Resource
advertisement

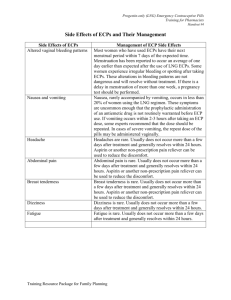
ECP Referral Guide After completing a primary and secondary survey, contact the ECP. This chart is a guide only. Extended care paramedics (ECPs) can provide treatment to patients at home or in a residential-care setting and thus help avoid unnecessary trips to hospital. However, it’s important that they are called to the right cases. Certain patient conditions and situations mean an ECP may not be appropriate (see ECP precautions/exclusions). If unsure in regards to ECP precautions/exclusions, please discuss with the ECP. Wound Care ECPs can attend: lacerations skin tears abrasions bites minor wounds existing wounds. ECP precautions/exclusions: injuries to face, genital area, hands or feet or over joints deep tissue wounds injuries requiring extensive closure loss of function penetrating injuries distal skin flaps foreign bodies paediatrics pt on anticoagulants and has head injury. Support ECPs can provide: crew consultation (career and volunteer) CPG extension paramedics (if no ICP available) client call-back and alternate pathways referral to respite services for carers. Palliative care ECPs can attend: generalised deterioration breakthrough pain respiratory distress vomiting agitation and delirium medication delivery – systems issues, e.g. pumps ECP precautions: pt without advance – directive document. Allergies ECPs can attend: mild to moderate allergic reactions pts with no Hx of deterioration cases not requiring adrenaline ECPs exclusions: anaphylaxis significant comorbidity (e.g. immunecompromised pt) airway or mucosal angioedema. Continence and feeding devices ECPs can attend for insertion of or issues with indwelling catheter (IDC) supra-pubic catheter (SPC) feeding tube (PEG). Note: ECPs only attend if regular continence provider is not available. ECP precautions/exclusions: first-time catheters acute urinary retention bleeding around catheter, recent TURP or haematuria traction pull PEGs (discuss on consult). Gastrointestinal/Genital ECPs can attend: diarrhoea and/or vomiting dehydration/heatwave rectal prolapse paraphimosis. ECP precautions/exclusions: decreased urine output over extended time malaena or haematemesis Hx of bowel obstruction (abdo. distention or tenderness) haemodynamic compromise or altered GCS significant comorbidity that may benefit from hospital assessment. Infections ECPs can attend: UTI (pt not pregnant and no anuria) cellulitis respiratory (if no previous ICU/HDU admissions and not needing increased O2). ECP precautions/exclusions: first presentation of male UTI suspected pyelonephritis immunocompromised pt or risk of infection febrile neutropenia (chemo) suspected sepsis pt currently taking steroids comorbidity, i.e. CCF or COAD. Musculoskeletal pain ECPs can attend: back pain chronic pain ring removal. ECP exclusions: acute loss of neurovascular integrity acute pain (if secondary to trauma) undiagnosed abdo, or chest pain. Headaches ECPs can attend: simple headaches migraine with previous Hx and identical presentation. ECPs exclusions: new presentation of severe headache suspicion of CVA/positive ROSIER pregnant pt Hx of recent head trauma suspected infection, e.g. Meningococcal, septicaemia loss of consciousness lack of responsible person for supervision decreased GCS. Dizziness ECPs can attend: vertigo/Hx of Meniere’s dizziness not central in origin with known Hx of benign causes. ECP precautions/exclusions: cardiac Hx CVA/other neurological pathology ECP Referral Guide consider metabolic, sepsis or other nonbenign causes. After completing a primary and secondary survey, contact the ECP. This chart is a guide only.








![view Unit 14: Emergency Contraceptive Pills [PDF 319KB]](http://s3.studylib.net/store/data/008439478_1-6df94ca90794562e31dfc68f6a601d55-300x300.png)