Case Studies Aging Course
advertisement

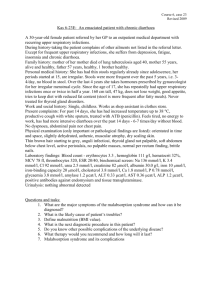
Case Studies Aging Course Case 1 A 68 year old woman with metastatic colon cancer presents to the ER with 1 hour of chest pain and shortness of breath. She has no known previous cardiac or pulmonary problems. ABG: pH 7.49 , pCO2 28 torr, HCO3- 21 mmol/l, pO2 52 torr Lab. Tests: Na+ 133 mmol/l, K+ 3.9 mmol/l, Cl- 102 mmol/l, HCO3- 22 mmol/l Questions: 1. What is the predominant acid-base disorder? 2. Is the degree of compensation appropriate? 3. Interpret the blood gases. 4. Is there another disorder present? Case 2 A 75 year old man with morbid obesity is sent to the ER by his skilled nursing facility after he developed a fever of 38 oC and rigors 2 hours ago. In the ER he is lucid and states that he feels „terrible“, but offers no localizing symptoms. His ER vitals include a heart rate of 115´, and a blood pressure of 84/46 torr. ABG: pH 7.12 , pCO2 50 torr, HCO3- 13 mmol/l, pO2 96 torr Lab. tests: Na+ 138 mmol/l, K+ 4.2 mmol/l, Cl- 99 mmol/l, HCO3- 15 mmol/l Urine pH 5.0 Questions: 1. What is the „predominat“ acid-base disorder? 2. Is the degree of compensation appropriate? 3. Interpret the blood gases. 4. How would you classify this patient´s haemodynamic status? 5. Is there another disorder present? Case 3 A 62 year old woman with severe COPD comes to the ER complaining of increased cough and shortness of breath for the past 12 hours. There are no baseline ABGs to compare to, however, her HCO3- measured during a routine clinic visit 3 month ago was 34 mmol/l. ABG: pH 7.21 , pCO2 85 torr, HCO3- 33 mmol/l, pO2 47 torr Lab. tests: Na+ 135 mmol/l, K+ 4.0 mmol/l, Cl- 90 mmol/l, HCO3- 34 mmol/l Urine pH 5.5 Questions: 1. What is the „predominant“ acid-base disorder? 2. Is the degree of compensation appropriate? 3. Interpret the blood gases. 4. Is there another disorder present? Case 4 Mr. Homans is a 74 year old man with a past history significant for hypertension and COPD from smoking 2 packs per day for the last 40 years. He presented to an urgent pulmonary clinic appointment with 2 months of increased cough and 5 days of “mild” hemoptysis. Upon further obtaining further history, he reports feeling fatigued, nauseous, and chronically thirsty for several weeks. His exam is significant for bilateral rhonchi (no change from baseline lung exam) and absent reflexes. Stat labs are ordered from clinic: Sodium – 138 mmol/l, potassium – 3.7 mmol/l, magnesium – 0.9 mmol/l, calcium (total) – 3.2 mmol/l, phosphate – 0.42 mmol/l, albumin – 22 g/l, creatinine – 248 umol/l, Hct, PT/PTT, platelets – all normal, PTH - Pending Questions: 1. What primary physiologic abnormalities are present? 2. What is your explanation for his fatigue and chronic thirst? 3. Are any additional tests indicated, and if so, which ones? 4. What type of process is going on in the chest by evidence of exam? Case 5 A 79 year old diabetic male is brought to the ER for evaluation of shortness of breath. His symptoms began gradually after he returned from a trip yesterday evening (approximately 8 hours ago). At that time, he felt unusually fatigued, and thought he had 'overdone' it by walking 2 blocks to the market and back, an activity he did regularly. Thinking his symptoms were due to the flu, he took an aspirin upon arriving home, but without relief. He remained awake all night, and starting about 2 1/2 hours ago, he became progressively more dyspneic and air-hungry. He denies fever, chills, cough, hemoptysis, chest pain, lower extremity edema, or remote history of either cardiac or pulmonary disease. He checks his blood sugars regularly, and they have been well-controlled recently. Past medical history is notable for hypertension, well-controlled Type 2 diabetes mellitus with insulin, and osteoarthritis. Habits include a 50 pack-year history of tobacco use, but no current tobacco or alcohol. Examination: well-developed, well-nourished man appearing fatigued but in no acute distress. BP 150/90 torr, HR 104´ RR 24´ T 37.5 oC, generalized pallor, no obstruction in upper airway no skeletal deformities of chest, no use of accessory muscles of respiration, no intercostal retractions. Auscultation clear without wheezing, rales or rhonchi; heart: regular rhythm, no S3 or S4, grade 2/6 systolic murmur at left lower sternal border without radiation; jugular venous pressure 6cm; normal bowel tones, without masses or organomegaly; limbs symmetric, no edema. Bedside data: O2 saturation 93% on room air; Quick-look rhythm check reveals sinus rhythm, rate 105´. 12-lead EKG is pending. Questions: 1. What is your working diagnosis for this patient's complaints and physical findings? 2. Do either the subjective or objective findings provide a clear indication of the diagnosis? 3. How would you classify this patient´s haemodynamic status? 4. What underlying processes are involved in this disease? 5. What regulatory mechanisms are involved in this disease? 6. What might explain the elevated blood pressure other than essential hypertension? 7. What would be your next step in this situation? Case 6 An 84 woman presents to the emergency department after her falling at home. She has been having several days of high fever, nausea and poor intake of food or fluid. On exam she is weak appearing, slightly disoriented and dizzy. Her HR is 96´and her BP is 120/50 torr in the supine position, and HR 132´and BP 92/46 torr when upright. Her mucous membranes are dry and her neck veins are not seen while lying at a 30o angle. Her heart is tachycardic, her lungs are clear and her abdomen is soft and non-tender. Extremities reveal poor skin turgor and weak distal pulses. Laboratory data: Na+ 132 mmol/l in ER 139 mmol/l 1 week prior K+ 4,9 mmol/l 4,3 mmol/l Cl- 92 mmol/l HCO3- 32 mmol/l BUN 22,8 mmol/l Creatinine 168 umol/l 102 mmol/l 24 mmol/l 4,3 mmol/l 70,7 umol/l Questions: 1. How can you explain the laboratory findings? 2. What has caused her fall? 3. Why isn’t he sweating? 4. Why did she become disoriented? 5. Would you expect her urinary volume to decrease or increase? 6. Why was her blood pressure so different in supine and lying position? 7. Was her pulse rate decreased or increased and why? Case 7 Dr. Ramon. is a 64 year-old surgeon. He awakens one morning and feels entirely well. While eating breakfast, he notes precipitous development of left-sided weakness. His speech becomes slurred, and he drops his fork. He feels dizzy and sees double. This persists for ten minutes and all symptoms rapidly and completely resolve. He does not seek medical care as he believes the symptoms are due to “low blood sugar” before breakfast as they resolve with food intake. He proceeds to his office to carry out his schedule for the day. He is fine until 30 minutes before his lunch break, when he suddenly develops a severe occipital headache and becomes dizzy with diplopia. He collapses and cannot move his left side and cannot speak. Past Medical History: He has controlled hypertension. He has had a prior myocardial infarction and still has occasional angina. He has intermittent claudication of legs and has been diagnosed with peripheral arterial vascular disease, but refuses vascular or cardiac surgery. He is obese, smokes one pack of cigarettes per day and has elevated blood cholesterol levels. He has no history of diabetes mellitus. Physical examination: BP 190/104 mm Hg (right arm, sitting), P 80 regular, R 12, regular, Neck – supple, no neck vein distension, Heart & Lungs – normal, Pulse – symmetrical, no bruits, Neurological examination: Awake, eyes open but does not follow examiner commands, cannot verbalize – phonate, Cannot stand due to severe weakness, Quadriplegic with no motor response, motor tone reduced in all extremities, areflexic with extensor Babinski responses bilaterally, no withdrawal response to pin prick, pupils equal and respond to light; no horizontal eye movements with preserved vertical eye movements, bilateral facial weakness with preserved blink response; gag and palate movements preserved; aphonic Laboratory studies: CBC – normal, urinalysis – normal, chest x-ray – enlarged heart, EKG – old anterior wall myocardial infarction Imaging investigations - angiography - high grade midbasilar stenosis Questions: 1. What can explain the difficulty in seeing and his problems with fine movements in the morning? 2. What's causing the progressive extremity weakness? 3. Explain the sensory difficulties. 4. What is the reason for changes in reflex responses? 5. What is the reason for facial weakness? 6. Explain the positive Babinski sign. 7. What does the past medical history indicate? 8. What level is the lesion? 9. What structures are damaged that result in these symptoms? Case 8 An 81- year- old Mr. Ryan is brought to the physician's office by his son who . The son is concerned that father is increasingly forgetful. Recently, he became lost on a walk in his neighborhood. Mr. Ryan denies depressed mood, difficulty sleeping, concerns about death, or thoughts about taking his life. On further questioning, Mr. Ryan's son describes that over the last two years his father has had increasing difficulty managing his finances, caring for his apartment, and preparing meals. He has trouble remembering the names of his three grandchildren and has forgotten all family birthdays over the past year. He will spend most of the morning reading the paper and seems to reread the sports pages several times. Past medical history is unremarkable except for bilateral cataract replacements. There are no prescribed medications. There is no history of depression. He remotes smoking history but no cigarettes for over thirty years, and one to two drinks a night. Physical exam: pleasant older man, laughing and winking as his son mentions his concerns. Vital signs - regular pulse at 70´ and a blood pressure of 145/90 torr. No evidence of head trauma, clear lungs, a regular cardiac rhythm with a soft systolic murmur heard at the right second intercostal space, no carotid bruits, a benign abdominal and a firm prostate nodule. Neurologic exam reveals normal cranial nerve findings, normal motor strength in all extremities, sensory intact to light touch with decreased vibratory sense in legs, and normal cerebellar exam, gait, and reflexes. A Mini-Mental State Exam reveals a lower total score than normal. Mr. Ryan missed the day, date, year, and place. He was attentive and able to spell WORLD backwards. He remembered 0 from 3 objects after 5 minutes. Questions: 1. What is your working diagnosis for Mr. Ryan and why? 2. What parts of the history, physical, and mental status examinations aid you in your final diagnosis? 3. What tests would you order for Mr. Ryan's work-up? 4. What can explain the difficulty in expressing herself and her problems with concentration and short-term memory? 5. What's causing the progressive difficulty managing with normal life activities? 6. Explain the change of blood pressure level. 7. What is the reason for vibration and proprioceptive loss in both lower extremities? 8. What would you discuss with Mr. Ryan and his family about diagnosis and planning for the future?