Minimal-Incision Total Hip Arthroplasty
advertisement

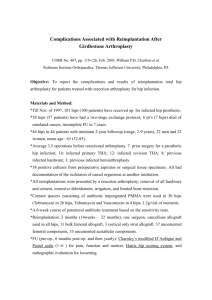
THE JOURNAL OF BONE & JOINT SURGERY VOLUME 85-A · SUPPLEMENT4 · 2003 Minimal-Incision Total Hip Arthroplasty BY WAYNE M. GOLDSTEIN, MD, JILL J. BRANSON, RN, BSN, KIMBERLY A. BERLAND, CST, FA, AND ALEXANDER C. GORDON, MD Objective: The purpose of this study is to present the experience with total hip arthroplasty performed through a minimal incision. Materials and Methods: Retrospectively of 170 total hip, 85 hips in 76 patients (the minimal-incision group), 85 hips in 78 patients (the standard-incision group). Preoperative Blood Product Protocol All patients scheduled for unilateral total hip arthroplasty donated one or two units of autologous blood. Individuals scheduled for bilateral total hip arthroplasty donated three units of autologous blood. Operative Technique For the standard-incision technique, a posterolateral approach to the hip was performed with use of a standard-length (12 to 24-in [30 to 61-cm]) curved incision. The minimal-incision technique is begun with an incision 2 cm posterior and 2 cm proximal to the apex of a standard incision, angled from the flare of the greater trochanter to the posterior superior iliac spine. Warfarin therapy for thromboembolic prophylaxis was started on the evening of the surgery, and a complete blood-cell count was done daily for the first three postoperative days. Data Collection: Demographic information, laboratory values, postoperative clinical course were determined, component type, estimated blood loss, length of the skin incision, operative time and the type and amount of blood products transfused. Clinical Evaluation: Physical examinations consisting of evaluation of the wound and measurement of the range of motion were performed at all visits. Statistical Analysis Unpaired t tests were used to compare continuous variables in normally distributed data between groups. The Pearson chi-square and Fisher exact tests were used to compare categorical data, such as transfusion status. Result: Patients Differences between groups with regard to weight and body-mass index (p = 0.0001) not to patient age or height (p = 0.30 and 0.16, respectively). Operative Data: There was a significant difference in the estimated blood loss at surgery between the standard-incision group (408 mL) and the minimal-incision group (273 mL) (p = 0.0001). Perioperative Blood Data No significant difference between groups with respect to preoperative hemoglobin level (p = 0.44). A significant difference between groups with regard to the absolute hemoglobin level on postoperative day one (98 g/L in the minimal-incision group and 102 g/L in the standard-incision group; p = 0.05). Categorical Data Sixty-five percent of the patients in the minimal-incision group and 56% in the standard-incision group required postoperative blood transfusions (p = 0.31, Fisher exact test). Eleven percent of the patients who had a transfusion in the minimal-incision group. 7% of such patients in the standard-incision group also required allogenic blood after infusion of the autologous units. Component Position The mean abduction angle of the cup was 47° (range, 38° to 56°). Two femoral components were in varus alignment; the rest were in neutral. Clinical Evaluation Patient satisfaction was high in both groups. no significant differences between the minimal-incision and standard-incision groups with regard to the Harris hip scores preoperatively. Complications There were seven wound complications, five in the standard-incision group and two in the minimal-incision group. All seven of these complications involved prolonged serous drainage. Six resolved with wound care and administration of oral antibiotics. The seventh, in a patient in the standard-incision group, required irrigation and débridement with a short period of intravenous antibiotics. Obese Patients Treated with Minimal-Incision Technique: Discussion: It is clear from those study data that the minimal-incision technique is not a minimally invasive operation. This is reflected by the fact that failed to find a difference between groups with regard to various postoperative parameters. The term minimally invasive must be used with caution, as a smaller skin incision does not necessarily mean less pain or faster rehabilitation.