appendix - JACC: Cardiovascular Imaging
advertisement
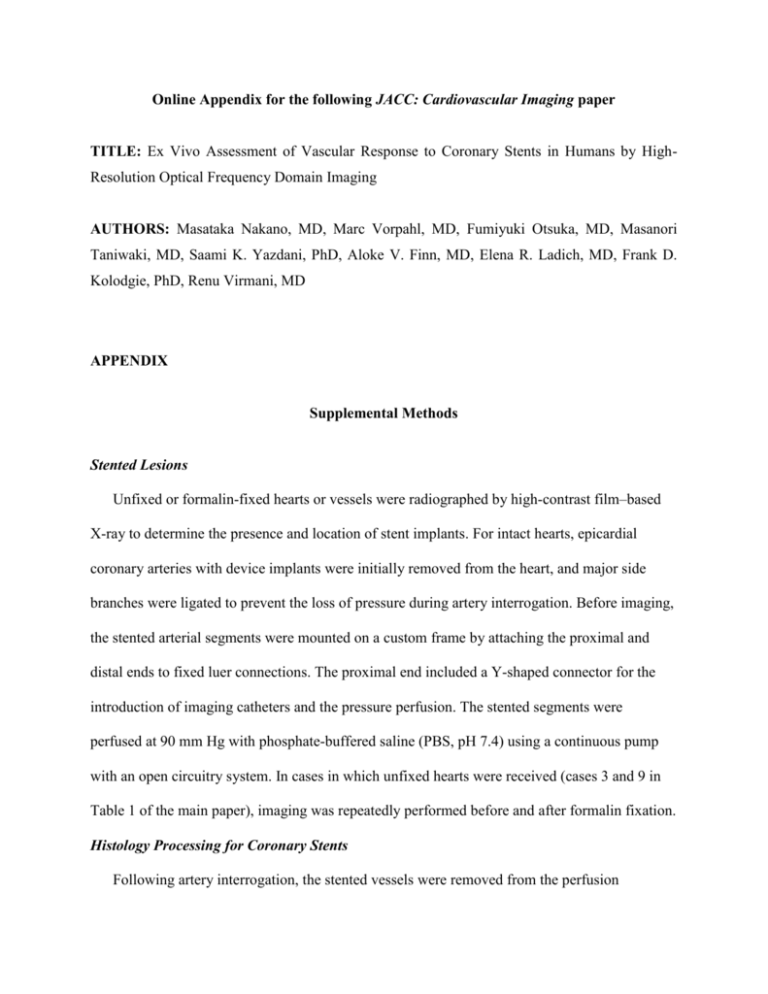
Online Appendix for the following JACC: Cardiovascular Imaging paper TITLE: Ex Vivo Assessment of Vascular Response to Coronary Stents in Humans by HighResolution Optical Frequency Domain Imaging AUTHORS: Masataka Nakano, MD, Marc Vorpahl, MD, Fumiyuki Otsuka, MD, Masanori Taniwaki, MD, Saami K. Yazdani, PhD, Aloke V. Finn, MD, Elena R. Ladich, MD, Frank D. Kolodgie, PhD, Renu Virmani, MD APPENDIX Supplemental Methods Stented Lesions Unfixed or formalin-fixed hearts or vessels were radiographed by high-contrast film–based X-ray to determine the presence and location of stent implants. For intact hearts, epicardial coronary arteries with device implants were initially removed from the heart, and major side branches were ligated to prevent the loss of pressure during artery interrogation. Before imaging, the stented arterial segments were mounted on a custom frame by attaching the proximal and distal ends to fixed luer connections. The proximal end included a Y-shaped connector for the introduction of imaging catheters and the pressure perfusion. The stented segments were perfused at 90 mm Hg with phosphate-buffered saline (PBS, pH 7.4) using a continuous pump with an open circuitry system. In cases in which unfixed hearts were received (cases 3 and 9 in Table 1 of the main paper), imaging was repeatedly performed before and after formalin fixation. Histology Processing for Coronary Stents Following artery interrogation, the stented vessels were removed from the perfusion apparatus, dehydrated in a graded series of ethanol, and embedded in methylmethacrylate resin. After polymerization, the stented artery was segmented at 2-mm intervals using a diamond wafering blade. Histological sections were then prepared on a rotary microtome equipped with a tungsten carbide knife, at four to six microns, mounted and stained with hematoxylin and eosin (H&E) and modified Movat pentachrome (1). The confirmation of hypersensitivity was based on recognition of eosinophils by Luna stain (2). Difference of OFDI Signal from Unfixed and Formalin-fixed Tissue In the limited cases (case numbers 3 and 9 in Table 1 of the main paper), optical frequency domain imaging was performed before and after formalin fixation. Histological slides from those cases including i) normal neointima >1 year (n = 6 sections) and ii) organized thrombus (n = 5) were co-registered with corresponding OFDI images obtained in the unfixed and fixed status. The OFDI signal intensity was calculated from luminal surface to 0.3-0.4 mm depth, and fitted to an approximate exponential formula (y = A×exp−Bx), where index A represents a “Peak intensity,” and index B reflects an “Attenuation rate” as described in the main paper. For all sections, 3 regions of interest (ROI) were selected for each feature were examined and averaged. Prior to this evaluation, all OFDI images were adjusted to the same default setting, and the analysis was performed by Image J software (National Institutes of Health, Rockville, MD). Statistical Analysis The values were expressed as mean SD for continuous valuables. Paired t-test was used to calculate the significance of differences between OFDI signals from unfixed and formalin-fixed tissues. A value of p < 0.05 was considered statistically significant. 2 3 Supplemental Results/Discussion Results of OFDI signal analysis of the differences between unfixed and formalin-fixed tissue are summarized in Online Table 1 and Online Figure 6. There were no en face differences in OFDI appearance of unfixed and fixed tissues. Similarly, quantitative evaluation of OFDI signals did not show absolute disparities, where signal Peak intensity of normal neointima >1 year in unfixed and fixed tissues were 180.9 ± 5.0 and 182.1 ± 4.4, respectively (p = 0.33), and Peak intensity of organized thrombus were 136.1 ± 3.8 (unfixed) vs. 135.4 ± 3.8 (fixed) (p = 0.62). In addition, no difference was identified in the analysis of Attenuation rate: normal neointima >1 year, 0.37 ± 0.17 (unfixed) vs. 0.37 ± 0.13 (fixed) (p = 0.92); organized thrombus, 0.40 ± 0.06 (unfixed) vs. 0.41 ± 0.07 (fixed) (p = 0.67). Our observation in the limited cases showed no substantial differences in the OFDI signal reflection regardless of tissue fixation. However, the results was acknowledged only in the normal neointima >1 year and organized thrombus, and was not confirmed in other neointimal features described in the main manuscript. Further, it is difficult to determine whether the absence of significant difference in the quantitative signal analysis derived from the plausible analogy or from the lack of statistical power. Therefore, further studies are required to confirm the results in a larger cohort of cases. 4 Supplemental Table 1. Difference of OFDI Signal from Unfixed and Formalin-fixed Tissue Unfixed Fixed P value Intensity Index 180.9 ± 5.0 182.1 ± 4.4 0.33 Attenuation Index 0.37 ± 0.17 0.37 ± 0.13 0.92 Intensity Index 136.1 ± 3.8 135.4 ± 3.8 0.62 Attenuation Index 0.40 ± 0.06 0.41 ± 0.07 0.67 Normal neointima >1 year (n = 6) Organized thrombus (n = 5) 5 Supplemental Figure 1. Human coronary histology with a stent implant with corresponding IVUS and OFDI A and B: histological sections of stented coronary artery segment (A: H&E; B: Movat, magnification ×12.5). A stent was implanted over a lesion with necrotic core (NC). Stent struts were observed on the luminal surface (black arrows). C: co-registered OFDI image. D: coregistered IVUS image. 6 Supplemental Figure 2. Example of strut identification in sequential frames in OFDI A: histological section of stented coronary artery. B to G: sequential OFDI images. Individual struts in the OFDI images were matched with the corresponding histological section. 7 Supplemental Figure 3. Atherosclerotic change in neointima with foam cell macrophage infiltration A: histological image shows lipid core (LC) formation deep inside neointima (Movat, magnification ×20). B: magnified image of the inset in A (×100). Macrophages with foam cell morphology are infiltrating the “shoulder” of a newly formed area of atherosclerosis in neointima (yellow arrows) (asterisk: fixation artifact). C: corresponding OFDI to image A. LC in histology appears dark without clear border. D: corresponding OFDI to image B. A narrow 8 signal-rich layer was observed in the area with macrophages in histology (white arrows). 9 Supplemental Figure 4. Thin cap fibroatheroma in neointima A: histological image shows a relatively small eccentric necrotic core (NC) near the luminal surface (Movat, magnification ×20). B: magnified image of the inset in A (×100). NC containing cholesterol crystals (area enclosed by yellow arrowheads) is covered by a thin fibrous cap. C: corresponding OFDI to image A. D: corresponding OFDI to image B. A thin, signal-rich layer was observed near the luminal surface, sequentially followed by signal attenuation in deeper intima. 10 Supplemental Figure 5. Other histological features identified in neointima A: histological image with sheet of calcification within neointima matrix (black arrows) (Movat, magnification ×20). B: corresponding OFDI to image A. The stent lumen was severely narrowed with neointimal tissues, in which a black mass sharply delineated with clear borders was identified. C: corresponding IVUS to image A. A strong signal with a trailing shadow was observed with less clear margins in the calcified area. D: histological image shows deep dissection in neointima. E: corresponding OFDI to image D. A discontinuation of neointimal surface is clearly identified. F: corresponding IVUS image shows a neointimal disruption but with poorer resolution compared to OFDI. 11 Supplemental Figure 6. Difference of OFDI appearance in unfixed and fixed tissue A: OFDI image of coronary artery >1 year following stent implantation. Right: magnified image of the inset in the left image demonstrating bright and homogeneous appearance of neointima above the strut. B: OFDI image acquired following formalin fixation. The neointimal tissue shows a similarity to the image in A. C: Histology corresponding to the images in A and B (Movat, magnification ×20). Right: Magnified image of the inset in the left image showing normal neointima consisting of smooth muscle cells and extracellular matrix such as proteoglycans (Movat, ×200). D: OFDI image of stented coronary segment with severe luminal narrowing. Right: magnified image of the inset in the left showing relatively dark, coarse tissue with various sizes of black holes (white arrows) (* lumen area). E: OFDI image acquired following formalin fixation. The tissue within the stent appears analogous to the image D, and 12 also has black holes (white arrows) (* lumen area). F: Histology corresponding to the images in D and E (Movat, ×20). Right: Magnified image of the inset in the left image showing sparse tissue rich in proteoglycans with various sizes of cavities (black arrows) representing angiogenesis in the organized thrombus (Movat, ×400). 13 Supplemental References 1. Finn AV, Joner M, Nakazawa G, et al. Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation 2007;115:243541. 2. Luna LG. Histologic Staining Methods of the Armed Forces Institute of Pathology. New York: McGrow-Hill Book Co, 1968. 14