Chapter 16: The child with altered respiratory status
advertisement
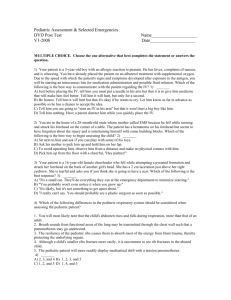
1 Bowden, Chapter 16: Supplemental Information Key Terms apnea atelectasis atopy cor pulmonale cyanosis dyspnea hemoptysis hypercarbia hypoxemia hypoxia pallor respiratory distress respiratory failure retractions subcutaneous emphysema tachypnea ventilation-perfusion mismatch 2 Summary of Key Concepts Certain anatomic and structural features of the respiratory tract in infants and young children predispose them to develop respiratory distress more readily than older children or adults. Respiratory illnesses and exacerbations of chronic respiratory conditions are the most common reasons for pediatric hospital admissions and ambulatory center visits, especially during winter and early spring. Viral and bacterial infections of the respiratory system are common and relatively unavoidable during childhood. Children with chronic conditions, especially conditions that involve the respiratory or cardiac systems, are at highest risk for serious morbidity or mortality associated with common childhood respiratory infections. Worsening respiratory distress can be identified by frequent and thorough respiratory assessments. Early recognition and prompt intervention for respiratory distress are key to prevent respiratory failure. Parents of children with chronic respiratory conditions must be educated to recognize signs and symptoms of respiratory compromise and to notify their healthcare provider immediately when they occur. Good decision making skills are an essential component of daily disease management. The nurse must teach these parents how to manage emergency situations in the home Children with chronic respiratory conditions require regular follow-up visits with healthcare providers and use of proactive and preventive measures. 3 Evidence-Based Practice Guidelines American Academy of Pediatrics. (2001). Clinical practice guideline: Management of sinusitis. Pediatrics, 108 (3), 798-808. American Academy of Pediatrics (AAP). (2003). Apnea, Sudden Infant Death Syndrome, and home monitoring. Pediatrics, 111, 914-917. American Association for Respiratory Care (AARC). (2007). Removal of the endotracheal tube—2007 revision & update. Respiratory Care, 52, 81-93. American Thoracic Society. (2007). An Official ATS Workshop Report: Issues in Screening for Asthma in Children. Available at http://www.thoracic.org/sections/publications/statements/ American Thoracic Society. (2007). An Official ATS/ERS Statement: Pulmonary Function Testing in Preschool Children. Available at http://www.thoracic.org/sections/publications/statements/ American Thoracic Society. (2000). Care of the child with a chronic tracheostomy. Available at http://www.thoracic.org/sections/publications/statements/ Cincinnati Children’s Hospital Medical Center. (2006). Evidence-based clinical practice guideline for medical management of bronchiolitis in infants less than 1 year of age presenting with a first time episode. Cincinnati, OH: Author. Available at www.guideline.gov. Kelley, L., & Allen, P. (2007). Managing acute cough in children: Evidenced –based guidelines. Pediatric Nursing, 33, 515-524. 4 Organizations Allergy & Asthma Network Mothers of Asthmatics www.breatherville.org American Academy of Allergy, Asthma and Immunology www.aaaai.org American Association for Respiratory Care (AARC) www.aarc.org American Cleft Palate-Craniofacial Association www.cleftline.org American College of Allergy, Asthma, and Immunology www.Acaai.org American Lung Association www.lungusa.org American Thoracic Society www.thoracic.org Association of Asthma Educators 5 www.asthmaeducators.org Asthma and Allergy Foundation of America (AAFA) www.aafa.org Centers of Disease Control and Prevention (CDC) www.cdc.gov Cystic Fibrosis Foundation www.cff.org Cystic Fibrosis Worldwide www.cfww.org Environmental Protection Agency, Office of Children’s Health Protection http//yosemite.epa.gov/ochp/ochpweb.nsf/homepage Food Allergy & Anaphylaxis Network www.foodallergy.org National Asthma Education and Prevention Program, NHLBI Information Center www.nhlbi.nih.gov/about/naepp/ 6 National Heart, Lung and Blood Institute Information Center www.nhlbi.nih.gov National Jewish Medical and Research Center www.njc.org Respiratory Nursing Society www.respiratorynursingsociety.org 7 Bibliography American Academy of Pediatrics (AAP). (2001). Clinical practice guidelines: Management of sinusitis. Pediatrics, 108, 798-808. American College of Obstetricians and Gynecologists (ACOG) (2001). Preconception and prenatal carrier screening for cystic fibrosis: Clinical and laboratory guidelines. Washington, DC: American College of Obstetricians and Gynecologists. Bennett, A.D. (2002). Home apnea monitoring for infants. Advance for Nurse Practitioners, 10, 47-54. Berge, J., & Patterson, J. (2004). Cystic fibrosis and the family: A review and critique of the literature. Families, Systems, & Health, 22, 74-100. Bjornson, C., & Johnson, D. (2005). Croup-Treatment update. Pediatric Emergency Care, 21(12), 863-873. Carpenter, D.R. & Narsavage, G.L. (2004). One breath at a time: Living with cystic fibrosis. Journal of Pediatric Nursing, 19, 25-32. Conway, S. (2004). Transition programs in cystic fibrosis centers. Pediatric Pulmonary, 37. 1-3. Cooper, K.E. (2001). The effectiveness of ribavirin in the treatment of RSV. Pediatric Nursing, 27, 95-98. Darrow, D., & Siemens, C. (2002). Indications for tonsillectomy and adenoidectomy. Laryngoscope, 112(8), 6-10. Donahue, M. (2002). “Spare the cough, spoil the airway:” Back to the basics in airway clearance. Pediatric Nursing, 28, 107-111. 8 Ebbinghaus, S. & Bahrainwala, A.H. (2003). Asthma management by an inpatient asthma care team. Pediatric Nursing, 29, 177-192. Flume, P.A., Taylor, L.A., Anderson, D.L., Gray, S. & Turner, D. (2004). Transition programs in cystic fibrosis centers: Perceptions of team members. Pediatric Pulmonary, 37, 1-3. Franzese, C.B. & Schweinfurth, J.M. (2002). Delayed diagnosis of a pediatric airway foreign body: Case report and review of the literature. Ear, Nose & Throat Journal, 81, 655-656. Grosse, S.D., Boyle, C.A., Botkin, J.R., et al (2004). Newborn screening for Cystic Fibrosis. Morbidity and Mortality Weekly Reports: Recommendations and Reports, 53, 1-36. Heijerman, H. (2005). Infection and inflammation in cystic fibrosis: A short review. Journal of Cystic Fibrosis, 4, 3-5. Horner, S.D., Surratt, D. & Smith, S.B. (2002). The impact of asthma risk factors on home management of childhood asthma. Journal of Pediatric Nursing, 17, 211-221. Johnson, C., Butler, S.M., Konstan, M.W. et al, (2003). Factors influencing outcomes in cystic fibrosis: A center based analysis. Chest, 123, 20-27. Kotagal, S. (2005). Childhood obstructive sleep apnoea (editorial). British Medical Journal, 330, 978-979. Korppi, M. (2003). Community-acquired pneumonia in children: Issues in optimizing antibacterial treatment. Pediatric Drugs, 5(12), 821-832. Lee, E., Parker, V., DuBose, L., Gwinn, J., & Logan, B. (2006). Demands and resources: Parents of school-age children with asthma. Journal of Pediatric Nursing, 21, 425-433. McCarthy, M.J., Herbert, R., Brimacombe, M., Hansen, J., Wong, D. & Zelman, 9 M. (2002). Empowering parents through asthma education. Pediatric Nursing, 28, 465-473. Meissner, H.C. & Rennels, M.B. (2004). Unpredictable patterns of viral respiratory disease in children. Pediatrics. 113, 1814-1816. Millman, R.P. & Working Group on Sleepiness in Adolescents/Young Adults; and AAP Committee on Adolescence (2005). Excessive sleepiness in adolescents and young adults: Causes, consequences, and treatment strategies. Pediatrics, 115, 1774-1786. Patterson, E.E., Brennan, M.P., Linskey, K.M., et al (2005). A cluster randomized intervention trial of asthma clubs to improve quality of life in primary school children: The School Care and Asthma Management Project (SCAMP). Archives of Diseases in Childhood, 90, 786-791. Pediatric Tuberculosis Collaborative Group (2004). Targeted Tuberculin skin testing and treatment of latent Tuberculosis infection in children and adolescents. Pediatrics, 114, 1175-1201. Peeke, K., Hershberger, M., & Marriner, J. (2006). Obstructive sleep apnea syndrome in children. Pediatric Nursing, 32, 489-494. Rotta, A.T. & Wiryawan, B. (2003). Respiratory emergencies in children. Respiratory Care, 48, 248-260. Sander, N., (2002). Making the grade with asthma, allergies, and anaphylaxis. Pediatric Nursing, 28, 593-598. 10 Schaefer, R., Stadler, J., & Gosain, A. (2003). To distract or not to distract: An algorithm for airway management in isolated Pierre robin sequence. Plastic and Reconstructive Surgery, 113, 1113-1125. Schibli, S., Durie, P. & Tullis, E. (2002). Proper usage of pancreatic enzymes. Current Opinion in Pulmonary Medicine, 8(6), 542-546. Schuster, M., Franke T., & Pham C.(2002). Smoking patterns of household members and visitors in homes with children in United States. Archives of Pediatric Adolescent Medicine, 156, 1094-1100. Society for Adolescent Medicine (2003). Transtion to adult healthcare for adolescents and young adults with chronic conditions. Journal of Adolescent Health, 33309-311. Sterling, Y., & El-Dahr, J. (2006). Wheezing and asthma in early childhood: An update. Pediatirc Nursing, 32(1), 27-31. Trollvik, A., & Severinsson, E. (2005). Influence of an asthma education program on parents with children suffering from asthma. Nursing and Health Sciences, 7, 157-163. Velissariou, I., & Papadopoulos, N. (2006). The role of respiratory viruses in the pathogenesis of pediatric asthma. Pediatric Annals, 35, 637-642. Velsor-Friedrich, B., Pigott, T.D. & Louloudes, A. (2004). The effects of a school-based intervention on the self-care and health of African-American inner-city children with asthma. Journal of Pediatric Nursing, 19, 247-256. Weiland, J., Schoettker, P.J., Byczkowski, T., Britto, M.T., Pandzik, G. & Kotagal, U.R. (2003). Individualized daily schedules for hospitalized adolescents with cystic fibrosis. Journal of Pediatric Healthcare, 17, 284-289. Yankaskas, J.R., Marshall, B.C., Sufian, B., Simon, R.H. & Rodman. D. (2004). Cystic 11 Fibrosis adult care: Consensus conference report. Chest, 125, 1S-39S. 12 Addenda Care Path 16-1 - An Interdisciplinary Plan Of Care for the Child with Apnea Nursing Diagnosis: Ineffective breathing pattern related to apneic episodes. Child/Family Outcomes: Child will have effective breathing pattern without apneic spells throughout hospitalization. Nursing Diagnosis: Impaired home maintenance related to change in home care regimen. Child/Family Outcomes: Parents will verbalize understanding of necessary diagnostic tests and consultations. Parents will describe and demonstrate understanding of CPR and home apnea monitor prior to discharge. Nursing Diagnosis: Interrupted family processes related to anxiety associated with threat of infant death. Child/Family Outcomes: Parents will develop open communication with healthcare team and receive patient information in a timely manner. Parents will verbalize understanding of need to develop support system to provide respite care. Care Intervention Admission Categories Consults Transition to Discharge to Discharge Community Social service Teach Specialty services parent/family such as members CPR Pulmonary and (basic life Gastroenterology support) and 13 evaluate return demonstration Nursing Check vital signs Vital signs every Discontinue pulse Assessment and every 4 hr 4 hr oximetry. Care Management Daily weights. Pulse oximetry Place home monitoring Height on spot checks. device on child. admission Assess and Assess response to reflux Complete document precautions. assessment, with respiratory emphasis on responses to care. respiratory Pulse oximetry system spot checks. Cardiorespiratory Keep child monitor (Apnea upright for 30-45 monitor) minutes following Pulse oximetry feeding. Keep head of bed Position on elevated. abdomen between Avoid feedings. hyperflexion of neck. Initiate documentation of 14 apneic episodes. Diagnostic Tests & Possible tests Repeat diagnostic Procedures include CBC, tests as indicated capillary blood by child’s gases, calcium, condition. electrolytes, glucose, septic work-up Aminophylline requires blood level monitoring. Chest radiograph ECG, EEG Pneumogram (pneumocardiogra m) If history indicates, upper GI series, reflux scan, Ph probe, polysomnography Pharmacologic As ordered by As ordered by Continue with Management healthcare healthcare medications, as ordered 15 Nutrition professional professional Gastroesophageal Gastroesophageal reflux reflux medications, if medications, if indicated indicated Accurate intake Diet for age as and output tolerated. Diet for age as tolerated. Maintain reflux Reflux Maintain reflux precautions if precautions if diagnosed with needed. precautions if needed. reflux. Discharge planning Orient family to Notify discharge Hold discharge / Teaching hospital and planner of need conference with parents primary for home nursing to review teaching needs, caregivers. referral at time of follow-up clinic visits, Have family discharge. equipment needs, and verbalize Find out whether financial resources. understanding of family has Instruct parents to keep monitors and telephone. log of apneic episodes to diagnostic Advise family of include time, child’s studies. home nursing activity at time of 16 Have family referral. episode, and verbalize Complete home interventions to stimulate understanding of healthcare the child. infant's referral. Provide parents with cardiopulmonary Contact home information on support system. health agency. group or name of other Have family family with child on demonstrate Begin CPR apnea monitoring at reflux teaching. home. precautions, Have family Have parents notify medication demonstrate use neighborhood EMT of administration, of home monitor. child’s status. monitor Have family Home visit by home care application, steps demonstrate CPR. agency is scheduled. to answer monitor Review Follow up appointments alarms. scheduled. guidelines for using home monitoring with parents. Suggest educating secondary care providers regarding 17 monitor use and CPR. CBC, complete blood count; CPR, cardiopulmonary resuscitation; EEG, electroencephalogram; ECG, electrocardiogram; EMT, emergency medical technicians; GI, gastrointestinal. Care Path 16-2 - An Interdisciplinary Plan of Care for the Child with Bronchiolitis Nursing Diagnosis: Ineffective breathing pattern related to bronchospasm, mucosal edema, and accumulation of mucus. Child/Family Outcomes: Child will demonstrate improved breathing pattern, as evidenced by absence of tachypnea, retractions, nasal flaring, grunting, wheezing, cyanosis, or cough. Nursing Diagnosis: Impaired gas exchange related to bronchiolar obstruction, atelectasis, and hyperinflation. Child/Family Outcomes: Child will demonstrate adequate oxygenation and ventilation, as evidenced by oxygen saturation >92% and decreased work of breathing. Nursing Diagnosis: Deficient fluid volume related to dyspnea, tachypnea, and decreased oral intake. Child/Family Outcomes: The child will maintain adequate intake and output for age and weight. The child will maintain adequate hydration, as evidenced by moist mucous membranes, good skin turgor, and serum electrolytes within normal range. 18 Nursing Diagnosis: Deficient knowledge related to home management of bronchiolitis. Child/Family Outcomes: Family will demonstrate knowledge of and adherence to home treatment plan. Care Admission Intervention Transition to Discharge to Discharge Community Categories Consults Pediatric pulmonologist prior to initiation of ribavirin, if needed Infection control specialist Nursing Vital signs and pain Vital signs and pain Discontinue Assessments and q 2-4 hours based every 4 hours cardiopulmonary Care on acuity Pulse oximetry spot monitor. Management Blood pressure on checks with Discontinue pulse admission respiratory oximetry. Strict intake and treatments and PRN Activity as tolerated output for respiratory Cardiopulmonary distress monitor Keep head of bed Continuous pulse elevated. oximetry Activity as Discontinue isolation. 19 Keep head of bed tolerated elevated. Bulb suction with Activity as normal saline PRN tolerated for congestion. Bulb suction with Suction with normal saline PRN catheter and saline for congestion. only for airway Suction with obstruction causing catheter and saline substantial only for airway respiratory obstruction causing compromise. substantial Contact isolation respiratory during non- compromise. epidemic period; Contact isolation contact precautions during non- plus droplet epidemic period; precautions during contact precautions RSV epidemic plus droplet periods precautions during RSV epidemic periods Diagnostic Tests CBC with Repeat diagnostic 20 & Procedures differential tests as indicated by Blood culture if child’s condition child appears very ill or temperature is >102F Consider blood gas measurements Nasal washing for RSV panel (if indicated) Chest Radiograph (if indicated) Pharmacologic IV antibiotics if Maintain IV fluids Management strong suspicion or if not taking PO evidence of feeds well or bacterial infection change to Acetaminophen15 heparin/saline lock. mg/kg PO/PR every 4 hrs p.r.n. (if fever 1010F or mild pain);max dose = 75 mg/kg/day or 4 gm/day; whichever Discontinue IV. Room air 21 is less Ibuprofen 10 mg/kg PO every 6 hrs (if fever >1010F or discomfort) if acetaminophen is not effective; max dose+ 400 mg Neo-Synephrine 1/8%; 2-3 drops each nostril every 6 hrs PRN for nasal congestion IV fluids at maintenance if clinically dehydrated or not taking PO feeds Nutrition NPO if in Diet for age respiratory distress Encourage PO PO feedings if feeds and fluid Diet for age 22 RR<60 Psychosocial intake. Parental support for anxiety Rest for parent if sleep deprived Respiratory Suction prn, before Begin weaning Discontinue O2. feedings and before oxygen to keep O2 Room Air inhalation therapy. saturation >94%. Oxygen to keep O2 saturation >92% or for severe respiratory distress Discharge Teach family to use Teach about home Discharge if Ribavirin planning / bulb syringe and medication therapy not needed. Teaching watch them administration. Return to clinic if practice. Ensure family signs/symptoms of understands dosing respiratory distress and purpose of recur. medications. Home nebulizer, if needed Assess smoking status in home, 23 refer family for smoking cessation and encourage smoke-free homes and cars. ADLs, activities of daily living; CBC, complete blood count; ECG, electrocardiogram; IM, intramuscular; IV intravenous; NPO, nothing by mouth; PO, by mouth; RR, respiratory rate; RSV, Respiratory Syncytial virus Care Path 16-3 - An Interdisciplinary Plan of Care for the Child with Pneumonia Nursing Diagnosis: Ineffective breathing pattern related to an inflammatory infection of the lower airway Child/Family Outcomes: Child will demonstrate and maintain an improved breathing pattern throughout hospitalization, as evidenced by lessening or absence of tachypnea, retractions, nasal flaring, grunting, wheezing, cyanosis, and/or cough. Nursing Diagnosis: Deficient knowledge related to disease process and home management of child upon discharge Child/Family Outcomes: Family will verbalize understanding of illness and rationale for treatment plan. By discharge, family will verbalize/demonstrate an understanding of how to administer medication at home, how to perform PD&P, how to use a bulb syringe and an MDI as appropriate, and when to notify physician of changes in respiratory status. 24 Care Admission Intervention Transition to Discharge to Discharge Community Categories Nursing Check vital Vital signs every 4 hr Discontinue apnea Assessment and signs every 4 hr I&O every shift monitor. Care Strict intake and Apnea monitor as Activity as tolerated Management output indicated Discontinue isolation Consider apnea SpO2 p.r.n. for monitor for respiratory distress infants <6 mo Activity as tolerated with moderate Maintain contact to severe isolation. respiratory distress. SpO2 check once, and then check p.r.n. for respiratory distress. 25 Activity as tolerated Contact isolation Diagnostic Tests CBC with Repeat diagnostic & Procedures differential tests as indicated by Consider blood child’s condition. culture and cold agglutinins. Chest radiograph Spirometry for children (> 6 yrs) with comorbid conditions (e.g., CF, asthma, neuromuscular, etc.) Pharmacologic Ampicillin 200 Once PO intake is Discontinue Neo- Management mg/kg/day IV q consistently 75% or Synephrine (>3 day use 6 hrs more of maintenance, not recommended). 26 (maximum 2 switch to g/dose) heparin/saline lock Change to oral Or IV antibiotics. Cefuroxime 75- For bacterial pneumonia, 150 mg/kg/day discharge on PO IV q 8 hr for antibiotics to complete a bacterial 10-day course. pneumonia (maximum Discontinue dose, 1.5 heparin/saline lock. g/dose) Neo-Synephrine 1/8%, 2-3 drops each nostril every 6 hr, p.r.n. for nasal congestion. Acetaminophen 15 mg/kg (max dose 650 mg) PO/PR every 4 27 hours PRN T>101F or discomfort Ibuprofen 10 mg/kg (max dose 400 mg) PO every 6 hours PRN T>101F or discomfort if acetaminophen is not effective. Heparin/saline lock or consider IV fluids at maintenance if unable to take PO feeds. Nutrition NPO if Diet for age; respiratory encourage fluids distress (clear); avoid dairy Diet for age as tolerated 28 symptoms or products vomiting Respiratory Oxygen to keep Encourage deep Discontinue oxygen. saturation >92% breathing and Room air Bulb or wall directed cough every Discontinue nebulized suction p.r.n. 4 hours while awake. treatments. PD&P with Consider weaning Use albuterol MDI 2-4 nebulized oxygen. puffs via aerochamber treatments, if Consider alternating every 4-6 hr, if clinically clinically nebulized treatments indicated. indicated with MDI treatment. (atelectasis or Or lobar Discontinue pneumonia nebulized treatments identified by and use albuterol chest MDI 2-4 puffs every radiograph) 4-6 hr, if clinically Albuterol 0.15 indicated. mg/kg in 2 mL Wean oxygen as normal saline tolerated. via nebulizer every 2-4 hr and p.r.n. (minimum 29 diluted dose 0.25 mL) Discharge Provide Review all teaching Discharge to home if on Planning / education on content. Provide room air, respiratory Teaching how to information on home treatment not needed recognize medication more than every 4-6 hr, worsening administration, and tolerating PO feeds. respiratory including Instruct parent to call distress, signs discontinuation and physician if respiratory of inadequate follow-up distress is noted. PO intake; how instructions. Ensure that parent makes to use a bulb a follow-up appointment syringe (for within 1 week of infants and discharge. toddlers), and how to do respiratory treatments. I&O, input and output; MDI, metered-dose inhaler; NPO, nothing by mouth; PD&P, postural drainage and percussion; PO, by mouth; SpO2, arterial blood oxygen saturation. 30 Care Path 16-4 - An Interdisciplinary Plan of Care for the Child with Cystic Fibrosis Nursing Diagnosis: Impaired gas exchange related to increase pulmonary secretions. Child/Family Outcomes: From baseline at admission, the child will demonstrate improved gas exchange with improved airway clearance measured by: -Decreased respiratory rate -Decreased use of accessory muscles. – Decreased secretions – Increased airway clearance – Improved or back to baseline PFTs – Increased 02 saturation/baseline – Decreased cough – Increased exercise tolerance. . Nursing Diagnosis: Imbalance nutrition: less than body requirements related to interference with enzyme production, compromised respiratory status, increased metabolic requirements due to work of breathing, infection, and malabsorption and/or decreased appetite. Child/Family Outcomes: Child will ingest adequate nutrients based on individual needs. 31 Child will have stools of normal consistency, frequency, and color. Nursing Diagnosis: Potential for nonadherence to self-care related to chronic nature of condition and developmental level. Child/Family Outcomes: Child and family will attain and maintain behavior that is consistent with goals of therapy. Nursing Diagnosis: Potential for ineffective coping related to chronic illness and the risk of life-threatening complications. Child/Family Outcomes: Family members will verbalize feelings about the illness and its effect on their lives; will identify family and community resources, social support. Nursing Diagnosis: Readiness for enhanced self concept related to appearance, treatment regimen, and limitations on activities. Child/Family Outcomes: Child will have a positive self-concept and value personal strengths. Child will express feelings about the disease and limitations it imposes. Child will demonstrate accomplishments in areas of interests. Care Intervention Admission Categories Consults CF Team and Transition to Discharge to Discharge Community Social Work 32 specialists as needed (e.g., endocrine) Nursing Assessment Admission Weight daily Discontinue and Care weight Management Vital signs and Vital signs and pain assessment pain assessment q Discontinue q 4 hr 4 hr pulse oximetry. Monitor stool Ad lib ADL’s calorie count Respiratory assessment. pattern Monitor stool Calorie count Discontinue pattern p.r.n. isolation Calorie count Spot pulse p.r.n. oximetry for O2 Spot pulse saturations>92% oximetry for O2 Continuous pulse saturations>92 oximetry for O2 % saturations< 92% Continuous pulse oximetry Ad lib ADL’s for O2 saturations< Continue reverse 33 92% isolation. Avoid contact Ad lib ADL’s with other CF patients. Reverse isolation to prevent infection with multiple resistant organisms Avoid contact with other CF patients. Diagnostic Tests & CBC with Assess Procedures differential aminoglycoside Sputum culture therapy. and sensitivity Levels with third labeled for CF to fourth dose; Basic repeat if dose biochemical adjusted panel, including Follow up on renal and liver abnormal 34 functions and laboratory values. glucose Assess culture Other results and laboratory tests sensitivities. p.r.n.; UA, Consider work-up AFB, sputum for allergic for fungal bronchopulmonar cultures, IgE, y aspergillosis HbA1c (ABPA). Chest Consider workup Radiograph post for cor anterior and pulmonale, ECG, lateral views O2 desaturation Spirometry study as indicated PFTs for >5 by clinical status. years ABG as indicated Pharmacologic Determine Continue with Continue with Management venous access medications as medications as option: initiate ordered. ordered. IV, PICC, or Heparin flush as access indicated for Discontinue IV. 35 implanted PICC or central venous access line Heparin flush as device. indicated for Standard IV PICC or central solution for line pediatric maintenance at patients, unless home patient has glucose intolerance Heparin/saline lock may be used. Pulmonary medications/aer osolized/antibio tics/DNase Pediatric enzymes Vitamins H2 blockers Prokinetic agents 36 Antibiotics NSAID’s/ analgesics Nutrition Regular diet Regular diet (high Regular diet (high calories) calories) (high calories) Snacks t.i.d. Snacks t.i.d. Snacks t.i.d. Night Night Night supplemental supplemental supplemental feeds for 10-12 feeds for 10-12 feeds if hours as hours as indicated indicated indicated Assess need for home enteral program and placement of gastrostomy tube. Psychosocial Initiate Continue Resume school Social Service therapeutic therapeutic activities upon Play therapy/school play/recreationa play/recreational discharge. l activities as activities as appropriate. appropriate. Incorporate Continue to schoolwork into incorporate 37 daily schedule. schoolwork into daily schedule. Respiratory PD&P and PD&P and ACT’s Return to usual ACT’s while while awake home treatment, awake O2 as indicated unless O2 as indicated exacerbation requires additional respiratory support in the home (e.g., oxygen, more frequent PD&P) Discharge planning / Assess self-care Assess/instruct in Confirm Teaching behaviors and adherence to understanding provide age- treatments/medica of discharge: appropriate tion/nutrition -Follow-up education for plan. plan/ medical Provide education appointment on symptom -Return to management. school/work selfmanagement. Assess home 38 and community Identify home Obtain resources. care needs and prescription for initiate referrals: discharge - needs. Nutritional/entera l supplements -Respiratory durable medical equipment for airway clearance, O2; etc. -Home IV antibiotics and labs Track progress of education for new home care skills. Consider home health referral. ABG, arterial blood gases; ACT, airway clearance technique; AFB, acid-fast bacilli; ADLs, activities of daily living; CBC, complete blood count; CF, cystic fibrosis; ECG, electrocardiogram; HbA1c hemoglobin A1c , IgE, 39 immunoglobulin E; NSAID, nonsteroidal anti-inflammatory drug; O2, oxygen; PD&P, postural drainage and percussion; PFT, pulmonary function tests; PICC, peripherally inserted central catheter; UA, urinalysis.