CURRICULUM VITAE - Consultant Medical
advertisement
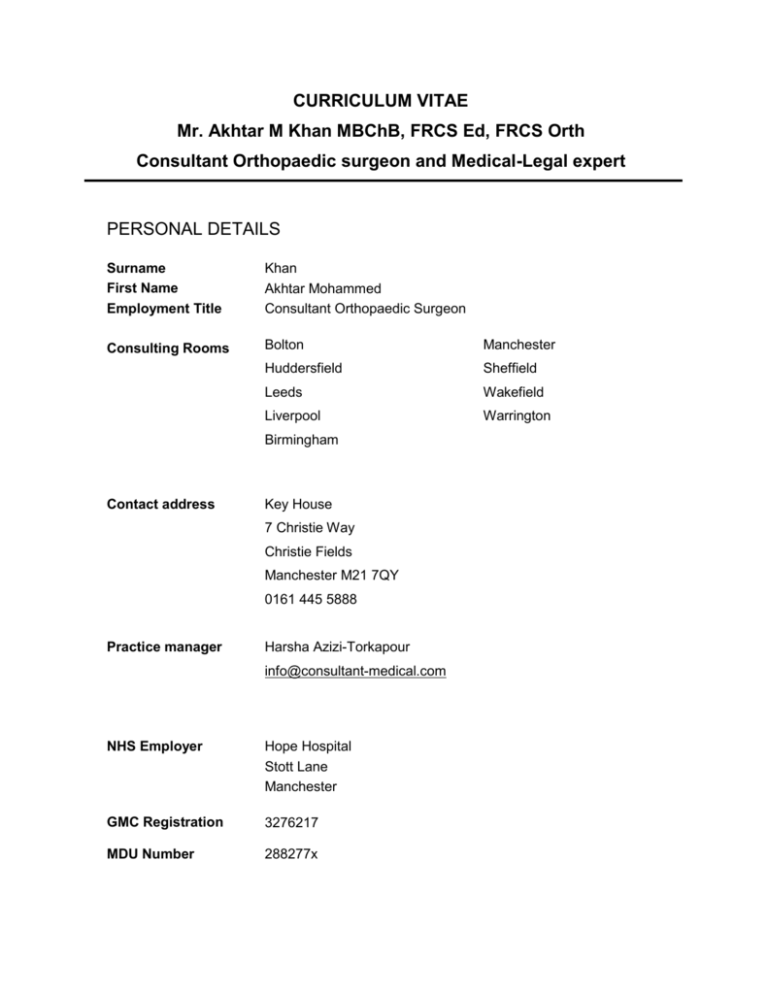
CURRICULUM VITAE Mr. Akhtar M Khan MBChB, FRCS Ed, FRCS Orth Consultant Orthopaedic surgeon and Medical-Legal expert PERSONAL DETAILS Surname First Name Employment Title Khan Akhtar Mohammed Consultant Orthopaedic Surgeon Consulting Rooms Bolton Manchester Huddersfield Sheffield Leeds Wakefield Liverpool Warrington Birmingham Contact address Key House 7 Christie Way Christie Fields Manchester M21 7QY 0161 445 5888 Practice manager Harsha Azizi-Torkapour info@consultant-medical.com NHS Employer Hope Hospital Stott Lane Manchester GMC Registration 3276217 MDU Number 288277x PROFESSIONAL QUALIFICATIONS 1991 1995 2001 2006 MBChB FRCS. Edinburgh FRCS. Trauma & Orth Diploma in Medical-legal report writing PERSONAL INJURY EXPERIENCE Preparing medical reports since 2001. Over 750 reports annually 50% claimant work and 20% defendant work ratio and 30% joint instructions. Court Experience AREAS OF EXPERTISE Low velocity accidents – guest speaker at medical legal conferences RTA and Cervical acceleration/deceleration trauma Pelvic trauma Fracture management- short term, mid term and long term outcomes SERVICE LEVEL OF AGREEMENT Appointment 4-6 weeks of instruction Report return 7 working days. (24 hours in case limitation) Home visits Yes Office structure 5 full time members of staff. Office hours 9.00-16.00 CLINICAL NEGLIGENCE 35-40 Clinical negligence reports/annum Negligence in Trauma management and patient care pathways Lower limb arthroplasty issues Metal on Metal issues MEDICAL-LEGAL LECTURES & EDUCATION o Lecturer at Medical–legal conferences since 2004/5 o Low velocity RTA and review of literature o Waddell’s signs- the misconception in their use to determine malingering o Biomechanics of acceleration/ deceleration injuries (Whiplash) o Fracture outcome. Short term, medium term and long term issues o In House training for paralegals. Half day training program o Monthly Newsletters on PI issues to >500 solicitors MEDICAL-LEGAL EXPERTS FORUM LinkedIn forum >700 members in 4 months from conception in July 2012 Weekly review and update of medical literature and outcomes. Promoting discussion between medical experts and solicitors RESEARCH 16 Papers in peer reviewed Journals 15 Internet publications 32 Podium presentations at national or international meetings 19 Poster presentations national or international meetings 3 Prizes for best presentations 5 Research Grants CURRENT APPOINTMENT & HIGHER SURGICAL TRAINING August 2005-present. Senior Consultant Orthopaedic Surgeon. Salford Royal Teaching Hospital. Manchester. Senior Lower limb Arthroplasty and reconstruction Surgeon. Specialising in complex primary and revision arthroplasty surgery. Trauma interest has evolved around pelvic and complex lower limb injuries. August 2003 Consultant Orthopaedic Surgeon. Pelvic trauma and Lower Limb Arthroplasty North Manchester General Hospital Feb. 2003-July 2003 Consultant Orthopaedic Surgeon. Pelvic trauma and Lower Limb Arthroplasty North Manchester General Hospital January 2003 Lower Limb Arthroplasty Fellowship and pelvic trauma North Manchester General Hospital, Manchester Mr A D Clayson Mr D H Sochart Foot & Ankle Arthroplasty Fellowship Wrightington Hospital Mr P R L Wood July 2002- Dec 2002 Lower Limb Arthroplasty Fellowship. Royal Orthopaedic Hospital, Birmingham Mr M McMinn Mr R B C Treacy Mr A M C Thomas Mr D Dunlop Aug.2001-July 2002 Year 5 SpR Northwest Health Region. Hope Hospital, Manchester Lower Limb Arthroplasty, Foot & Ankle, Non-union reconstruction Mr H A Maxwell Mr R A Wilkes Aug. 2000- Aug.2001 Year 4 SpR Northwest Health Region. Hope Hospital, Royal Manchester Children’s Hospital. Manchester Lower limb arthroplasty, Trauma, Paediatric Orthopaedic surgery Mr J G Andrews, Mr A Henry, Professor C S B Galasko Aug.99- Aug.2000 North West Health Authority Research and Development Fellow North Manchester General Hospital, University of Manchester Aug. 98-Aug. 99 Harry-Platt Fellow. Hope Hospital & North Manchester General Hospital, University of Manchester Aug. 97- Aug. 98 Clinical Tutor Orthopaedic Surgery North Manchester General Hospital, Manchester Lower Limb Arthroplasty, Paediatric Orthopaedic Surgery, Trauma Mr P R Kay Mr T H Meadows Mr A D Clayson Aug. 96- Aug.97 Clinical Tutor Orthopaedic Surgery. Wythenshaw Hospital, Manchester Upper & Lower Limb Arthroplasty, Paediatric Orthopaedic Surgery Mr C Warren-Smith Mr T H Meadows RESEARCH FUNDING Harry Platt Fellowship £34,450 Northwest Research and Development Fellowship £37,450 British orthopaedic Association Wishbone Trust £25,000 North Manchester R&D Unit £15,000 AWARDS/PRIZES Naughton Dunn Prize -Best Podium Presentation. Differentiating hip pain from back pain based on pain distribution Naughton Dunn Meeting. Birmingham 2002 McKee Prize. Best Podium Presentation. Blood transfusion following joint replacement: immune modulation and infection British Hip society. Keswick 2002. Best Poster Presentation. Preoperative concerns of patients awaiting hip and knee arthroplasty British Hip society. Keswick 2002 Second best Poster. Significance of post-operative pyrexia to the outcome of hip arthroplasty British Hip Society. Keswick 2002 PUBLICATIONS Secondary resurfacing of the patella for anterior knee pain following primary knee arthoplasty H E Muoneke A M Khan K Giannakas E Hagglund T Dunningham Journal of Bone and Joint Surgery vol.85-B, No 5 July 2003 Abstract Out of a total of 623 patients who, over a ten-year period, underwent primary total knee replacement (TKR) without patellar resurfacing, 20 underwent secondary resurfacing for chronic anterior knee pain. They were evaluated pre- and postoperatively using the clinical and radiological American Knee Society score. The mean follow-up was 36.1 months (12 to 104). The mean knee score improved from 46.7 to 62.2 points and the mean functional score from 44.7 to 52.2 points. Only 44.4% of the patients, however, reported some improvement; the remainder reported no change or deterioration. The radiographic alignment of the TKR did not influence the outcome of secondary resurfacing of the patella. Complications were noted in six of the 20 patients including fracture and instability of the patella and loss of movement. Anterior knee pain after TKR remains difficult to manage. Secondary resurfacing of the patella is not advocated in all patients since it may increase patient dissatisfaction and hasten revision. Cross-sectional anatomy of the post-distraction osteogenesis tibia. Long term study in adults K Giannakas, A M Khan, R A Wilkes Orthopaedic Proceedings. Supplement of the Journal of Bone and Joint Surgery Abstract While the early period of distraction osteogenesis has been extensively investigated, there are very few data describing the long-term morphology of the regenerate. We performed magnetic resonance scans in ten adults (men age 35+− 11 yr), seven of whom had bone transport for an iatrogenic osseous defect while further three had tibial lengthening for limb length discrepancy. Follow-up ranged between 14 and 43 months (mean : 28 + − 10 months) following the removal of the external fixator. The perimeter, cross- sectional area, volume and the mean signal intensity was calculated from the obtained T1 weighted axial images. Values were compared with the contralateral tibia that acted as control. All cases that had bone transport increased the volume of the tibia from 15.3% up to 50.8%. The regenerated segment was noted to have expanded significantly (p<0.0001) in all cases. Mean signal intensity in the regenerate decreased in seven cases significantly (p<0.0001) suggesting increase content of unhydrated tissue such as bone and collagen. The cross-sectional surface of the transported segment was increased in all cases (p<0.008). Finally in cases that underwent bone transport, the docking site was noted to be obstructed by unhydrated tissue. Contrary to previous claims, the post-distraction osteogenesis tibia is far from normal, consisting of areas with potentially different biomechanical properties. Recognition of these changes is essential not only for appropriate pre-operative counseling but also for considering treatment modalities in case of a fracture. Evaluation of patient concerns prior to hip and knee replacement surgery. Moran M, Khan A, Sochart DH, Andrew G. Journal of Arthroplasty 18(4): 442-5. 2003 Abstract The preoperative concerns of patients undergoing total knee or hip arthroplasty were evaluated in a cross-sectional study of 370 patients. Patients completed a questionnaire on 29 concerns, each rated on a scale of 1 (not concerned) to 4 (very concerned). Short Form 12 and Oxford hip or knee scores were also calculated. The results showed that the greatest concern for patients was cancellation of the surgery. This was followed by failure of the surgery to reduce pain, loss of a limb, and joint infection. Concerns regarding scar problems, nursing care, and preoperative tests were the lowest. Women showed statistically significant greater concerns in 9 areas. Younger patients (age, <65) showed increased concerns in 8 areas. Patients who had previously undergone joint arthroplasty were less concerned than those who had not undergone previous lower limb joint arthroplasty for 6 responses. They showed increased concern in 2 areas, nursing care and hospital food. Those undergoing total hip arthroplasty were more concerned about dislocation, dressing, and returning to work (all, P<.05). This study provides useful information for the preoperative counseling of patients and the production of preoperative literature. Expect the best prepare for the worst. Surgeon and patient expectation of the outcome of primary total hip and knee replacement M Moran A M Khan J G Andrews D H Sochart Annals Royal Coll Surg England 85(3); 204-6. 2003 Abstract A cross-sectional study of 100 surgeons and 370 patients awaiting primary total hip or knee replacement was carried out. Oxford hip or knee score questionnaires were sent to the surgeons and patients. They were asked to predict the level of symptoms expected 6 months following surgery. The Oxford scores derive a value of 12-60, with a greater score indicating worsening symptoms. The mean pre-operative score was 45.12 for the hip patients and 42.96 for the knee patients, and the patients expected this to drop to 23.70 and 25.66, respectively, 6 months' postoperatively. This was a significant difference for both groups. The surgeons expected the patients to have a mean postoperative score of 20.91 for the hip group and 22.19 for the knee group. The surgeons' scores were significantly lower than those from the patients. There was a significant difference between the patients' and surgeons' expectations of the results of total knee and hip replacement surgery. The surgeons expected better results than the patients. We believe that this is the first study that directly compares surgeon and patient expectations of lower limb arthroplasty. Post-operative pyrexia and primary total hip replacement. A M Khan J G Andrews P R Kay. Orthopaedic Proceedings. Supplement of the Journal of Bone and Joint Surgery Abstract Pyrexia in the post-operative setting has often been associated with a possible systemic or wound infection. We assessed whether there is any justification for our concern regarding post-operative pyrexia following hip arthroplasty and subsequent deep prosthetic infection. An assessment of the clinical outcome of 97 sequential patients who underwent 103 primary hip arthroplasty for primary osteoarthritis replacements. Daily temperature and systemic complications in the post-operative period were recorded. Clinical outcome was measured using an Oxford hip questionnaire. Patients had a mean follow-up of 5.2 years (range 3.5–7.2years) We reviewed the postoperative temperature records of 80 patients who had undergone primary total hip replacement. Thirty-one patients had required revision surgery at a mean time interval of 37.2 months (range 5–74 months) for confirmed deep prosthetic infection. The remaining Forty-nine patients were asymptomatic at a mean follow-up of 31.5 months. Study 1: Post-operative pyrexia of 38 degrees Celsius was present in 51% of patients undergoing primary hip replacement in the first post-operative week but in 21.1% no etiological cause could be identified. Clinical outcome measured by an Oxford hip questionnaire was not influenced by the post-operative temperature pattern. Study 2 : The mean peak temperature on the first post-operative day was significantly lower in patients with deep prosthetic infection then patients with a clinically normal outcome (p=0.01). Post-operative pyrexia is clearly not uncommon following primary arthroplasty and its presence should not be regarded as detrimental. Pyrexia in the postoperative setting is a component of the acute phase response to trauma and study 2 demonstrates patients who develop a low-grade infection following arthroplasty may have a diminished febrile response to surgical trauma which may be an indirect representation of a diminished immune response to surgical trauma or infection Post-operative infection following hip arthroplasty. use of serological parameters for diagnostic assistance Orthopaedic Proceedings. Supplement of the Journal of Bone and Joint Surgery Abstract The metabolic response of trauma may mimic infection and the reliability of serological parameters for diagnosing infection may be questionable. We prospectively assessed the changes in the acute inflammatory markers, febrile response and the immune profiles cytokine activation and collagen markers of 101 patients following primary hip arthroplasty and their association with infection. Method: The clinical outcome of 101 patients was monitored. Serological analysis was performed pre-operatively and on the second and 8th post-operative day as well as in an out patient clinic 6 weeks following surgery. The serological markers included total white blood cell count along with T and B lymphocyte function. Levels of CD4, CD8 and CD56 were analysed for T helper, T Cytotoxic cell and Natural Killer cell activity. Inflammatory makers included plasma viscosity and CRP. Cytokine assays included IL-1, IL-6, IL-10 and TNF. Collagen markers included P1CP and P1NP as markers of Type I and Type III collagen synthesis. Serological titers of Staph. Aureus and Staph. Epidermis were performed pre-operatively and on day 8 and week 6 following surgery. Results: Post-operative complications included 19 UTI, 11 chest infections and three URTI and six a confirmed deep vein thrombosis. Wound complications included 10 patients with wound erythema and 4 patients had pus discharge. 20 patients had elevated ASO titers and 19 patients had raised Staph. Epidermis titers. Statistical comparison of WBC, Plasma viscosity, temperature profiles and T helper, T cytotoxic cell and NK cell assays is not different between patients with and without systemic infection or raised titres of Staph. Aureus or Staph. Epidermis. Collagen markers were significantly higher in wound complications. Conclusion: The acute phase responses following surgery and metabolic response to trauma obscures the changes seen in infective complications up to six weeks postoperatively. The use of serological parameters that are components of the acute phase response of surgery does not allow differentiation of infection from normal physiological changes. Blood transfusion following primary hip arthroplasty: immune modulation and infection Orthopaedic Proceedings. Supplement of the Journal of Bone and Joint Surgery Abstract Blood transfusion is associated with an increased incidence of post-operative nosocomial infections following surgery. In a prospective study we evaluated the association of blood transfusion and the changes in the immune status with the incidence of infection in the post-operative period following primary hip arthroplasty and subsequently for two years following surgery Method: Prospective analysis of 100 patients undergoing primary total hip replacement. 25 patients received predonated autologus blood transfusions, 26 received SAGM whole blood, 23 received leukocyte depleted blood and 26 did not require a transfusion. T-helper cell, cytotoxic T cell and NK cell activity was recorded using a Beckton Dickson flow cytometer and assays of Plasma viscosity, CRP, Staph. Epidermis and ASO titres were analysed. All infections were recorded for 2 years following surgery. Results: he incidence of confirmed or suspected nosocomial infections following hip replacement was the same in non transfused patients as those receiving predonated autologus blood (19%). The incidence of nosocomial infection in patients receiving leukocyte depleted blood was 32% and 42% in those receiving a SAGM blood transfusion. ASO titres were raised in 16.9% of the patients on day 8 following surgery and Staph. Epidermis assays were raised in 20.2% of the patients however the frequency was unrelated to the type of blood transfusion. The incidence of nosocomial infections was reflected by a greater reduction in NK activity and CD4: CD8 ratio following surgery in patients receiving SAGM blood transfusion. Conclusion: Homologus blood transfusion may produce an immune compromise in patients, which is still detectable at 6 weeks following surgery. This is clinically reflected by a higher incidence of systemic infections in the postoperative period. Homologus blood should be used judiciously in joint arthroplasty with a preference to either leukocyte depleted blood or predonated autologus blood. Treatment of recurrent dislocation of total hip arthroplasty using a ligament prosthesis K Barbosa A M Khan J G Andrews Journal of Arthroplasty April 2004, Pages 318–321 Abstract Recurrent dislocation of total hip arthroplasty (THA) has a poor prognosis when the cause of dislocation cannot be ascertained. We present the successful use of a synthetic ligament prosthesis to treat 4 patients with recurrent posterior dislocation of THA. After an average follow-up period of 28 months, none of the patients had any further episode of dislocation. We believe that this is a simple and low-risk method of treating selected patients and avoids the poor outcome associated with surgery to revise components. Hip Osteoarthritis. Where is the pain? A M Khan E Mcloughlin K Giannakas C E Hutchinson J G Andrews. Annals of the Royal College of Surgeons 2004 March; 86(2): 119–121. Abstract Pain radiating below the knee is typically thought to originate from the lumbosacral spine rather than degenerative hip pathology. We investigated the lower limb distribution of pain using body image maps in 60 patients awaiting primary hip arthroplasty and in 60 patients awaiting spinal decompression for confirmed spinal stenosis. The perception of 33 orthopedic registrars regarding distribution of hip pain was also assessed. RESULTS: Groin and buttock pain are significantly more common in hip osteoarthritis. The presence of groin pain is 84.3% of those sensitive for hip dysfunction with a specificity of 70.3%. Patients with hip osteoarthritis had pain below the knee in 47% of cases whereas 88.5% of orthopaedic trainees believed hip pain did not radiate below the knee. Radiographic features of osteoarthritis within the hip joint, visual analogue pain score or Oxford Hip Score have no significant association with a patient's distribution of hip pain. CONCLUSIONS: Hip pain referred below the knee is common with a degenerate hip joint and follows the distribution of the saphenous nerve, which branches from the femoral nerve. Radiographic deterioration of a hip joint does not correlate with pain distribution or patient dysfunction as measured by the Oxford Hip Score. Cross match protocols for femoral neck fractures. Finding one that works. A M Khan. N Mushtaq D H Sochart J G Andrews. Annals of the Royal College of Surgeons 2004 January; 86(1): 11–14. Abstract Cross-match practice for patients with femoral neck fractures continues to cause concern due to a failure of compliance to the existing protocols. To address this issue, a number of studies were conducted over a 3-year period. METHODS: First, the existing crossmatch practice for patients admitted with femoral neck fractures was reviewed to demonstrate the deficiencies within the system. Second, the opinion of anaesthetic and orthopaedic trainees was assessed regarding blood requirements for different femoral neck fractures following surgery and the justification of their perceptions. RESULTS: A summation of the studies is reported which demonstrates the reasons for the poor compliance to previous protocols. CONCLUSIONS: A simple and effective protocol is provided that has helped reduce pre-operative cross-matching of femoral neck fractures from 71% to 16.7% when assessed 2 years after its introduction. Bladder catheterisation in joint arthroplasty. Pre-opertive identification of patients Orthopaedic Proceedings. Supplement of the Journal of Bone and Joint Surgery Abstract Bladder catheterisation following joint arthroplasty is not uncommon but delaying catheterisation in the postoperative period until the patient is symptomatic can produce an atonic bladder due to the distension. This can prolong catheterisation and increase the risk of urinary tract infection. We prospectively determined if we could identify patients needing pre-operative catheterisation. Method: 150 consecutive patients undergoing knee and hip arthroplasty were recruited. Pre-operative symptoms of frequency, nocturia, retention, incontinence and previous bladder or prostate surgery along with prior history of catheterisation were recorded. The type of anaesthesia and post-operative analgesia was noted. Details of catheterisation included duration, antibiotic administration, and reason for catheterisation and incidence of urinary tract infection. Results: Patients mean age was 67.7 years. 47 patients required catheterisation of which 56.6% were female. The mean age of patients catheterised was 70.6 years in comparison to 66.3 years (Mann-Whitney P<0.01). The frequency of catheterisation was unrelated to the surgical procedure. Nocturia was significantly more common in-patients requiring catheterisation (Kruskal Wallis P=0.04) and its combination with pre-operative symptoms of frequency, retention or incontinence increased the significance further to P=0.001. Patient age of greater then 66 years had a 76.6% predictive value for the subsequent need of catheterisation. This further increased to 91.5% when combined with a previous history of either catheterisation or nocturia. The type of anaesthesia or the post-operative analgesia did not significantly influence catheterisation frequency. Conclusion: Patients aged greater then 66 years undergoing joint arthroplasty with previous history of catheterisation or nocturia may benefit from pre-operative bladder catheterisation. Peri-operative catheterisation of high-risk patients in theatre reduces patient discomfort caused by the observation period and avoids bladder atonia consequent of the distention, which may subsequently prolong catheterisation. Ganglion of the flexor hallucis longus tendon as a cause of posterior ankle pain extending to the Hallux. R Hillier K Giannakas A M Khan. Foot. Pages 119-121, June 2003 Abstract We describe a case of a ganglion of the flexor hallucis longus tendon in a young man with chronic foot pain, and suggest that such ganglia be considered as part of the differential diagnosis for posterior ankle pain. Sacroiliac joint fusion for chronic pain: a simple technique avoiding the use of metalwork A M Khan K Giannikas H A Maxwell European Journal of Spine 2004 May;13(3):253-6. Epub 2003 Nov 28. Abstract A previously undescribed method for posterior fusion of the sacroiliac joint (SIJ) utilizing the Cloward instrumentation is presented, suitable for cases with chronic pain and intact ligamental structures of the SIJ. The advantages of the method in comparison with other described options include minimal disturbance of the periarticular structures, avoidance of introduction of metalwork and preservation of the iliac crest contour. This technique has been used in five cases with follow-up longer than 2 years (mean 29 months, range 25-41 months). In all cases there was resolution of their painful symptomatology. Use of intramedullary reaming as a therapeutic procedure in treatment of diaphyseal osteomyelitis of intact long bones Orthopaedic Update 2001 vol:10 no. 2 page 46-8 Lacerations of the extensor hallucis longus tendon Orthopaedic update Vol.11. No.2 August 2001 Non-union of colles fractures. Orthopaedic update Vol. 11.No 1 April 2001 Tension band fixation of greater tuberosity fractures following anterior dislocation of the shoulder joint. Orthopaedic Update. Vol 6. No. 1. Dec 96 Spontaneous perforation of the second part of the duodenum in a child. Postgraduate Medical Journal. Sep 96 vol. 72: 575 No. 851 Cerebrotendinous Xanthomatosis: A rare cause of tendon xanthomas. A M Khan A Paul M Amr. Orthopaedic Update. Vol: 5. No. 1 Dec. 95 PRESENTATIONS Secondary resurfacing of the patella for anterior knee pain following primary knee arthroplasty A M Khan, R Goyal, H E Moneke, K A Giannikas, E Hagglund, T Dunningham 1. European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 2. North West Orthopaedic Trainees Association Annual meeting Nov. 2002 3. Naughton Dunn Meeting. Birmingham 2002 Cross-sectional anatomy of the post-distraction osteogenesis tibia. Long term study in adults A M Khan, R A Wilkes, M T Karski, K A Giannikas, A M Buckle, S Hutchinson 1. European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 2. British Orthopaedic Association 2003 Bladder catheterisation in joint arthroplasty. A M Khan, K Ho, D H Sochart J G Andrews British Orthopaedic Association. 2003 Arthrodesis of the first metatarsophalangeal joint using tricortical grafts as salvage for failed Kellers excisional arthroplasty. A M Khan, M Karski, K Giannikas, H A Maxwell British Orthopaedic Association. 2003 Serological parameters in the detection of postoperative infection following hip arthroplasty A M Khan, Professor I Hutchinson, P R Kay 1. European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 2. Naughton Dunn Meeting. Birmingham 2002 The cost efficiency of autologous blood transfusion in primary knee arthroplasty A M Khan, K Ho, D H Sochart European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Cross-sectional anatomy of the post-distraction osteogenesis tibia. Long term study in adults A M Khan, R A Wilkes, M T Karski, K A Giannikas, A M Buckle, S Hutchinson 1. European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 2. British Orthopaedic Association. 2003 The paradox of post-operative pyrexia and deep infection following hip arthroplasty A M Khan, B M Wroblewski, P R kay European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Blood transfusion following joint replacement: immune modulation and infection A M Khan, Professor I Hutchinson, P R Kay 1. International Charnley Era Arthroplasty symposium. Manchester 2002 2. British Hip Society. Keswick 2002 Awarded best podium presentation The short term outcome of the OPERA cup A M Khan, K Ho, J P Hodgkinson, D H Sochart North West Orthopaedic Trainees Association Annual meeting. Nov. 2002 Cross match protocols for femoral neck fractures-finding one that works A M Khan, Z Siddique, K Giannikas, D H Sochart, J G Andrews 1. British Orthopaedic Association. Cardiff 2002 2. Naughton Dunn Meeting. Birmingham 2002 Preoperative concerns of patients awaiting hip and knee arthroplasty A M Khan, M Moran, J G Andrews, D H Sochart 1. British Orthopaedic Association. Cardiff 2002 2. North West Orthopaedic Trainees Association Annual meeting. Bolton 2001 Morton’s Neuroma: MR Scanning and corticosteroid injections for diagnostic assistance A M Khan, V George, K A Giannikas, H A Maxwell Naughton Dunn Meeting. Birmingham 2002 Differentiating hip pain from back pain based on pain distribution A M Khan, E Mcloughlin, A Quereshi, K Giannikas, J G Andrews Naughton Dunn Meeting. Birmingham 2002 Awarded best podium presentation The Orthopaedic management of the Rheumatoid Hip and Knee A M Khan Birmingham National Rheumatoid society. Birmingham 2002 Significance of post-operative pyrexia to the outcome of hip arthroplasty A M Khan, B M Wroblewski P R Kay British Orthopaedic Association. Cardiff 2002 Autologus versus homologus blood transfusion in primary total hip replacement: A change in immune status. A M Khan Professor I Hutchinson P R Kay International Charnley Era Arthroplasty symposium. Writingtington Hospital. 2000 Post-operative pyrexia in hip arthroplasty. A M Khan, P R Kay, J G Andrews North West Orthopaedic Trainees Association Annual meeting. Bolton 2000 Current guidelines for crossmatching and transfusion in orthopaedic surgery. A M Khan Current concepts course. Manchester October 2000 Do you really need that much blood? A M Khan, P R Kay British Trauma Society. Norwich Sep 2000. How much do you cross-match for femoral neck fractures? A difference in opinion between anaesthetists and orthopaedic trainees. A M Khan, J G Andrews Current concepts Manchester 1999 Diagnosis and management of colorectal submucosal lipomas A M Khan Gastrointestinal meeting. Manchester 1995 POSTER PRESENTATIONS Blood transfusion following joint replacement: immune modulation and infection. A M Khan, Professor I Hutchinson, P R Kay 1. European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 2. American Academy of Orthopaedic Surgeons 69th Annual meeting. Dallas. Feb 2002 3. British Orthopaedic Association. Cardiff 2002 Differentiating hip pain from back pain based on pain distribution A M Khan, E Mcloughlin, A Quereshi, K Giannikas, J G Andrews European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 The cost efficiency of autologous blood transfusion in primary knee arthroplasty A M Khan, K Ho, D H Sochart British Association for Surgery of the Knee. London 2003 Bladder catheterisation in joint arthroplasty. When should it be done? A M Khan, K Ho, D H Sochart 1. European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 2. British Hip Society. Belfast 2003 MR scanning for diagnosing Morton's neuroma A M Khan, K Giannikas, V George, S Hutchinson, H A Maxwell European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Recurrent dislocation of total hip replacement. Stabilisation with ligament prosthesis A M Khan, K Barbosa, J G Andrews European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Medium term results of the LCO hip A M Khan, K Giannikas, H E Muneke, E Hagglund, T Dunningham European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Sacroiliac joint fusion. A simple technique avoiding use of metalwork A M Khan, K Giannikas, H A Maxwell European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Arthrodesis of the first metatarsophalangeal joint using tricortical grafts as salvage for failed Kellers excisional arthroplasty. A M Khan, M Karski, K Giannikas, H A Maxwell European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 The short term outcome of the OPERA cup A M Khan, K Ho, D H Sochart European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Subtalar joint fusion- a new technique A M Khan, D Powers, A M C Thomas European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Significance of post-operative pyrexia to the outcome of hip arthroplasty A M Khan, J G Andrews, D H Sochart European Federation of National Associations of Orthopaedics &Traumatology. Finland 2003 Preoperative concerns of patients awaiting hip and knee arthroplasty A M Khan, M Moran, J G Andrews, D H Sochart British Hip Society. Keswick 2002 Awarded best poster presentation The paradox of post-operative pyrexia and deep infection following primary hip arthroplasty A M Khan, B M Wroblewski P R Kay British hip society. Keswick Feb 2002 Awarded second best poster presentation Use of intramedullary reaming as a therapeutic procedure in treatment of diaphyseal osteomyelitis of intact long bones. A M Khan, S Rao, P R Kay British Orthopaedic Association. Llandudno April 1996