Guideline For Connective Tissue Disease
advertisement

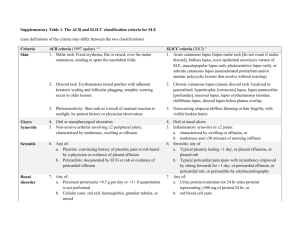
Guideline for Connective Tissue Disease Suggestive Symptoms to Connective Tissue Disease • 1. Skin Rash – Malar, discoid rash, photosensivity • 2. Swelling of joints - mono/oligo(3~5)/poly (>5) • 3. Serositis –Presence of pericardial or pleural effusion of • 4. Seizures – unknown etiology or offending drugs • 5. Psychosis – unknown etiology or offending drugs • 6. Fever – • 7. Fatigue – Weakness of extremities, especially • 8. Myalgia/myositis – nonspecific muscle pain unknown infection focus or unknown etiology. malignancy Suggestive Physical Findings to Connective Tissue Disease • Alopecia, hair loss • Dry eyes • dry mouth, Oral/nasal ulcers • Vasculitic lesions, Adenopathy • Edema • Cyanosis of fingers in cold weather or during emotional stress Initial Serological Evaluation with Antinuclear Antibody • If ANA negative – Symptoms remit, SLE not present • If ANA negative – Symptoms persists, • - repeated ANA • - check other markers (Rheumatic factor) • If RF negative – Check HLA-B27, Study Sero-negative Arthropathy (Ankylosing Spondylosis, Reiter’s syndrome, Psoriatic Arthritis) • If RF positive – consider as ANA positive, also study disease associated with RF.(See after) Diseases Commonly Associated with Positive Rheumatoid Factor • Rheumatic diseases • Rheumatoid arthritis, systemic lupus erythematosus, connective tissue disease, scleroderma, mixed Sjogren's syndrome • Viral infections • Acquired ImmunoDeficiency Syndrome, hepatitis, mononucleosis, influenza, ers; after vaccination (may yield falsely elevated titers of antiviral antibodies) • Parasitic infections • Trypanosomiasis, kala-azar, malaria, schistosomiasis, filariasis • Chronic bacterial infections • Tuberculosis, leprosy, yaws, syphilis, brucellosis, subacute bacterial endocarditis, salmonellosis • • • • Neoplasms After irradiation or chemotherapy Other hyperglobulinemic states Hypergammaglobulinemic purpura, cryoglobulinemia, chronic liver disease, sarcoid, other chronic pulmonary diseases Initial Serological Evaluation with Antinuclear Antibody • If ANA positive, consider diseases below before diagnosis of SLE • - Check CPK, EMG, NCV, muscle/skin biopsy • for DermatoMyositis/PolyMyositis • • • • • • - Survey Systemic Sclerosis(Scleroderma), CREST - Mixed Connective Tissue Disease (Anti-RNP) - Drug-induced lupus - Sjogren’s syndrome If ANA positive, with no symptom, or only one or two symptoms that are suggestive of connective tissue disease - Undifferentiated Connective Tissue Disease(UCTD) Laboratory investigations for Connective Tissue Disease • Urine Routine – proteinuria > 3+, Daily protein >0.5g. CCR • • • • • • • • Complete Blood Count & Differential Count, platelet – hemolytic anemia, leukocytopenia, thrombocytopenia – if agranulocytosis, consider drug-induced. E.S.R, CRP – acute phase reactant, follow-up of disease activity, CRP to rule out infection. Glucose, Bun, Cr, Na, K – Renal Function Test Bil(T/D), GOT/GPT – liver function, autoimmune hepatitis Lipid profile – Triglyceride, Cholesterol in nephrotic syndrome Albumin – edema/proteinuria/nephrotic syndrome • PT/APTT – Prolonged time even mixed with normal serum. • RPR – false positive indicates presence of antiphospholipid antibody • Anti-dsDNA – related with lupus nephritis • ENA-screening(Anti-SM, Anti-RNP,Anti-SSA/SSB) • Anticardiolipin Ab, Lupus Anticoagulant How to Establish A Diagnosis • What is Criteria for CTD? Classification rather than Diagnosis • Evaluation of System: • - mucocutaneous subacute cutaneous LE, Discoid LE • • • - musculoskeletal: lupus myositis, lupus arthritis - kidney: lupus nephritis - heart & vessels: lupus pericarditis, atherosclerosis, Antiphospholipid syndrome • - Stomach system: lupus vasculitis of intestine • - Brain: CNS lupus Condition That may confused with systemic lupus erythematosus • Undifferentiated connective tissue disease • Sjogren’s syndrome • Antiphospholipid antibody syndrome • • • Fibromyalgia with positive antinuclear antibody Idiopathic thrombocytopenia purpura Drug-induced lupus • Early rheymatoid arthritis • Vasculitis Evaluation of patient’s condition • 1. Infection • 2. Drug-related complication • 3. Disease flare-up Infection • Always rule out infection first in febrile patient with confirmed connective tissue disease. • Detail physical examination • Infection study including blood culture, Chest X-ray, U/A, Sonography of abdomen, CSF-study, cellulitis. • Aggressive antibiotic treatment if condition deteriorated and sepsis is highly suspected. Recommended monitoring strategy for drugs commonly used in SLE Drug Toxicities requiring monitoring System review Laboratory Baseline evaluation Salicylates,nonSteroidal antiinflammatory drugs Gastrointestinal bleeding,hepatic toxicity, renal toxicity, hypertension CBC, creatinine, urinalysis, AST, ALT Dark/black CBC yearly, stool,dyspepsia, creatinine nausea/vomiting, yearly abdominal pain, shortness of breath, edema Glucocorticoids infections, Hypertension, hyperglycemia, hyperlipidemia, hypokalemia, osteoporosis, avascular necrosis, cataract, weight gain, Fluid retention Hydroxy-chloro Macular damage quine Drug allergy BP,glucose, Polyuria, Urinary dipstick potassium, cholesterol, bone densitometry triglycerides (HDL, LDL) polydipsia, edema, shortness of breath, BP at each visit, visual changes, bone pain for glucose every 3–6 months, total cholesterol yearly, bone densitometry yearly to assess osteoporosis None unless patient is over 40 years of Visual changes Funduscopic and visual fields age or has previous eye disease every 6–12 months Drug Toxicities requiring monitoring System review Baseline evaluation Laboratory Azathioprine Myelosuppression, CBC, platelet Symptoms of CBC and hepatotoxicity, count,creatinine, lymphoproliferative AST or ALT Disorders pancreatitis myelosuppression platelet count every 1–2 weeks with changes in dose (every 1–3 months thereafter), AST yearly, Pap test at regular intervals Cyclophosphamide Myelosuppression, CBC and DC and myeloproliferative platelet count, disorders, urinalysis malignancy, immunosuppression , hemorrhagic Symptoms of CBC and myelosuppression urinalysis , monthly, urine hematuria, cytology and Infertility Pap test yearly for life cystitis, secondary infertility Methotrexate Myelosuppression, hepatic fibrosis, cirrhosis, pulmonary infiltrates, fibrosis CBC, CXR within past year, hepatitis B, C serology in high-risk patients, AST, albumin, bilirubin, Creatinine Symptoms of CBC and myelosuppression platelet count , every 4–8 shortness of weeks, AST breath, or ALT every nausea/vomiting, 4–8 oral ulcer weeks, albumin every 4–8 weeks, serum creatinine, urinalysis Evaluate Disease Activity • Clarify Life-threatening and not life-threatening condition • (1) Mild, not organ or life-threatening • (2) Impairs quality of life but not organ or life threatening • (3) Severe disease, organ or life threatening, potentially reversible Serious and Life-Threatening Manifestations of SLE: Responses to Glucocorticoids • Vasculitis • Severe dermatitis of subacute cutaneous LE or SLE • Polyarthritis • Polyserositis--pericarditis, pleurisy, peritonitis • Myocarditis • Lupus pneumonitis • Glomerulonephritis--proliferative forms • Hemolytic anemia • • Thrombocytopenia Diffuse CNS syndrome --acute confusional state, demyelinating syndromes, intractable headache • Serious cognitive defects • Myelopathies • Peripheral neuropathies • Lupus crisis Manifestations not often responsive to glucocorticoids • Thrombosis--includes strokes • Glomerulonephritis--scarred end-stage renal disease, pure membranous glomerulonephritis • Resistant thrombocytopenia or hemolytic anemia--occurs in a minority of patients; consider splenectomy, cytotoxics, danazol, or cyclosporine/neoral therapies • Psychosis related to conditions other than SLE, such as glucocorticoid therapy Manifestations of SLE That Can Be Managed with Strategies Other Than Immunosuppression • Thrombosis • • • Recurrent fetal loss with antiphospholipid Thrombocytopenia or hemolytic anemia Seizures without other serious manifestations • • Behavior disorders or psychosis without other serious manifestations Pure membranous glomerulonephritis