Reply to reviewer comments 1 Line 112 – The flexor retinaculum is
advertisement

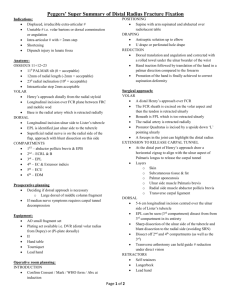
Reply to reviewer comments 1 Line 112 – The flexor retinaculum is found over the carpal tunnel and should not be incised during distal radius exposure. Reply: Agree! Omitted already. Line 113-114 – Can you elaborate what structures you may need to go through or retract before you expose the pronator quadratus fully? Reply: The FCR approach was used in this study. Namely, a longitudinal incision about 5 cm was made over the tendon of flexor carpi radialis (FCR). As the palmar cutaneous branch of the median nerve is almost always ulnar to the FCR tendon, the FCR tendon is then exposed by releasing its superficial sheath sharply. In addition, when releasing the sheath, one must be careful distally near the proximal wrist crease as the superficial branch of the radial artery crosses superficial to the sheath and runs from ulnar to radial. Upon releasing the FCR sheath, the FCR tendon is retracted radially. The deeper sheath and fascia under the FCR tendon are then released. At this point, dissection is done between the radial fascia and the FPL (flexor pollicis longus) muscle that runs deep to the fascia. The radial artery runs radial to the FCR tendon and superior to this fascia. Thus, when the radial fascia is retracted, the radial artery is protected. The FPL muscle must then be bluntly dissected and ulnar retraction be performed. The bed of the FCR tendon sheath was incised in line with the skin incision. Blunt dissection was then preformed to expose PQ. Line 116 – Do you perform brachioradialise muscle insertion release? Reply: For most of the cases it is not necessary to release brachioradialise muscle insertion.The flexor carpi radialis tendon is again retracted ulnarly, its gliding floor is divided longitudinally, and the brachioradialis tendon is retracted radially. Line 116 – Can you please describe how the volar capsulotomy is performed? This is important because of the risk of injury to the radioscaphocapitate ligaments and the radiolunate ligaments. Reply: Usually, a 21 gauge needle was used to check the distal border of the scaphoid and lunate fossa of radius. A minimal capsulotomy was performed to make sure the position as the reference point of measurement. Line 119 – Can you elaborate how the 2 K wires are positioned for temporary stabilization? Reply: The fracture is distracted and the achieved closed reduction is checked by fluoroscopy. When a good reduction has been achieved it is temporarily stabilized with two 1.8 mm Kirschner wires driven into the radial styloid in a distal to proximal direction . Line 122-126 – I think it would be of great benefit if you can diagrammatically illustrate how the measurements are made in a drawing or in a photo. Also, could you elaborate whether the measurements are projectional or along the surface of the bone? Reply: A vernier caliper was used to measure the distance along the surface of the bone. A diagram(Fig. 1) illustrates the measurements in this study. Fig. 1. A diagram demonstrates the relationship of distal radius and measurement of pronator quadratu, distance from distal edge of pronator quadratus to lunate or scaphoid fossa. Likewise, the distance from fracture site to lunate or scaphoid fossa could also be measured. PQ:pronator quadratus muscle. P-L:distance from pronator quadratus to lunate fossa, P-S: distance from pronator quadratus to scaphoid fossa Line 128 – 129 – Can you tell us if there is any tips that you use to help to align the longitudinal limb of the plate? Reply: The longitudinal limb of the plate was lined up with the radial shaft, and the position of the plate was adjusted under fluoroscopy. The more perfect alignment will be achieved then. Line 131-133 – How did you manage to retract the distal edge of the PQ? Was there a need to incise the soft tissue along the distal edge of the PQ to allow you to retract the muscle? Reply s: It is important to note that the fracture site is usually near distal edge of PQ or slightly covered by the pronator quadratus so that it is not necessary to divide this muscle. Gentle traction of PQ is enough. Line 158-164 – I think a diagram to illustrate your results would be of great benefit. Numbers like these may not give people much of an impression. Reply: Thanks. Table 1. The width of pronator quadratus and distances between pronator quadratus or fracture site to the distal radial edge. PQ: pronator quadratus; PQ-lunate:distance from pronator quadratus to lunate fossa; PQ-scaphoid: distance from pronator quadratus to scaphoid fossa; Fracture-lunate: distance from fracture site to lunate fossa; Fracture-scaphoid: distance from fracture site to scaphoid fossa. Mean(mm) Range(mm) PQ width 37.2 30-49 PQ-lunate 16.2 12-19 PQ-scaphoid 17.6 11-29 Fracture-lunate 12.2 7.3-17 Fracture-scaphoid 13.2 9.4-18.8 Line 186-189 – Did you manage to see the deep and superficial head of the PQ during your clinical study? Reply :Although Stuart reported that the superficial head of the PQ muscle is the prime mover in forearm pronation and the deep head is a dynamic stabilizer of the distal radioulnar joint. In this study, we did not try to identify these two portions. Others – I think it would be good to briefly report on union rate and time to union as one of the approaches of the PQ sparing technique is to preserve periosteal blood supply. Reply :Union was achieved in all fractures. The PQ vascularity was preserved in this technique. There is no statistical significance on union rate and time between PQ sparing technique and PQ incision technique. 2. Please also report on the operative time and comment whether it took longer to perform PQ sparing approach. Reply: Although it could save time to repair PQ, checked the plate alignment took some time. Totally, the operation time did not take shorter. 3. Functional outcome in terms of range of motion would also be good although it is not an objective of the study. Reply :Yes, I would like to demonstrate the functional outcome in another manuscript. 4. Also, we would like to know what the post op rehabilitation regime is like and whether it is different between the traditional approach versus the PQ sparing approach. Reply: Active motion of fingers and wrist are started at next day after surgery or 5 days after removal of temporary splint immobilization in some cases. 5. Can you tell us if you routinely use a drain and if this PQ approach makes a difference in drain use. Reply :We do not routinely use a drain in distal radiu s fracture. The PQ approach should make no difference in drain use. 6. Finally, could you show some x-rays of the results and also comment on plate position in your cases and whether plate alignment is likely to be better or worse in the PQ sparing approach. Reply :We did not compare plate alignment in the PQ sparing approach or PQ repairing approach, but we believe there will be no apparent difference.