Group B: IRRITABLE BOWEL SYDROME in a 40
advertisement
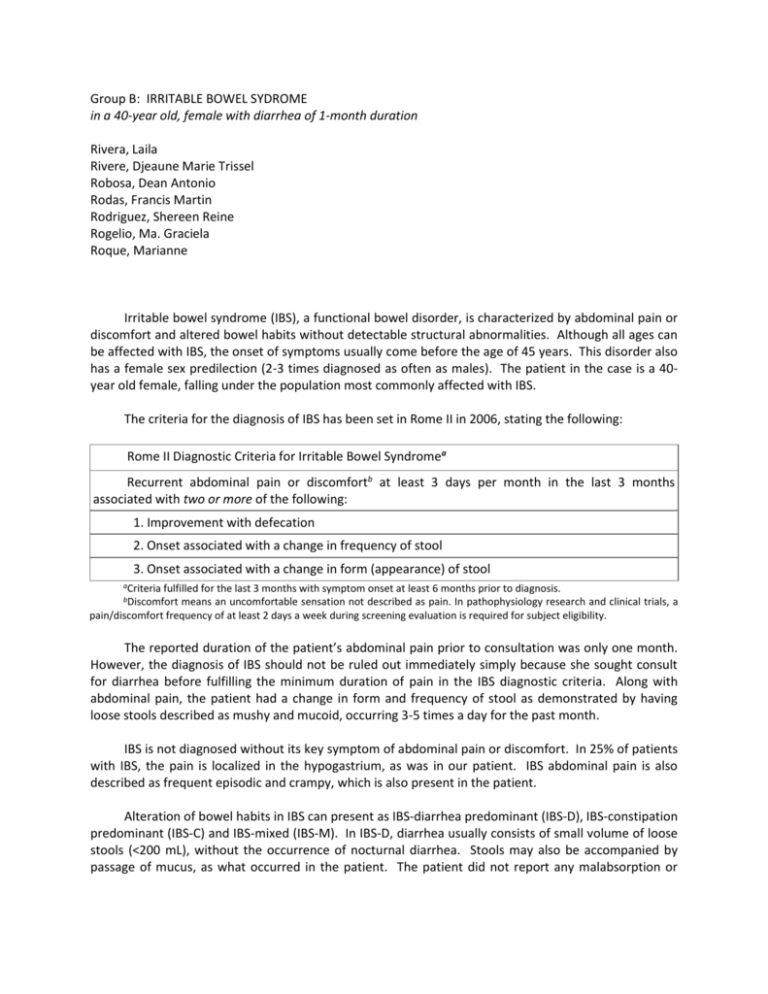
Group B: IRRITABLE BOWEL SYDROME in a 40-year old, female with diarrhea of 1-month duration Rivera, Laila Rivere, Djeaune Marie Trissel Robosa, Dean Antonio Rodas, Francis Martin Rodriguez, Shereen Reine Rogelio, Ma. Graciela Roque, Marianne Irritable bowel syndrome (IBS), a functional bowel disorder, is characterized by abdominal pain or discomfort and altered bowel habits without detectable structural abnormalities. Although all ages can be affected with IBS, the onset of symptoms usually come before the age of 45 years. This disorder also has a female sex predilection (2-3 times diagnosed as often as males). The patient in the case is a 40year old female, falling under the population most commonly affected with IBS. The criteria for the diagnosis of IBS has been set in Rome II in 2006, stating the following: Rome II Diagnostic Criteria for Irritable Bowel Syndromea Recurrent abdominal pain or discomfortb at least 3 days per month in the last 3 months associated with two or more of the following: 1. Improvement with defecation 2. Onset associated with a change in frequency of stool 3. Onset associated with a change in form (appearance) of stool aCriteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis. means an uncomfortable sensation not described as pain. In pathophysiology research and clinical trials, a pain/discomfort frequency of at least 2 days a week during screening evaluation is required for subject eligibility. bDiscomfort The reported duration of the patient’s abdominal pain prior to consultation was only one month. However, the diagnosis of IBS should not be ruled out immediately simply because she sought consult for diarrhea before fulfilling the minimum duration of pain in the IBS diagnostic criteria. Along with abdominal pain, the patient had a change in form and frequency of stool as demonstrated by having loose stools described as mushy and mucoid, occurring 3-5 times a day for the past month. IBS is not diagnosed without its key symptom of abdominal pain or discomfort. In 25% of patients with IBS, the pain is localized in the hypogastrium, as was in our patient. IBS abdominal pain is also described as frequent episodic and crampy, which is also present in the patient. Alteration of bowel habits in IBS can present as IBS-diarrhea predominant (IBS-D), IBS-constipation predominant (IBS-C) and IBS-mixed (IBS-M). In IBS-D, diarrhea usually consists of small volume of loose stools (<200 mL), without the occurrence of nocturnal diarrhea. Stools may also be accompanied by passage of mucus, as what occurred in the patient. The patient did not report any malabsorption or weight loss, which is not associated with IBS. Bleeding (also not a feature of IBS) occurred, but the presence of hemorrhoids, cannot be ruled out. The pathophysiology of IBS-diarrhea predominant in the patient may be explained by small bowel dysmotility manifesting as accelerated meal transit in patients prone to diarrhea. Patients exhibit shorter intervals between migratory motor complexes which is the predominant interdigestive small bowel motor patterns. Colonic motor abnormalities are more prominent under stimulated conditions such as eating. IBS patients exhibit increased recto-sigmoid activity for up to 3 hours after eating. The patient’s associated crampy hypogastric pain may be due to visceral hyperalgesia – the enhanced perception of normal motility and visceral pain characteristic of irritable bowel syndrome. Patients who are affected describe widened dermatomal distributions of referred pain. Sensitization of the intestinal afferent nociceptive pathways that synapse in the dorsal horn of the spinal cord provides a unifying mechanism. Visceral afferent dysfunction manifests as exaggerated sensory responses to visceral stimulation which influences postprandial pain in 74% of IBS patients after the entry of food bolus to the cecum. The IBS-diarrhea predominant symptom in the patient may have also been due to a GI infection she could have acquired during her 1 year stay in Bangladesh. Small bowel bacterial overgrowth has been heralded as a unifying mechanism for the symptoms of bloating and distention common to patients with IBS. The microbes involved are Campylobacter, Salmonella and Shigella. Those patients with Campylobacter infections who are toxin-positive are more likely to develop postinfective IBS. Increased rectal mucosal enteroendocrine cells, T lymphocytes and increased gut permeability could persist and may contribute to postinfective IBS. The diagnosis of IBS relies on recognition of positive clinical features (Rome II diagnostic criteria plus other supportive symptoms such as defecation straining, urgency or a feeling of incomplete bowel movement, passing mucus, bloating, lethargy, nausea, backache and bladder symptoms) and elimination of other organic diseases. The differential diagnosis of IBS should be based on the location of the pain, accompanying symptoms, and the primary associated bowel habit. All patients presenting with possible IBS symptoms should be asked if they have unintentional and unexplained weight loss, rectal bleeding, family history of bowel or ovarian cancer, change in bowel habit to looser and/or more frequent stools persisting for more than 6 weeks in a person aged over 60 years and should be referred to secondary care for further investigation if any are present. In people who meet the IBS diagnostic criteria, the following tests should be undertaken to exclude other diagnoses: complete blood count (CBC), erythrocyte sedimentation rate (ESR) or plasma viscosity, C-reactive protein (CRP), antibody testing for coeliac disease (endomysial antibodies [EMA] or tissue transglutaminase [TTG]) (National Institute for Health and Clinical Excellence, 2008), sigmoidoscopic examination, stool examination for ova and parasites. The laboratory features that argue against IBS include evidence of anemia, elevated ESR, presence of leukocytes or blood in stool, and stool volume > 200-30 mL/d (Fauci 2007). The patient in our case presents with diarrhea and is classified as IBS-D. Antidiarrheal agents used for IBS-D patients include peripherally acting opiate-based agents, loperamide and bile acid binder cholestyramine resin. Peripherally acting opiate-based agents is the initial therapy of choice for IBS-D. Some drugs showed potential for management of IBS and are currently being studied, an example is TCA imipramine and serotonin receptor agonist and antagonists. Tricyclic antidepressant (imipramine) slows jejunal migrating motor complex transit propagation and delays orocecal and whole-gut transit, indicative of a motor inhibitory effect making it a possible drug for IBS-D. There are other drugs that could be recommended for the treatment of IBS, such as antispasmodics and antiflatulence therapy. Antiflatulence therapy includes advising the patient to eat slow and to not chew gum or drink carbonated beverages; dietary exclusion trial; avoiding flatogenic foods, exercising, losing weight, taking activated charcoal; probiotics which is still in trials. In the management of IBS, patient counseling and dietary alterations are important. The patient must be reassured and the functional nature of the disorder must be carefully explained. Food precipitants that aggravate the symptoms should be avoided and foodstuff that appears to produce the symptoms eliminated from the patient’s diet. Dietary change would include a high fiber diet. References: De Gowin’s et.al. Diagnostic examination 2004. 8th edition. McGraw-Hill, USA Fauci et.al. Harrison’s principles of Internal Medicine 2008 17th edition. McGraw-Hill USA Lehrer J. Irritable Bowel Syndrome. http://emedicine. medscape. com/article/ 180389-overview; Aug 2009 [Full Text] [No authors listed].(2008). Irritable bowel syndrome in adults: Diagnosis and management of irritable bowel syndrome in primary care by The National Institute for Health and Clinical Excellence