Posture
advertisement
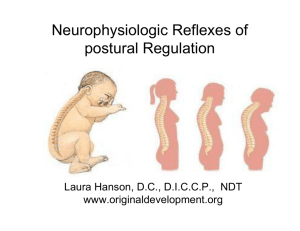
Posture Why is posture important? ability of an individual to maintain and adjust his or her overall body position so the extremities can be utilized to perform gross and fine motor tasks. Proximal stability for distal mobility Static Posture Body and its segments are aligned and maintained in a position Eg. Standing, sitting, lying Dynamic Posture The body and/or its segments are moving Eg. Walking, running, jumping, throwing, and lifting Postural Control A person’s ability to maintain stability of the body and body segments in response to forces that threaten to disturb the body’s structural equilibrium Static – maintenance of a stability against gravity Dynamic – maintenance of stability during movements of the body or body segments and/or changes in the supporting surface. However, even static postural control is NOT completely static. WHY? Sway – analyze center of pressure with force plate to see this. Sagittal plane – 120 Frontal plane - 160 What does postural control (balance) require? Intact CNS that can integrate and process a variety of inputs and then respond to these inputs Inputs 1 1. 2. 3. 4. Vision Vestibular Proprioception – muscle and joint receptors Sensation – tactile and pressure Output from CNS 1. Instructions to certain muscles to fire What happens when one or more of these inputs are impaired? 1. postural control is altered/reduced 2. body compensates by depending on the other intact inputs Examples of altered/impaired inputs Astronauts in weightless – What is altered? 1. proprioception 2. tactile 3. vestibular Can a sprained ankle alter one’s postural control? Why? Altered kinesthesia secondary to stretching of ligaments and joint capsule Postural control or balance has most recently been studied via perturbation studies. These studies have helped identify three different strategies/patterns for maintaining postural control. 1. Ankle 2. Hip 3. Stepping The strategy used depends on: 1. magnitude/intensity of the perturbation 2. limitations in other strategies (ROM, ligamentous strategies, etc. 2 Ankle strategy posterior perturbation of surface results in activation of anterior musculature dorsiflexors, hip flexors, abdominals, neck flexors Hip strategy 20: limitation in ankle motion excessive velocity of perturbation excessive displacement standing on unstable surface where ankle strategy is ineffective posterior perturbation of surface results in a forward sway & activation of anterior musculature: hip flexor and abdominal musculature Stepping strategy 20: excessive displacement or velocity ineffective ankle and/or hip strategies posterior perturbation forward step to prevent falling when limits of stability have been exceeded line of gravity falls outside the base of support Forces that affect postural control or equilibrium: same as gait External 1. gravity 2. ground reaction forces 3. inertia Internal 1. muscle activity 2. passive tension of ligaments, tendons, capsules, etc. Relationship of Line of Gravity and Postural Control COG anterior to S2 3 Static Optimal Posture Ankle – just anterior to lateral malleolus dorsiflexion moment soleus activity Knee – just anterior to anterior to knee extension moment passive structures (posterior capsule & ligaments) Hip – through the greater trochanter (slightly posterior to hip joint) extension moment passive structures (iliofemoral, pubofemoral, ischiofemoral) L/S – LOG passes thru body of L5 which is anterior to the other lumbar vertebrae extension moment resisted by the anterior longitudinal ligament Head – LOG thru external auditory meatus falls anterior to AOR flexion moment ligamentum nuchae, tectorial membrane, neck extensors What happens if there are deviations from this normal posture? effectively the moment arm/torque being applied to a joint thus requiring more torque/force to counteract this torque Where is this additional force/torque coming from? 1. muscular activity 2. stress on passive structures Deviations from Optimal Posture What is the concern with deviations from optimal posture? 1. energy expenditure 20 to muscular activity 2. stress on supporting structures injury 4 Lateral View 1. 2. 3. 4. 5. 6. 7. Forward head posture Excessive anterior tilt Sway-back posture Flat-back posture Military posture Flexed knee posture Genu recurvatum Anterior/Posterior view 1. 2. 3. 4. 5. 6. 7. 8. Scoliosis – primary vs. compensatory curves Genu valgum – “knock knees” Genu varum – “bow-legged” Pes planus Pes cavus Hallux valgus Toe clawing – active vs. passive Hammer toe – extension of MTP and DIP w/ flexion of PIP Proposed sequence of events for adolescent idiopathic scoliosis: 1. failure in the supporting and/or control systems 2. lateral flexion moment 3. deviation of the vertebrae w/ rotation 4. compression of the vertebral body (concave-side) 5. inhibition of growth of vertebral body (concave-side) 6. wedging of vertebra 7. head out of line w/ sacrum 8. compensatory curve 9. adaptive shortening of muscle (concave –side) 10.stretching of muscles and passive structures (convex-side) What factors affect postural control? 1. Age 2. Pregnancy 3. Lifestyle / occupation Relationship of Posture to RSIs (Repetitive Strain Injuries) 5