Project and will leverage these relationships to advance research activities. Internet2 is a nationwide, high bandwidth network linking universities for research and data-sharing capabilities. It will be available to HICTR leadership via Dr. Spaulding’s efforts. Biomedical informatics will work with KUCTT to provide a telemedicine clinical trials network connected by CRIS for remote data collection via study personnel or direct data entry through a patient portal. KUCTT also will provide in-kind support for HICTR investigators using telemedicine for meetings across the region. Table 3.7 Grant Examples using Telemedicine and the Comprehensive Research Information System Title PI Grant/Agency CRIS used? Describing and Measuring Tobacco K. Richter R21DA020489, National Institute on Yes Treatment in Drug Treatment Drug Abuse Telemedicine for Smoking Cessation K. Richter R01HL087643, NIH National Heart, Lung No in Rural Primary Care and Blood Institute Using CBPR to Implement Smoking C. Daley R24MD002773, National Center on Yes Cessation in an Urban American Minority Health and Health Disparities Indian Community Centralized Disease Management for E. Ellerbeck R01CA101963, National Cancer Institute Yes Rural Hospitalized Smokers Pediatric epilepsy prevalence study D. Lindeman RTOI # 2008-01-01 AUCD, National No Center for Birth Defects and Developmental Disabilities, CDC Kansas Comprehensive Telehealth E-L Nelsen, L. Health Resources and Services No Services for Older Adults Redford Administration Office for the Advancement of Telehealth C4.3. We will “wire” the University of Kansas Hospital and clinic information systems to provide a laboratory for translational informatics research. Figure 3.4 provides a timeline for University of Kansas Hospital and associated clinics Epic clinical information system implementation. Working with Dr. Gregory Ator, we will build upon this investment by consulting with HICTR investigators to optimize the use of clinical systems for disseminating translational evidence and recording measures to verify adoption. This work is also foundational to medical informatics and will allow the evaluation of native clinical information system “signals” against manual processes used to report measures to government, regulatory agencies, and national registries. Working with the hospital to develop capabilities to acquire user activity data to measure the systems’ impact on workflow and clinical decision making (e.g. drugdrug interaction overrides, time to complete medication administration task) will also help us overcome translational research’s last mile: implementation into clinical workflow. Preliminary analysis indicates that many measures already exist in Epic Clarity audit tables, though we realize this goal may require developing custom messages using Epic “Bridges” functionality. 15 Barohn, Richard J. Figure 3.4. Epic rollout timeline expands T2 capabilities C.4.4. We will develop methods to directly engage with community providers regarding EHR adoption and explore their systems capabilities as a platform for translational research. While the University of Kansas leadership is partnering with state agencies to shape regional policy regarding health information exchange and electronic health record adoption, those activities primarily focus on adoption, incentives, and external requirements as opposed to investigator-initiated research. However, there is a unique alignment between existing health services research in underserved populations with the core mission of the Kansas Health Policy Authority (KHPA is responsible of Medicaid in Kansas). Implementing a medical home for all Medicaid recipients is a primary goal for the State Medicaid HIT Plan (SMHP). We will work with Dr. Allen Greiner (director of the HICTR Community Partnership for Health Program) and Dr. Theresa Shireman (leading the Medicaid databases section of the HICTR Personalized Medicine and Outcomes Center), the state Regional Extension Center, and members of the Kansas Physicians Engaged in Practice Research (KPEPR) Network24 to pilot connections between rural clinical systems and HERON to evaluate clinical research in rural settings. This will benefit rural practices as our combined expertise will help tune electronic health records (EHR) for meaningful use. We will determine the adopted clinical systems’ capacity to deliver evidence-based medicine and promote the medical home approach to primary care. We also will provide i2b2 to researchers and clinicians working with underserved populations. Our targeted evaluation will help define research requirements in rural practices and inform the Kansas and bi-state health exchanges. C.4.5. We will enhance data maintained by the state, national registries, and regional collaborators. Informatics will stay abreast of the database resources in our Novel Methods 2 section. We will work with those resources and investigators to create capabilities to enrich each data source by linking to additional clinical information from HERON. Kansas has made significant progress with its multi-payer database (Data Analytic Interface or DAI) - an ambitious technology infrastructure initiative to consolidate and manage health care data for several public and private insurance programs. DAI includes the Medicaid Management Information System (MMIS), the State Employee Health Program (SEHP), and the Kansas Health Insurance Information System (KHIIS.) It allows analysis of health care based on episodes of treatment, disease management, predictive modeling, and cost and outcome effectiveness measures. The Medicaid and SEHP modules have been successfully integrated and launched in January 2010 with KHIIS integration expected to be completed by first quarter 2011. Preliminary comparative pricing and utilization reports on pharmacy, durable medical equipment, physician services, hospital inpatient services, and dental services have been publicly shared with the Kansas Health Data Consortium – a multi-stakeholder advisory committee of key government agencies, hospitals, physicians, insurers, purchasers, and consumers convened by the Kansas Health Policy Authority to leverage the state’s data for health reform via data-driven policy recommendations. We will adopt methods for distributed data integration between such datasets and clinical information systems as outlined in C.2.4 above. This will further three objectives: (a) national data may provide outcome measures lacking in acute care clinical information systems, (b) national registries, such as the National Database of Nursing Quality Indicators, can evaluate the degree to which manually abstracted measures might be 16 Barohn, Richard J. automatically derived from a mature clinical information system, and (c) data integration will allow hypotheses to be explored that suggest methods for improving care. C4.6. We will collaborate with the HICTR Personalized Medicine and Outcomes Center to provide complex risk models for decision support to a variety of clinical specialties. As described in the Novel Methods 2: Personalized Medicine and Outcomes Center (Section 7), regional investigators have developed the Patient Risk Information Services Manager (PRISM): software that translates complex risk models into fully functional decision-support tools for physicians as well as personalized educational and informed consent documents for patients. Though initially deployed and evaluated in cardiology (R01 HL096624 Transforming PCI Informed Consent into an Evidence-Based Decision Making Tool), this approach has direct applicability to other clinical specialties. As investigators develop validated statistical models, biomedical informatics will work in consultation with Dr. Spertus and his colleagues to deploy PRISM into practice and evaluate its adoption and effectiveness. In year three, our inpatient clinical informatics capabilities will have matured so that we may evaluate integration of PRISM risk modeling into other clinical workflows such as inpatient Computerized Provider Order Entry provided by Epic. D. STRUCTURE, GOVERNANCE, AND CTSA INTEGRATION D.1.Structure and governance. Russ Waitman, PhD will direct the overall biomedical informatics key function. Drs. Lushington and Warren will lead and coordinate bioinformatics and health informatics activities respectively, as assistant directors. Their expertise and qualifications were described in the Background section. Dr. Waitman will meet with the assistant directors on a bi-weekly basis to discuss issues and go over project statuses. He will determine support for each component through an annual review with the assistant directors. Dr. Waitman will report to the HICTR director and be an active member of the HICTR Leadership Team. If he cannot attend, Dr. Warren or Dr. Lushington will attend in his place. Dr. Waitman will represent HICTR at the CTSA Informatics Steering Committee. Biomedical informatics requires collaboration across multiple groups at the University of Kansas medical center, KU hospital, and HICTR affiliated network institutions. The HERON Executive Committee (shown in Table 3.8) will provide guidance for institutional data sharing. Our rapid success implementing change has been due to Dr. Waitman’s leadership and work with this group. The HERON Executive Committee will engage the HICTR Leadership Team, Deans Council, Community Council, and Health Systems Leadership Council regarding expansion. To achieve our informatics objectives for the medical center, Dr. Waitman will use a working group composed of: Shelley Gebar, MPH, Senior Associate Dean for Operations; Karen Blackwell, MS, Director of our Human Research Protection Program; Matthew Mayo, PhD, Chair of the Department of Biostatistics; Richard Barohn, MD, HICTR Director; Gregory Ator, MD, hospital Chief Medical Information Officer and Senior Medical Director; Chris Hansen, hospital Chief Information Officer; and James Bingham Associate Vice Chancellor for Information Resources and Chief Information Officer. Table 3.8 HERON Executive Committee Name Title Organization Paul Terranova Shelley Gebar Vice Chancellor for Research Chief of Staff and Senior Associate Dean for Operations Director of Medical Informatics Executive Vice President and Chief Operating Officer Executive Vice President and Chief Financial Officer Senior Vice President for Ambulatory Services and Chief Information Officer President Chief Executive Officer Chief Operating Officer University of Kansas Medical Center University of Kansas Medical Center Russ Waitman Tammy Peterman Scott Glasrud Chris Hansen Kirk Benson Jim Albertson Teresa Neely D.2. Data and Software Sharing. 17 University of Kansas Medical Center University of Kansas Hospital University of Kansas Hospital University of Kansas Hospital University of Kansas Physicians University of Kansas Physicians University of Kansas Physicians Barohn, Richard J. The HICTR will adhere to NIH guidelines on data sharing. We will make scientific data available as widely as possible while safeguarding the privacy of our participants and protecting confidential or proprietary data. As described in Aim 2, we have developed data sharing agreements at an organizational level to streamline requests for de-identified data. Our repository’s use of i2b2 and UMLS terminologies should facilitate national collaboration. Because of the risk for re-identification using even de-identified data, our system access and data use agreements reinforce the investigator’s responsibilities as custodians of patient data to prevent improper disclosure. The informatics consultation service will assist investigators with data sharing and with providing meta-data to identify the data and the methods used in data processing. Data generated from microarray experiments will be posted by investigators on publically accessible databases (e.g. NCBI with MIAME compliant meta-data). All new software developed using support from this grant will be available to others using open source tools and licenses. For work internal to i2b2, modifications will follow the terms of the Brigham and Women’s Hospital Inc. i2b2 Open Source Software License. While not open source, we also anticipate that our partnership with Velos regarding the eIRB module will prove beneficial to other CTSA and research organizations using Velos. E. INTERACTION AND INTEGRATION OF INFORMATICS WITH THE OTHER HICTR COMPONENTS. Clinical & Translational Research Education Center (CTREC) Participant & Clinical Interaction Resources Program (PCIRP) Community Partnership for Health Program (CPH) Novel Methods 1: Institute for Advancing Medical Innovations (NM:IAMI) Novel Methods 2: Personalized Medicine and Outcomes Center Pilot and Collaborative Studies Funding Program Translational Technologies Resource Center (TTRC) Biostatistics Regulatory Knowledge and Support In aim C.1, the portal will promote access to educational offerings. Dr. Lushington coordinates educational offering from CBI and the School of Engineering which may be relevant for certain translational investigators. Dr. Warren will coordinate educational offerings (ex: AMIA 10x10) from the Center for Health Informatics and provide guidance regarding educational simulations. CRIS and HERON support for PCIRP research (e.g, study form development using standardized terminology, potential study cohort size and hypotheses generation). PCIRP provides oversight for HICTR Participant Registry via the Data Request Committee. We will work with CPH leadership and KUMC Outreach to develop and evaluate methods for T2 translation of research into practice in partnership with the rural KPEPR network in aim C.4. Bioinformatics provides extensive informatics consultation for IAMIsupported high throughput screening and lead optimization projects (8 distinct projects within the past year alone). We specifically extend bioinformatics expertise to integrate pharmacokinetics and clinical trials in aim C.3. In aim C.1, we will advance the adoption of web-based tools for collaborative research and on-line communities such as CRIS/Velos and www.cvoutcomes.org. In aim C.4, we will collaborate with Dr. Spertus on applying PRISM to other workflows. In aim C.4 we will collaborate with Drs. Shireman and N. Dunton regarding Medicaid and nursing quality databases respectively. Research funded by pilot programs will use informatics resources. In aim C.1, the portal will be used to track Pilot program requests. Many of the TTRC resources are informatics technologies. This is facilitated by the fact that the informatics co-director, Dr. Lushington, also directs the TTRC Molecular Biomarker Core. In aim C.3, informatics will work with the Biological Tissue Repository to link specimens to the clinical information and improve specimen management and with the Pharmacokinetic/Pharmacodynamics (PK/PD) program to integrate findings with the Comprehensive Research Information System and information from the clinical record for phase I clinical trials. Biostatistics and Informatics work closely regarding maintenance and expansion of data-related resources and data warehouses for the HICTR; compliance with national standards and innovation in developing interfaces between biostatistics and informatics will be ongoing. The CRIS team is led by the Biomedical Informatics director who is a faculty member in the Department of Biostatistics. The portal enhances research users’ access to regulatory materials and processes. Informatics is directing the electronic IRB to improve 18 Barohn, Richard J. Program Ethics Program regulatory oversight and ease access for investigators. Regulatory support uses informatics methods to track initial project requests, research monitoring, and clinical research coordinator services. The Ethics program will be engaged in oversight regarding ethical and privacy concerns in the development of databases especially HERON (Aim 2). Our recent capability to provide electronic IRB processes and use HERON to determine if we have the patient population to carry out studies will inform the ethical oversight of research protocols. F. EVALUATION, IMPLEMENTATION AND MILESTONES The evaluation plan and identification of specific milestones for the Biomedical Informatics key function are in the Evaluation Section (Section 14) and the Implementation and Milestones Section (Section 15) of this application. Figure 3.5 shown below also provides an overview of our specific aims in relation to the in-kind current and projected staffing and additional personnel requested. Where specific aims are aligned with other institutional objectives for informatics and the biomedical informatics team, they will be provided in-kind. 19 Barohn, Richard J. Key Personnel: RW Russ Waitman; GL Gerry Lushington; JW Judy Warren; AC Arvinder Choudhary; DC Dan Connolly; MV Mahesh Visvanathan Teams: kbc K-INBRE Bioinformatics Core; bmi Biomedical Informatics, telemed Kansas University Center for Telemedicine and Telehealth Note: Bar height indicates relative effort Combined Teams Full Time Equivalents (FTE) for Clinical and Translational Research 5.5 3.7 Existing CRIS Initiatives and Services Research Budgeting 0.8 FTE (bmi) eIRB rollout 1.2 FTE (bmi) 9.5 9 8.3 7.5 post CTSA funding Research Budgeting maintain and refine 0.2 FTE (bmi) eIRB adv. process mgt. 1.0 FTE (bmi) eIRB maintain and refine 0.3 FTE (bmi) CRIS & demographics and lab integration 1 FTE (DC, bmi) CRIS improved integration maintain and refine 0.3 FTE (bmi) C4.6 ePRISM -> EPIC integration 1 FTE (RW, JW, bmi) C.4.5 HERON<-> Medicaid/Medicare dataset integration 0.6 FTE (AC, RW, bmi) Aim 4 C.4.3 wire EPIC & systems for T2 research with HERON 1 FTE (JW, RW, DC, bmi) C.4.1 HIE planning (HC, RW) Community EMR adoption & HIE established Maintain 0.2 FTE (bmi) Maintain intervention monitoring 0.3 FTE (bmi) C.4.4 Community EHRs and HIE as platform for research 1.7 FTE (JW, RW, bmi) C4.2 CRIS and Telemedicine in kind/fee for service (RS, bmi, telemed) C3.3 BI, CRIS,HERON integration 0.7 FTE (GL, MV, RW, kbc, bmi) C3.2 PK/PD and CRIS 0.7 FTE (GL, MV, RW, kbc, bmi) C3.1 Clinical Pathology and HERON 1 FTE (bmi, RW) Aim 3 C3.1 Biological Tissue Repository and CRIS or caTissue 1 FTE (bmi, RW) Maintain (bmi) 0.1 FTE Maintain, refine Clinical Pathology integration 0.2 FTE (bmi) Biological Tissue Repository integration maintain, refine 0.3 FTE (bmi) Bioinformatics in kind/fee for service (GL coord 0.05 FTE, kbc) CRIS/caBIG, start ontology HERON: ontology mgt enhanced 0.7 FTE (JW, bmi) HERON: ontology mgt maintain 0.5 FTE (JW, GL, bmi) Aim 2 HERON Construct 2.5 FTE (AC, DC, RW, bmi) Consults (RW) HERON: maintain + ETL/messaging + feeds 3 FTE (AC, DC, RW, bmi) HERON: maintain, refine, add feeds 2.5 FTE (AC, DC, RW, bmi) Staffed Informatics Consult Service Established 0.7 FTE (JW, bmi) Informatics Consult Service Team Based 0.7 FTE (RW, JW, bmi) Aim 1 Portal: foundation 0.5 FTE (DC, RW, bmi) 2011 Portal: HICTR focused 0.6 FTE (DC, RW, bmi) Bioinformatics Resources 0.05 FTE (GL) 2012 2013 Portal maintain, refine 0.5 FTE (bmi, DC, kbc) 2014 2015 Jul 2010 2016 Jul 2016 Figure 3.5. Biomedical Informatics Aims and Team Resources Timeline G. REFERENCES 1. Pulley JM, Harris PA, Yarbrough T, Swafford J, Edwards T, Bernard GR. Acad Med. 2010 Jan;85(1):164-8. An informatics-based tool to assist researchers in initiating research at an academic medical center: Vanderbilt Customized Action Plan. 20 Barohn, Richard J. 2. Parks M, Anderson W. E-Project: A Web-based System to Enhance the Pure Matrix of Project Management for Biostatistical Informatics. The Society for Clinical Trials 31st Annual Meeting, Baltimore Maryland, May 17, 2010. 3. Kriete, A and Eils, R. Systems Biology. Academic Press, Burlington MA, 2006. 4. Sears CS, Prescott VM, McDonald CJ. The Indiana Network for Patient Care: A Case Study of a Successful Healthcare Data Sharing Agreement. American Bar Association Health eSource, September 2005. 5. Weber GM, Murphy SN, McMurry AJ, Macfadden D, Nigrin DJ, Churchill S, Kohane IS. The Shared Health Research Information Network (SHRINE): a prototype federated query tool for clinical data repositories. J Am Med Inform Assoc. 2009 Sep-Oct;16(5):624-30. 6. Roden DM, Pulley JM, Basford MA, Bernard GR, Clayton EW, Balser JR, Masys DR. Development of a large-scale de-identified DNA biobank to enable personalized medicine. Clin Pharmacol Ther. 2008 Sep;84(3):362-9. Epub 2008 May 21. 7. Pulley J, Clayton E, Bernard GR, Roden DM, Masys DR. Principles of human subjects protections applied in an opt-out, de-identified biobank. Clin Transl Sci. 2010 Feb;3(1):42-8. 8. Murphy SN, Weber G, Mendis M, Gainer V, Chueh HC, Churchill S, Kohane I. Serving the enterprise and beyond with informatics for integrating biology and the bedside (i2b2). J Am Med Inform Assoc. 2010 MarApr;17(2):124-30. 9. Friedlin FJ, McDonald CJ. A software tool for removing patient identifying information from clinical documents. J Am Med Inform Assoc. 2008 Sep-Oct;15(5):601-10. Epub 2008 Jun 25. 10. Loukides G, Denny JC, Malin B. The disclosure of diagnosis codes can breach research participants' privacy. J Am Med Inform Assoc. 2010 May 1;17(3):322-7. 11. Benitez K, Malin B. Evaluating re-identification risks with respect to the HIPAA privacy rule. J Am Med Inform Assoc. 2010 Mar 1;17(2):169-77. 12. Karp DR, Carlin S, Cook-Deegan R, Ford DE, Geller G, Glass DN, Greely H, Guthridge J, Kahn J, Kaslow R, Kraft C, Macqueen K, Malin B, Scheuerman RH, Sugarman J. Ethical and practical issues associated with aggregating databases. PLoS Med. 2008 Sep 23;5(9):e190. 13. Yeniterzi R, Aberdeen J, Bayer S, Wellner B, Hirschman L, Malin B. Effects of personal identifier resynthesis on clinical text de-identification. J Am Med Inform Assoc. 2010 Mar 1;17(2):159-68. 14. SP 800-66 Rev 1 Oct 2008 An Introductory Resource Guide for Implementing the Health Insurance Portability and Accountability Act (HIPAA) Security Rule http://csrc.nist.gov/publications/nistpubs/800-66Rev1/SP-800-66-Revision1.pdf 15. Wynden R, Weiner MG, Sim I, Gabriel D, Casale M, Carini S, Hastings S, Ervin D, Tu S, Gennari J, Anderson N, Mobed K, Lakshminarayanan P, Massary M, Cucina R. Ontology mapping and data discovery for the translational investigator. Presented at the 2010 AMIA Summit on Clinical Research Informatics meeting, March 12-13 2010, San Francisco, CA. 16. Blumenthal D, Tavenner M. The "Meaningful Use" Regulation for Electronic Health Records. N Engl J Med. 2010 Jul 13. 17. Diamond CC, Mostashari F, Shirky C. Collecting and sharing data for population health: a new paradigm. Health Aff (Millwood). 2009 Mar-Apr;28(2):454-66. 18. Berman JJ. Zero-check: a zero-knowledge protocol for reconciling patient identities across institutions. Arch Pathol Lab Med. 2004 Mar;128(3):344-6. 19. Nass SJ, Moses HL, Mendelsohn. A National Cancer Clinical Trials System for the 21st Century: Reinvigorating the NCI Cooperative Group Program. Committee on Cancer Clinical Trials and the NCI Cooperative Group Program; Institute of Medicine. Washington, DC: National Academies Press, 2010. 20. Zhou, Z., Lee, I.-H., Lushington, G.H., Visvanathan, M. ISMB 2010, submitted. 21. Parkinson M. Executive Order 10-06 Kansas Health Information Exchange, Inc. Governor of the State of Kansas. http://governor.ks.gov/issues-a-initiatives/executive-orders/717-executive-order-10-06 22. Spaulding RJ, Russo T, Cook DJ, Doolittle GC. Diffusion theory and telemedicine adoption by Kansas health-care providers: critical factors in telemedicine adoption for improved patient access. J Telemed Telecare. 2005;11 Suppl 1:107-9. 23. Doolittle GC, Spaulding RJ. Defining the needs of a telemedicine service. J Telemed Telecare. 2006;12(6):276-84. 23. Cox LS, Cupertino AP, Mussulman LM, Nazir N, Greiner KA, Mahnken JD, Ahluwalia JS, Ellerbeck EF. Design and baseline characteristics from the KAN-QUIT disease management intervention for rural smokers in primary care. Prev Med. 2008 Aug;47(2):200-5. 21