Original Research Annals of Internal Medicine Opportunistic
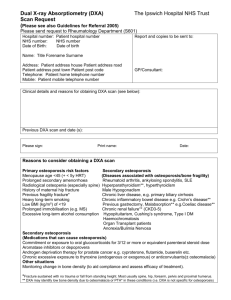
advertisement
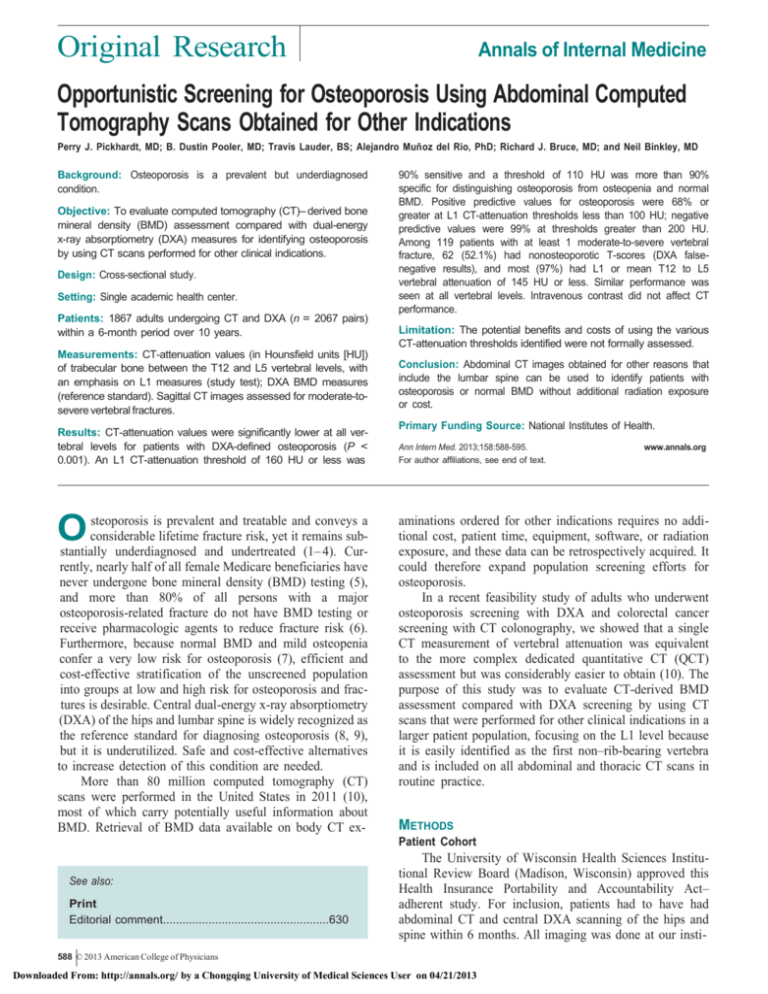
Original Research Annals of Internal Medicine Opportunistic Screening for Osteoporosis Using Abdominal Computed Tomography Scans Obtained for Other Indications Perry J. Pickhardt, MD; B. Dustin Pooler, MD; Travis Lauder, BS; Alejandro Muñ oz del Rio, PhD; Richard J. Bruce, MD; and Neil Binkley, MD Background: Osteoporosis is a prevalent but underdiagnosed condition. Objective: To evaluate computed tomography (CT)– derived bone mineral density (BMD) assessment compared with dual-energy x-ray absorptiometry (DXA) measures for identifying osteoporosis by using CT scans performed for other clinical indications. Design: Cross-sectional study. Setting: Single academic health center. Patients: 1867 adults undergoing CT and DXA (n = 2067 pairs) within a 6-month period over 10 years. Measurements: CT-attenuation values (in Hounsfield units [HU]) of trabecular bone between the T12 and L5 vertebral levels, with an emphasis on L1 measures (study test); DXA BMD measures (reference standard). Sagittal CT images assessed for moderate-tosevere vertebral fractures. Results: CT-attenuation values were significantly lower at all vertebral levels for patients with DXA-defined osteoporosis (P < 0.001). An L1 CT-attenuation threshold of 160 HU or less was O steoporosis is prevalent and treatable and conveys a considerable lifetime fracture risk, yet it remains substantially underdiagnosed and undertreated (1– 4). Currently, nearly half of all female Medicare beneficiaries have never undergone bone mineral density (BMD) testing (5), and more than 80% of all persons with a major osteoporosis-related fracture do not have BMD testing or receive pharmacologic agents to reduce fracture risk (6). Furthermore, because normal BMD and mild osteopenia confer a very low risk for osteoporosis (7), efficient and cost-effective stratification of the unscreened population into groups at low and high risk for osteoporosis and fractures is desirable. Central dual-energy x-ray absorptiometry (DXA) of the hips and lumbar spine is widely recognized as the reference standard for diagnosing osteoporosis (8, 9), but it is underutilized. Safe and cost-effective alternatives to increase detection of this condition are needed. More than 80 million computed tomography (CT) scans were performed in the United States in 2011 (10), most of which carry potentially useful information about BMD. Retrieval of BMD data available on body CT ex- 90% sensitive and a threshold of 110 HU was more than 90% specific for distinguishing osteoporosis from osteopenia and normal BMD. Positive predictive values for osteoporosis were 68% or greater at L1 CT-attenuation thresholds less than 100 HU; negative predictive values were 99% at thresholds greater than 200 HU. Among 119 patients with at least 1 moderate-to-severe vertebral fracture, 62 (52.1%) had nonosteoporotic T-scores (DXA falsenegative results), and most (97%) had L1 or mean T12 to L5 vertebral attenuation of 145 HU or less. Similar performance was seen at all vertebral levels. Intravenous contrast did not affect CT performance. Limitation: The potential benefits and costs of using the various CT-attenuation thresholds identified were not formally assessed. Conclusion: Abdominal CT images obtained for other reasons that include the lumbar spine can be used to identify patients with osteoporosis or normal BMD without additional radiation exposure or cost. Primary Funding Source: National Institutes of Health. Ann Intern Med. 2013;158:588-595. For author affiliations, see end of text. www.annals.org aminations ordered for other indications requires no additional cost, patient time, equipment, software, or radiation exposure, and these data can be retrospectively acquired. It could therefore expand population screening efforts for osteoporosis. In a recent feasibility study of adults who underwent osteoporosis screening with DXA and colorectal cancer screening with CT colonography, we showed that a single CT measurement of vertebral attenuation was equivalent to the more complex dedicated quantitative CT (QCT) assessment but was considerably easier to obtain (10). The purpose of this study was to evaluate CT-derived BMD assessment compared with DXA screening by using CT scans that were performed for other clinical indications in a larger patient population, focusing on the L1 level because it is easily identified as the first non–rib-bearing vertebra and is included on all abdominal and thoracic CT scans in routine practice. METHODS Patient Cohort See also: Print Editorial comment...................................................630 The University of Wisconsin Health Sciences Institutional Review Board (Madison, Wisconsin) approved this Health Insurance Portability and Accountability Act– adherent study. For inclusion, patients had to have had abdominal CT and central DXA scanning of the hips and spine within 6 months. All imaging was done at our insti- 588 © 2013 American College of Physicians Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 CT Screening for Osteoporosis tution over 10 years ending in December 2009; image retrieval and study analyses were performed between 2010 and 2012. Original Research Context Osteoporosis is underdiagnosed. Dual-Energy X-Ray Absorptiometry Contribution Dual-energy x-ray absorptiometry of the lumbar spine and proximal femora was performed using standard techniques on Lunar Prodigy densitometers (GE Healthcare, Waukesha, Wisconsin). Patients were categorized as having osteoporosis (T-score 三 2.5 or the presence of a moderate-to-severe vertebral compression fracture), osteopenia (T-score between 1.0 and 2.5), or normal BMD (T-score 三 1.0) by using the lowest reported Tscore (8, 11). Because low BMD at 1 site carries an increased risk for fracture at other sites (12, 13), patients are generally categorized and managed according to their lowest central T-score. Furthermore, in a substantial subset of cases, T-scores for 1 of the 2 central sites are not reported for various technical reasons. At least 1 valid reported T-score for the lumbar spine or hips was required for study inclusion. This study found that computed tomography (CT) scans can be used for detecting vertebral osteoporosis by comparing CT scans obtained for other reasons with dualenergy x-ray absorptiometry (DXA) scans performed within 6 months of the CT. Approximately half of patients with CT-identified osteoporotic vertebral compression fractures had nonsteoporotic T-scores (DXA false-negative results). Computed Tomography Abdominal CT was done using multidetector CT scanners (LightSpeed Series, GE Healthcare) calibrated daily to ensure accurate vertebral CT-attenuation numbers, which reflect underlying BMD (Figure 1). We retrospectively accessed the CT images and evaluated vertebral BMD on a standard radiology picture archiving and communication system workstation, with images viewed in soft tissue and bone windows (windows define gray-scale assignment of the image display to emphasize particular tissues and do not influence attenuation or BMD values [Figure 1]) (14). We assessed vertebral BMD by placing a single oval click-and-drag region of interest (ROI) over an area of vertebral body trabecular bone and then measuring CT attenuation in Hounsfield units (HU), with lower HU (lower attenuation) representing less-dense bone, at each of the T12 through L5 levels (Figures 1 and 2); this process is identical to that used for measuring CT attenuation for other clinical conditions (for example, adrenal adenomas, renal lesion enhancement, and fatty liver assessment). We avoided placing the ROI near areas that would distort the BMD measurement (posterior venous plexus; focal heterogeneity or lesion, including compression fracture; and imaging-related artifacts). We assessed the presence of vertebral compression fractures by using sagittal CT views of the lumbar spine (Figure 2, B) by employing the Genant visual semiquantitative method (15), a widely accepted way of assessing vertebral fractures on conventional radiography that can be easily applied to sagittal CT images. We counted only obvious moderate (grade 2, 25% to 40% loss of height) or severe (grade 3, >40% loss of height) compression deformities to avoid ambiguity related to more subjective borderline or mild compression deformities. All potential moderate-to-severe compression fractures identified on the www.annals.org Caution Osteoporosis treatment is often initiated based on hip fracture risk. The relationship between hip fracture risk and bone mineral density (BMD) is stronger for hip than for spine BMD measures. Implication CT scans obtained for other reasons can be used for opportunistic osteoporosis screening without additional radiation exposure or cost. —The Editors initial review were verified in a separate reading session for final confirmation, further excluding any questionable mild fractures. Statistical Analysis We used Kruskal–Wallis tests to compare CTattenuation values within BMD categories at each vertebral level (T12 to L5). We constructed kernel-density plots of L1 CT attenuation for normal, osteopenic, and osteoporotic groups by using a Gaussian kernel with bandwidth selected according to the Silverman rule of thumb. We calculated sensitivity and specificity, positive and negative predictive values (PPVs and NPVs), and positive and negative likelihood ratios for CT imaging compared with DXA imaging across the range of observed CT-attenuation values at 5-HU increments to establish thresholds that would yield high sensitivity (about 90%), high specificity (about 90%), or a balance between the 2 for distinguishing osteoporosis from nonosteoporosis (osteopenia and normal BMD) and normal BMD from low BMD (osteoporosis and osteopenia). We calculated adjusted Wald (“approximate”) 95% CIs for proportions (for example, sensitivity and specificity) (16) and based the 95% CIs for PPV and NPV on the logarithmic method (17). We also report findings for more extreme thresholds (<100 HU and >200 HU) intended to further increase specificity for osteoporotic and normal populations, and we report CT–DXA cross-classifications at thresholds that divide the study sample approximately evenly among BMD categories. 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 589 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 Original Research CT Screening for Osteoporosis Figure 1. Trabecular L1 CT-attenuation values for BMD assessment on body CT scans. Example of axial CT images at the L1 vertebral level in 4 patients (A through D) viewed in standard soft tissue (row 1) and bone (row 2) window settings. Trabecular bone CT-attenuation values are shown in red for each oval region of interest; note that the attenuation measure (in HU) does not change according to the CT window for viewing. The 4 patients represent sample BMDs ranging from low (osteoporosis) (A) to high (normal) (D), which is more visually apparent on the soft tissue window setting (row 1). Assuming a study-derived CT-attenuation threshold for osteoporosis of 三145 HU (see Results section for details), patient A has osteoporosis by both CT (attenuation value, 20 HU; L2 vertebral fracture [not shown]) and DXA (T-scores for both lumbar spine and hip, 4.0). Patient B has osteoporosis by CT (attenuation value, 93 HU; severe L4 vertebral fracture [not shown]) and osteopenia by DXA (lumbar spine T-score, 2.2; hip T-score, 1.6). Patient C has osteopenia by CT (attenuation value, 148 HU) and DXA (lowest T-score, 1.6). Patient D has normal BMD by CT (attenuation value, 210 HU) and DXA (lowest T-score, 0.1). BMD = bone mineral density; CT = computed tomography; DXA = dual-energy x-ray absorptiometry. We assessed CT performance across all thresholds for L1 and all vertebral levels by using empirical receiveroperating characteristic (ROC) curve analysis (18). The ROC analyses derive from univariate logistic regression models, where DXA-based osteoporosis was the dependent variable and CT attenuation the independent variable. We also performed multivariable logistic regression by using all 6 single-level T12 to L5 attenuations as dependent variables; the linear predictor was then used to construct ROC curves. We assessed areas under the ROC curve (AUCs) and corresponding 95% confidence limits for each vertebral level and compared the values by using a nonparametric approach (19). In additional analyses, we compared CT performance with and without intravenous contrast administration (because venous enhancement could potentially elevate ROIattenuation values through volume-averaging effects). Statistical calculations and graphics were performed using R, version 2.12.2 (R Development Core Team, Vienna, Austria) (20). Role of the Funding Source The National Institutes of Health funded this study. The funding source had no role in study design, conduct, or analysis or the decision to submit the manuscript for publication. RESULTS The study comprised 2063 CT–DXA pairs in 1867 adults (1511 women [81%]; mean age, 59.2 years [SD, 12.5]). The median time between abdominal CT and DXA studies was 67 days (interquartile range, 27 to 118 days). Abdominal CT was done for various clinical indications, most commonly for suspected mass or oncologic work-up (n = 414); genitourinary (n = 402) or gastrointestinal (n = 398) reasons, including virtual colonoscopy; and unexplained abdominal pain or symptoms (n = 374) (Appendix Table 1, available at www.annals.org). Of the 2063 CT scans, 1126 (54.6%) were obtained after intravenous contrast administration; the remainder were unenhanced. Fewer than 10% of patients contributed more than 1 CT–DXA pair because of imaging without and with contrast; analyses restricted to 1 CT–DXA pair per patient resulted in absolute changes to sensitivity or specificity less than 1% for all thresholds. The DXA screening reference standard categorized patients as osteoporotic (22.9%), osteopenic (44.8%), and normal (32.3%); BMD categories at hip and vertebral levels differed in approximately half the study population (Appendix Tables 2 and 3, available at www.annals.org). Computed tomography–attenuation values differed signif- 590 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 www.annals.org CT Screening for Osteoporosis icantly for the 3 DXA-defined BMD categories at all vertebral levels (P < 0.001) (Appendix Figure 1, available at www.annals.org). Figure 3 shows the overlap of DXAdefined BMD categories by L1 CT attenuation; Figure 4 is a scatterplot of L1 CT-attenuation values and DXA T-scores. An L1 CT-attenuation threshold of 160 HU was 90% sensitive and a threshold of 110 HU was more than 90% specific for distinguishing osteoporosis from osteopenia and normal BMD; a threshold of 135 HU resulted in a balanced sensitivity and specificity of approximately 75% for each (Table 1). A CT-attenuation threshold intended to increase specificity for osteoporosis (<100 HU) yielded a PPV for osteoporosis of 68.4%; most (82%) “falsepositive” cases were classified as osteopenic by DXA. Appendix Table 4 (available at www.annals.org) shows CT–DXA cross-classifications at thresholds that divide the study sample approximately evenly among BMD categories. The AUC across CT thresholds at L1 to distinguish osteoporosis from osteopenia or normal BMD (Figure 5) Original Research was 0.83 (95% CI, 0.81 to 0.85) without a significant difference between intravenous contrast– enhanced (AUC, 0.84) and unenhanced (AUC, 0.83) CT scans (P = 0.91). The AUCs were statistically similar in subsets of patients stratified by year (2000 to 2003, 2004 to 2005, 2006 to 2007, and 2008 to 2010) to account for changes in diagnostic technology or procedures over the study period (data not shown). Table 2 shows the diagnostic accuracy of CT for distinguishing normal from abnormal BMD (osteopenia and osteoporosis); an L1 CT-attenuation threshold of 135 HU was approximately 90% sensitive, and a threshold of 190 HU was 90% specific. A CT-attenuation threshold intended to increase specificity for normal BMD (>200 HU) yielded an NPV for osteoporosis of 99%; Appendix Figure 2 (available at www.annals.org) shows the change in PPV and NPV for osteoporosis across CT thresholds from 75 to 200 HU. The AUC across thresholds at L1 to distinguish normal from abnormal BMD was 0.80 (CI, 0.78 to 0.82). Figure 2. Opportunistic osteoporosis screening at abdominal CT in a 59-year-old woman undergoing colorectal cancer screening (with CT colonography). CT = computed tomography; DXA = dual-energy x-ray absorptiometry. A. Axial CT image at the L1 vertebral level viewed in a bone window setting shows appropriate placement of the oval region of interest in the trabecular bone. The CT-attenuation value of 109 HU places this patient in the lowest quintile, raising concern for osteoporosis. B. Sagittal CT view shows a moderate T12 compression fracture (arrow). Note that higher thoracic vertebral bodies are also sometimes included on abdominal CT scans. C and D. DXA evaluation of the hips (C) and lumbar spine (D) performed 3 mo later demonstrated osteopenic T-scores ranging from 1.1 to 1.9 (lowest T-score of 1.9 from L1 to L4 evaluation). Therefore, this represents a DXA falsenegative result. www.annals.org 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 591 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 CT Screening for Osteoporosis Computed tomography performed similarly at other (non-L1) vertebral levels (Appendix Table 5 and Appendix Figure 3, available at www.annals.org); attenuation thresholds targeted to yield sensitivity and specificity of approximately 90% varied slightly at each level because of the small average decrease in attenuation values toward the L3 level (Appendix Figure 1). The AUCs were similar using single-level vertebral measurements, a single multilevel (T12 to L5) average, and more complex model-based multilevel measures (Appendix Figure 3). One hundred nineteen patients had at least 1 moderate or severe vertebral fracture (35 with fractures at multiple vertebral levels), 62 (52.1%) of whom had either osteopenic (n = 50) or normal (n = 12) DXA T-scores (Figures 2 and 4). Presumed degenerative changes were noted in DXA evaluation in most of these false-negative cases, which may have resulted in spurious T-score results. Vertebral level L1 attenuation (or mean vertebral attenuation if L1 itself was involved by fracture) was 145 HU or less in 115 (96.6%) of these patients, compared with 39.0% of patients with a T-score greater than 2.5 and no fracture. Figure 4 shows the generalized decrease in vertebral CT attenuation among patients with fractures, despite a range of DXA T-scores encompassing normal values. Figure 4. L1 CT-attenuation values and corresponding DXA T-scores. 400 L1 CT Attenuation, HU Original Research 300 200 100 0 –6 –5 –4 –3 –2 –1 0 1 2 3 4 DXA T-Score Normal (T-score ≥ –1) Mild osteopenia (–1.5 < T-score < –1) Moderate osteopenia (–2 < T-score ≤ –1.5) Advanced osteopenia (–2.5 < T-score ≤ –2) Osteoporosis (T-score ≤ –2.5) DISCUSSION In this study of the diagnostic accuracy of a simple BMD screening method for adults who have undergone abdominal CT imaging for other clinical indications, we report results suggesting that CT images could be used to identify patients with osteoporosis or normal BMD. The Figure 3. Distributions of L1 CT-attenuation values in Compression fracture The black circles represent patients with CT-detected T12 to L5 compression fractures (not shown here are 15 patients with L1 compression fractures where reliable CT-attenuation measurement at this level was not possible). Note the broad range of DXA T-scores among patients with vertebral fracture, including normal scores. Overall, more than half of all patients with fractures had a nonosteoporotic DXA T-score, but 97% had an L1 or mean vertebral attenuation 三145 HU. CT = computed tomography; DXA = dual-energy x-ray absorptiometry. normal, osteopenic, and osteoporotic cohorts. BMD category, by DXA 0.012 Normal (T-score ≥ –1) Osteopenia (–2.5 < T-score < –1) Relative Frequency 0.010 Osteoporosis (T-score ≤ –2.5) 0.008 0.006 0.004 0.002 0.000 0 100 200 300 400 500 L1 CT Attenuation, HU Based on lowest central DXA T-score. BMD = bone mineral density; CT = computed tomography; DXA = dual-energy x-ray absorptiometry. method that we used requires a negligible amount of training and time; could be applied prospectively by the interpreting radiologist or retrospectively by a radiologist or even nonradiologist; adds no cost; and requires no additional patient time, equipment, software, or radiation exposure. It should not be confused with QCT, which is more labor-intensive; requires an imaging phantom or angle-corrected ROI measurement of bone, muscle, and fat at multiple levels (21); and involves additional money, time, and radiation exposure. Current QCT-derived Tscores do not directly correspond to DXA T-scores, limiting QCT clinical utility (21). We previously showed that the simpler approach used in this study was as or more effective and more reproducible than spine QCT for predicting DXA results (14). Although optimal implementation of this method of CT screening for osteoporosis remains to be determined, our data suggest ways that it could be used in practice, depending on clinical objectives. Identifying persons with very low BMD by CT (for example, <100 HU at L1) 592 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 www.annals.org Original Research CT Screening for Osteoporosis Table 1. Performance Characteristics of L1 CT-Attenuation Values for Distinguishing Osteoporosis From Nonosteoporosis in 2040 CT– DXA Pairs* Variable Threshold Selected for Achieving High Sensitivity (About 90%) Threshold Selected for Achieving High Specificity (About 90%) Threshold Selected for Balanced Sensitivity and Specificity L1 CT attenuation, HU 三160 三110 三135 Sensitivity TP/(TP + FN), n/N Sensitivity (95% CI), % 415/461 90.0 (86.9–92.4) 240/461 52.1 (47.5–56.6) 348/461 75.5 (71.4–79.2) Specificity TN/(TN + FP), n/N Specificity (95% CI), % 826/1579 52.3 (49.8–54.8) 1441/1579 91.3 (89.8–92.6) 1190/1579 75.4 (73.2–77.4) PPV TP/(TP + FP), n/N PPV (95% CI), % 415/1168 35.5 (32.8–38.3) 240/378 63.5 (58.5–68.2) 348/737 47.2 (43.6–50.8) NPV TN/(TN + FN), n/N NPV (95% CI), % 826/872 94.7 (93.0–96.0) 1441/1662 86.7 (85.0–88.2) 1190/1303 91.3 (89.7–92.7) Positive likelihood ratio (95% CI) 1.89 (1.78–2.00) 5.96 (4.97–7.14) 3.06 (2.77–3.39) Negative likelihood ratio (95% CI) 0.19 (0.14–0.25) 0.53 (0.48–0.58) 0.33 (0.28–0.38) CT = computed tomography; DXA = dual-energy x-ray absorptiometry; FN = false-negative; FP = false-positive; NPV = negative predictive value; PPV = positive predictive value; TN = true-negative; TP = true-positive. * “Nonosteoporosis” is defined as having osteopenia or normal bone mineral density. In this table, osteopenia and normal bone mineral density (according to the DXA T-score) are considered negative findings. Patients with moderate or severe compression fractures were categorized as osteoporotic. The total number of CT scans is fewer than 2063 because L1 attenuation could not be reliably measured in 23 cases. www.annals.org Figure 5. Receiver-operating characteristic curves for predicting osteoporosis by using CT attenuation at L1. 1.0 0.8 0.6 Sensitivity might allow for rapid identification of high-risk cohorts in whom further evaluation or treatment is warranted. Determining persons with high-normal BMD by CT (for example, >200 HU at L1) might effectively exclude osteoporosis and would probably make DXA unnecessary. For L1 trabecular CT-attenuation values between 100 and 200 HU, or for all patients across the range of attenuation values, various thresholds or ranges could be considered, perhaps on the basis of pretest probability or a priori risk. For example, an L1 CT-attenuation threshold of 160 HU (90% sensitive for distinguishing osteoporosis from nonosteoporosis) may be suitable for high-risk cohorts where the aim is to minimize false-negative results; a substantial subset of osteopenia cases would be included in this population, leading to low test specificity. Alternatively, an L1 threshold of 110 HU (91% specific) may be prudent for groups considered at lower risk to minimize false-positive results yet still detect approximately half (52%) of patients with osteoporosis. Other CTattenuation thresholds or vertebral levels can be used, depending on the population and screening objectives. One clear advantage of CT over DXA BMD screening is its ability to accurately identify unsuspected osteoporotic compression fractures, which clearly diagnose osteoporosis independent of the patient’s DXA T-score (1). Osteopenic and normal DXA T-scores were prevalent among patients with vertebral fractures in our study and in others (22, 23); this finding highlights the limitations of DXA, particularly in terms of BMD overestimation related to degenerative 0.4 0.2 All (AUC, 0.83 [95% CI, 0.81–0.85]) Contrast (AUC, 0.84 [95% CI, 0.81–0.87]) No contrast (AUC, 0.83 [95% CI, 0.79–0.86]) 0. 0 0.0 0.2 0.4 0.6 0.8 1.0 1 – Specificity Receiver-operating characteristic curves for the L1 vertebral level show no statistically significant difference in AUC for CT scans performed with and without intravenous contrast (P = 0.91). However, further investigation is needed to determine whether any adjustment in specific CT-attenuation thresholds is necessary. AUC = area under the receiveroperating characteristic curve; CT = computed tomography. 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 593 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 Original Research CT Screening for Osteoporosis Table 2. Performance Characteristics of L1 CT Attenuation for Distinguishing Normal From Low Bone Mineral Density in 2040 CT–DXA Pairs* Variable Threshold Selected for Achieving High Sensitivity (About 90%) Threshold Selected for Achieving High Specificity (About 90%) Threshold Selected for Balanced Sensitivity and Specificity L1 CT attenuation, HU 三135 三190 三160 Sensitivity TP/(TP + FN), n/N Sensitivity (95% CI), % 549/613 89.6 (86.9–91.7) 284/613 46.3 (42.4–50.3) 453/613 73.9 (70.3–77.2) Specificity TN/(TN + FP), n/N Specificity (95% CI), % 669/1427 46.9 (44.3–49.5) 1286/1427 90.1 (88.5–91.6) 1008/1427 70.6 (68.2–72.9) PPV TP/(TP + FP), n/N PPV (95% CI), % 549/1307 42.0 (39.4–44.7) 284/425 66.8 (62.2–71.1) 453/872 51.9 (48.6–55.2) NPV TN/(TN + FN), n/N NPV (95% CI), % 669/733 91.3 (89.0–93.1) 1286/1615 79.6 (77.6–81.5) 1008/1168 86.3 (84.2–88.2) Positive likelihood ratio (95% CI) 1.69 (1.59–1.78) 4.69 (3.92–5.60) 2.52 (2.29–2.76) Negative likelihood ratio (95% CI) 0.22 (0.18–0.28) 0.60 (0.55–0.64) 0.37 (0.32–0.42) CT = computed tomography; DXA = dual-energy x-ray absorptiometry; FN = false-negative; FP = false-positive; NPV = negative predictive value; PPV = positive predictive value; TN = true-negative; TP = true-positive. * “Nonosteoporosis” is defined as having osteopenia or normal bone mineral density. In this table, osteopenia (according to the DXA T-score) is combined with osteoporosis; normal bone mineral density is considered a positive result. Patients with moderate or severe compression fractures were categorized as having osteoporosis. The total number of CT scans is fewer than 2063 because L1 attenuation could not be reliably measured in 23 cases. changes (1, 24). Vertebral CT-attenuation values tended to be low at levels other than the site of fractures in our study, and the fractures themselves were readily visible on the sagittal views. Our observations are consistent with prior studies documenting that many patients without osteoporosis diagnosed by DXA will sustain fragility fractures (22, 23) and suggest that CT attenuation may be a more accurate risk indicator. Another possible advantage of CT over DXA screening is its scalability. We are currently assessing automation of CT BMD screening that would permit evaluation of numerous patients within the picture archiving and communication system file storage. Future refinements in appropriate population-specific CT-attenuation thresholds could be derived from large retrospective (or prospective) cohorts. In the future, it may even be possible to incorporate CT-attenuation data into fracture risk assessment tools, such as the FRAX tool (World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom) (25). We emphasize L1 vertebral measures in this study for several reasons. First, the results at L1 are as or more accurate than the results at other levels, including multilevel assessment. The L1 level is easily identified, which improves efficiency and reproducibility. It is included on all standard chest and abdominal CT scans, substantially increasing its potential for higher overall screening yield. Accuracy was unaffected by the presence or absence of intravenous contrast. Furthermore, the measurement can be applied retrospectively, because CT scans are now typically stored indefinitely in most electronic medical records (picture archiving and communication systems). Our study has limitations. Fracture risk prediction and osteoporosis treatment decisions are often determined by DXA-based hip T-scores. Our analysis is based on vertebral measures and excludes assessment of risk factors for clinical fracture important to the FRAX tool and other fracture risk calculators (26, 27). Computed tomographic evaluation of the hip for BMD assessment is much more complex than the simple lumbar assessment that we propose, and we are currently investigating the potential for deriving a DXA-equivalent T-score for the hips from standard pelvic CT scans by using a dedicated software tool. Our analysis is also based on DXA measures as a reference standard for assessing BMD, but the patients with vertebral fractures and osteopenia or normal BMD by DXA in our study highlight the limitations of use of DXA as a reference standard. This finding suggests that, in a clinical setting, cases with nonosteoporotic T-scores but very low CT-attenuation values may warrant further investigation for overlying degenerative changes. Finally, we did not formally assess the potential benefits and costs of using the CT thresholds that we identified, but we speculate that increasing detection of osteoporosis, with subsequent appropriate treatment to reduce fracture risk, combined with reducing the number of normal DXA studies, would be expected to yield substantial health care cost savings (28). 594 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 www.annals.org CT Screening for Osteoporosis In conclusion, we demonstrate how routine abdominal CT scans obtained for other clinical indications can be used for opportunistic osteoporosis screening without the need for additional imaging, radiation exposure, cost, equipment, or patient time. We also report accuracy statistics for various CT-attenuation thresholds, use of which would vary depending on clinical and population screening objectives. Refinement of our techniques and confirmation of these findings might justify more routine reporting of vertebral trabecular attenuation with readings of abdominal CT evaluations performed for any reason. From the University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin. Grant Support: By the National Institutes of Health (grants 1R01CA144835-01 and 1R01CA169331-01). Potential Conflicts of Interest: Disclosures can be viewed at www .acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum =M12-1803. Reproducible Research Statement: Study protocol and data set: Not available. Statistical code: Available from Dr. Pickhardt (e-mail, ppickhardt2@uwhealth.org). Requests for Single Reprints: Perry J. Pickhardt, MD, Department of Radiology, University of Wisconsin School of Medicine and Public Health, E3/311 Clinical Science Center, 600 Highland Avenue, Madison, WI 53792-3252; e-mail, ppickhardt2@uwhealth.org. Current author addresses and author contributions are available at www.annals.org. References 1. Raisz LG. Clinical practice. Screening for osteoporosis. N Engl J Med. 2005; 353:164-71. [PMID: 16014886] 2. Ebeling PR. Clinical practice. Osteoporosis in men. N Engl J Med. 2008;358: 1474-82. [PMID: 18385499] 3. Bessette L, Ste-Marie LG, Jean S, Davison KS, Beaulieu M, Baranci M, et al. The care gap in diagnosis and treatment of women with a fragility fracture. Osteoporos Int. 2008;19:79-86. [PMID: 17641811] 4. Metge CJ, Leslie WD, Manness LJ, Yogendran M, Yuen CK, Kvern B; Maximizing Osteoporosis Management in Manitoba Steering Committee. Postfracture care for older women: gaps between optimal care and actual care. Can Fam Physician. 2008;54:1270-6. [PMID: 18791104] 5. King AB, Fiorentino DM. Medicare payment cuts for osteoporosis testing reduced use despite tests’ benefit in reducing fractures. Health Aff (Millwood). 2011;30:2362-70. [PMID: 22147865] 6. Leslie WD, Giangregorio LM, Yogendran M, Azimaee M, Morin S, Metge C, et al. A population-based analysis of the post-fracture care gap 1996-2008: the situation is not improving. Osteoporos Int. 2012;23:1623-9. [PMID: 21476038] 7. Gourlay ML, Fine JP, Preisser JS, May RC, Li C, Lui LY, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-33. [PMID: 22256806] 8. Lewiecki EM, Gordon CM, Baim S, Leonard MB, Bishop NJ, Bianchi ML, et al. International Society for Clinical Densitometry 2007 Adult and Pediatric Official Positions. Bone. 2008;43:1115-21. [PMID: 18793764] www.annals.org Original Research 9. Conry CM, Main DS, Miller RS, Iverson DC, Calonge BN. Factors influencing mammogram ordering at the time of the office visit. J Fam Pract. 1993; 37:356-60. [PMID: 8409889] 10. IMV. IMV 2011 CT Market Outlook Report. Des Plaines, IL: IMV Medical Information Division; 2011. 11. National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, DC: National Osteoporosis Foundation; 2010. 12. Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM, et al. Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom. 2008;11:75-91. [PMID: 18442754] 13. Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996; 312:1254-9. [PMID: 8634613] 14. Pickhardt PJ, Lee LJ, del Rio AM, Lauder T, Bruce RJ, Summers RM, et al. Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res. 2011;26:2194-203. [PMID: 21590738] 15. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137-48. [PMID: 8237484] 16. Agresti A, Coull B. Approximate is better than “exact” for interval estimation of binomial proportions. The American Statistician. 1998;52:119-26. 17. Confidence interval and statistical guidelines. In: Altman D, Machin D, Bryant T, MJ Gardiner, eds. Statistics with Confidence. 2nd ed. London: BMJ Books; 2000:109-10. 18. Lumley T. Programmer’s niche: ROC curves. R News. 2004. 19. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837-45. [PMID: 3203132] 20. R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. 21. Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, et al. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom. 2008;11:123-62. [PMID: 18442757] 22. Siris ES, Brenneman SK, Barrett-Connor E, Miller PD, Sajjan S, Berger ML, et al. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2006;17:56574. [PMID: 16392027] 23. Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004;34:195-202. [PMID: 14751578] 24. Yu W, Glüer CC, Fuerst T, Grampp S, Li J, Lu Y, et al. Influence of degenerative joint disease on spinal bone mineral measurements in postmenopausal women. Calcif Tissue Int. 1995;57:169-74. [PMID: 8574931] 25. Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385-97. [PMID: 18292978] 26. Hans DB, Kanis JA, Baim S, Bilezikian JP, Binkley N, Cauley JA, et al; FRAX Position Development Conference Members. Joint Official Positions of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX. Executive Summary of the 2010 Position Development Conference on Interpretation and use of FRAX in clinical practice. J Clin Densitom. 2011;14:171-80. [PMID: 21810521] 27. Kanis JA, McCloskey EV, Johansson H, Oden A, Ström O, Borgström F. Development and use of FRAX in osteoporosis. Osteoporos Int. 2010;21 Suppl 2:S407-13. [PMID: 20464374] 28. Nayak S, Roberts MS, Greenspan SL. Cost-effectiveness of different screening strategies for osteoporosis in postmenopausal women. Ann Intern Med. 2011; 155:751-61. [PMID: 22147714] 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 595 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 Annals of Internal Medicine Current Author Addresses: Drs. Pickhardt and Pooler, Mr. Lauder, and Drs. Muñoz del Rio and Bruce: Department of Radiology, University of Wisconsin School of Medicine and Public Health, E3/311 Clinical Science Center, 600 Highland Avenue, Madison, WI 53792-3252. Dr. Binkley: Divisions of Geriatrics and Endocrinology, University of Wisconsin School of Medicine and Public Health, 2870 University Avenue, Suite 100, Madison, WI 53705. Author Contributions: Conception and design: P.J. Pickhardt, B.D. Pooler, R.J. Bruce, N. Winkler. Analysis and interpretation of the data: P.J. Pickhardt, B.D. Pooler, A. Muñoz del Rio, R.J. Bruce, N. Winkler. Drafting of the article: P.J. Pickhardt, B.D. Pooler, A. Muñoz del Rio. Critical revision of the article for important intellectual content: P.J. Pickhardt, B.D. Pooler, A. Muñoz del Rio, R.J. Bruce, N. Winkler. Final approval of the article: P.J. Pickhardt, B.D. Pooler, A. Muñoz del Rio, R.J. Bruce, N. Winkler. Statistical expertise: B.D. Pooler, A. Muñoz del Rio. Obtaining of funding: P.J. Pickhardt. Administrative, technical, or logistic support: P.J. Pickhardt, R.J. Bruce. Collection and assembly of data: P.J. Pickhardt, B.D. Pooler, T. Lauder, R.J. Bruce. Appendix Table 3. DXA T-Score Categorization According to Vertebral or Hip Location* Appendix Table 1. Indications for Abdominal CT Scans Indication CT Scans, n Suspected focal abnormality/mass or oncologic surveillance Genitourinary signs* Gastrointestinal signs† Nonspecific symptoms‡ Vascular signs§ Suspected infection, inflammation, or abscess Other or unspecified Total 414 402 398 374 181 154 140 2063 CT = computed tomography. * For example, urolithiasis, hematuria, renal evaluation, and adrenal lesion. † For example, virtual colonoscopy, bowel obstruction, and diverticulitis. ‡ For example, abdominal pain, fever, weight loss, and trauma. § For example, abdominal aortic aneurysm and suspected bleeding or ischemia. Vertebral DXA T-Score (n = 2063) Hip DXA T-Score (n = 2063) Normal Osteopenia Osteoporosis Not Reported Normal Osteopenia Osteoporosis Not reported 535 (4) 131 (1) 4 (0) 81 (4) 302 (11) 408 (22) 116 (7) 173 (19) 23 (4) 85 (6) 121 (23) 61 (13) 5 (0) 9 (1) 8 (4) 0 (0) DXA = dual-ener gy x-ray absorptiometry. * Numbers in parentheses indic ate that a moderate or severe vertebr al fracture is present. Appendix Figure 1. CT-attenuation data relative to DXA T-scores. Appendix Table 2. BMD Categorization in 2063 CT Scans 250 With DXA Correlation Osteoporosis Osteopenia Normal Not reported Patients With CT–DXA Pairs, n Hip DXA (Alone) Lumbar Spine DXA (Alone) Central DXA (Hip and Lumbar Spine)* Central DXA and Vertebral Fracture† 249 586 913 315 290 948 803 22 418 978 667 0‡ 480 928 655 0‡ Mean CT Attenuation, HU BMD Category 230 210 190 170 150 130 110 90 70 CT = computed tomography; BMD = bone mineral density; DXA = dualenergy x-ray absorptiometry. * Determined by the lowest DXA T-score between the hip and lumbar spine. † The presence of a moderate or severe vertebral compression fracture results in osteoporotic categorization. This column represents the final reference standard used in this study. ‡ Cases without both hip and lumbar spine DXA T-scores were excluded from the study cohort. 50 T12 L1 L2 L3 L4 L5 Average Vertebral Level Osteoporosis Osteopenia Normal Mean trabecular CT-attenuation values (SDs) at each vertebral level, stratified by osteoporosis, osteopenia, and normal bone mineral density according to the DXA reference standard. The differences between mean attenuation for each bone mineral density group at each level are significant (P < 0.001). On average, CT attenuation tends to be lowest at the L3 level and increases slightly at higher and lower levels. CT = computed tomography; DXA = dual-energy x-ray absorptiometry. W-240 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 www.annals.org Appendix Table 4. Sample L1 CT-Attenuation Ranges for Normal, Intermediate, and Abnormal Values Relative to DXA T-Scores in 2040 CT–DXA Pairs* L1 CT-Attenuation Value† Normal Intermediate Abnormal Hip DXA T-Score Normal Osteopenia Osteoporosis 417 287 96 180 410 344 13 66 206 Not Reported 3 5 13 Lumbar Spine DXA T-Score Normal Intermediate Abnormal Normal 447 335 128 Osteopenia 98 277 208 Osteoporosis 7 56 180 Not Reported 61 100 143 Central (Combined) DXA T-Score‡ Normal Intermediate Abnormal Normal 366 197 56 Osteopenia 228 467 314 Osteoporosis 19 104 289 Not Reported 0 0 0 CT = computed tomography; DXA = dual-energy x-ray absorptiometry. * Sample ranges were obtaining by roughly divided the cohort into thirds, but other cutoff values can be used. 613 CT scans were classified as “normal,” 768 as “intermediate,” and 659 as “abnormal.” † Values >175 HU were categorized as “normal,” those between 130 and 175 HU were categorized as “intermediate,” and those <130 HU were categorized as “abnormal.” ‡ Only T-scores, not vertebral compression fractures, were considered. www.annals.org 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 W-241 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 Appendix Figure 2. PPV and NPV, according to L1 CT-attenuation threshold. 100 90 80 PPV 70 Percentage NPV 60 50 40 30 20 75 80 85 90 95 100 105 110 115 120 125 130 135 140 145 150 155 160 165 170 175 180 185 190 195 200 L1 CT-Attenuation Threshold, HU The graph shows the PPV for osteoporosis for L1 CT-attenuation values at or below each threshold; the NPV for excluding osteoporosis refers to L1 CT-attenuation values at or above each threshold. The relatively high NPV throughout is driven partly by the lower overall prevalence of osteoporosis (22.9%). CT = computed tomography; NPV = negative predictive value; PPV = positive predictive value. W-242 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 www.annals.org www.annals.org Vertebral Level T12 L1 L2 L3 L4 L5 T12–L5ave High (About 90%) Sensitivity High (About 90%) Specificity Balanced Sensitivity and Specificity CT-Attenuation Threshold, HU Sensitivity (TP/[TP + FN]), % (n/N) Specificity (TN/[TN + FP]), % (n/N) CT-Attenuation Threshold, HU Sensitivity (TP/[TP + FN]), % (n/N) Specificity (TN/[TN + FP]), % (n/N) CT-Attenuation Threshold, HU Sensitivity (TP/[TP + FN]), % (n/N) Specificity (TN/[TN + FP]), % (n/N) 165 160 155 150 145 150 150 89.3 90.0 91.3 90.9 90.4 90.6 89.4 49.4 52.3 51.5 47.1 55.6 56.0 56.7 115 110 110 100 100 105 110 51.3 52.1 54.4 50.9 48.7 50.4 55.7 90.1 91.3 89.0 88.5 88.6 89.4 89.6 140 135 130 125 125 130 130 75.2 75.5 72.4 75.7 75.6 73.3 74.7 74.0 75.4 75.4 72.3 72.8 74.1 75.8 (407/456) (415/461) (430/471) (427/470) (423/468) (404/446) (428/479) (770/1560) (826/1579) (812/1577) (743/1576) (863/1553) (839/1497) (897/1583) (234/456) (240/461) (256/471) (239/470) (228/468) (225/446) (267/479) (1406/1560) (1441/1579) (1403/1577 (1394/1576) (1376/1553) (1339/1497) (1418/1583) (343/456) (348/461) (341/471) (356/470) (354/468) (327/446) (358/479) (1155/1560) (1190/1579) (1189/1577) (1139/1576) (1130/1553) (1110/1497) (1200/1583) CT = computed tomography; FN = false-negative; FP = false-positive; T12–L5ave = mean of the T12 to L5 values; TN = true-negative; TP = true-positive. * “Nonosteoporosis” is defined as having osteopenia or normal bone mineral density. 1.0 0.8 0.6 0.4 0.2 0.0 0.0 0.2 0.6 1 – Specificity 0.4 0.8 T12 (AUC, 0.82 [95% CI, 0.80–0.84]) L1 (AUC, 0.83 [95% CI, 0.81–0.85]) L2 (AUC, 0.83 [95% CI, 0.8–0.85]) L3 (AUC, 0.81 [95% CI, 0.79–0.84]) L4 (AUC, 0.82 [95% CI, 0.79–0.84]) L5 (AUC, 0.82 [95% CI, 0.8–0.85]) Average (AUC, 0.84 [95% CI, 0.82–0.86]) 1.0 Appendix Figure 3. Receiver-operating characteristic curves for predicting osteoporosis by using CT values (region of interest method). Sensitivity Multivariate model (AUC, 0.83 [95% CI, 0.81–0.86]) The AUCs are similar at each individual vertebral level, using a multilevel T12 to L5 average, and in a multivariable model incorporating measures from all levels simultaneously, with broad overlap of 95% CIs. Osteopenia was considered a false-positive result for these calculations. The total number of assessable CT measurements per level was 2016 for T12, 2040 for L1, 2048 for L2, 2046 for L3, 2021 for L4, and 1943 for L5. AUC = area under the receiver-operating characteristic curve; CT = computed tomography. 16 April 2013 Annals of Internal Medicine Volume 158 • Number 8 W-243 Downloaded From: http://annals.org/ by a Chongqing University of Medical Sciences User on 04/21/2013 Appendix Table 5. Diagnostic Performance of Sample Vertebral CT-Attenuation Thresholds at Abdominal CT for Distinguishing Osteoporosis From Nonosteoporosis*