Overview of Rheumato..
advertisement
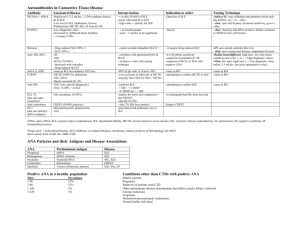
Overview of Rheumatology Labs: Alphabet soup? Pediatric Rheumatology Red Team Resident Teaching Series What are all those letters? • • • • • • • • • • • ESR ANA CRP dsDNA ENA RNP Smith SS-a/SS-b Cardiolipin Jo-1 CPK • • • • • • • • • • • • p-ANCA/ c-ANCA RF C3/C4 CH50 Histone Centromere Scl-70 VDRL/RPR DRVVT Beta 2 glycoprotein 1 LDH Aldolase Background • Rheumatology spans a group of diseases that have auto-immune components • Proposed mechanisms to auto-immunity including cross reactive antigens, molecular mimicry, and autoantibody amplification • We can identify auto-antibodies and therefore characterize clinical diseases • However, presence of auto-antibodies does not always predict disease Diagnostic vs. Evaluative Tests • Need to distinguish to determine which test is appropriate • Diagnostic tests accurately distinguish a group of patients with a specific disease from a non-disease group • Evaluative tests monitor disease activity over time Erythrocyte Sedimentation Rate (ESR) • Mainly used as a disease activity indicator • Method: Westergren method (most common) which measures the rate of settling of RBCs in anticoagulated whole blood • Nonspecific test of inflammation • Elevated in infection, IBD, cancer, pregnancy, trauma, and stress • Can be falsely low in conditions that don’t let RBCs undergo rouleaux formation (sickle cell anemia, Hereditary Spherocytosis, CHF, polycythemia) Anti-nuclear Antibodies (ANA) • Immunoglobulins directed against structures within the cell (i.e. DNA, ribonuclear proteins, histones, and centromere) • Titer is important; pattern not important • Found in a variety of autoimmune diseases such as SLE, MCTD, JRA, scleroderma, Sjogren’s syndrome in high titers (>1:320) • Almost always present in SLE (95-98%) • Low titers (<= 1:160) found in: • Infections (EBV, CMV, Hepatitis B, bacterial endocarditis, HIV) • Drugs (hydralazine, INH, dilantin, tegretol, ETX, PCN, and sulfas) • Neoplasias (lymphoma) • It is sensitive but not that specific • Consider using as a screening test in only symptomatic patients • Approximately 10% of the population has a positive low titer ANA and can be asymptomatic • ANAs do not correlate with disease activity ( i.e. diagnostic test) • If positive, should subtype (anti-dsDNA, ENA panel) • Must measure ANAs in patients with JIA to assess risk of uveitis ANA Subtype: Double Stranded DNA (anti-dsDNA) • • • • • • Anti-dsDNA antibody is an ANA subtype In higher titers, highly specific for SLE Seen in >80% of SLE patients at some time during their course Associated with the presence of active lupus nephritis Can detect flare up before clinically significant Check anti-dsDNA levels if you suspect SLE in a child with positive ANA ANA Subtype: Anti-Extractable Nuclear Antibodies (anti-ENA) • anti-Smith (Sm) and anti-ribonucleoprotein (RNP) • Both are directed against RNA proteins and are readily soluble in neutral buffers • Anti-RNP is specific for MCTD (high titer) • Anti-Sm ab is highly specific for SLE • 10-20% in Caucasians, 30% in Asians, 40% in African Americans • One of the lupus criteria ANA Subtype: Anti Ro/SS-A and Anti La/SS-B • Associated with Sjogren’s, SLE, and neonatal lupus • Anti Ro/SS-A antibodies seen in: • 5-15% of normals • 50% of Sjogren’s patients • 30% of SLE patients (many have negative ANA or subacute cutaneous lupus) • Correlates with active nephritis and cytopenias • Crosses the placenta and is associated with neonatal SLE and heart block • Anti La/SS-B antibodies seen in: • • • • 5% of normals 15-85% of Sjogren’s patients 10-15% of SLE patients Also associated with neonatal SLE but do not see the cardiac manifestations ANA Subtype: Anticentromere, AntiScl-70, and Antihistone Antibodies • Anticentromere Antibodies seen in limited cutaneous systemic sclerosis • Anti-Scl-70 Antibodies (also known as anti-topoisomerase I) are assoicated with increased risk of pulmonary fibrosis in both limited and diffuse cutaneous systemic sclerosis • Anti-histone antibodies are found in 95% of patients with drug-induced lupus syndrome • Seen with: • • • • Procainamide Quinidine Hydralazine Phenytoin or other anti-epileptics Antineutrophil Cytoplasmic Antibodies (ANCA) • Associated with vasculitides • Used as diagnostic test and possibly an evaluative test (still questionable) • 2 main staining categories: c-ANCA and p-ANCA: • Cytoplasmic ANCA (c-ANCA) – coarse granular staining of the cytoplasm. The main antigen is proteinase-3 (PR3). Seen in 90% of Wegener’s granulomatosis. • Perinuclear ANCA (p-ANCA) – staining of the nucleus and perinuclear area leaving cytoplasm clear. Main antigen is myloperoxidase (MPO). Associated with microscopic polyarteritis nodosa, Churg-Strauss, and Ulcerative Colitis. Rheumatoid Factor (RF) • Uncommon in children • Should NOT be used as a screening test for rheumatic disease in children • Only indication is for polyarticular JIA patients to classify and offer prognostic information • Low titers seen in healthy children (<5%), infections (viral, SBE), malignancy, SLE • High titers seen in JIA (<20%) and predictive of erosive joint disease (follows adult RA course more) and MCTD HLA-B27 • One of the histocompatibility genes • Associated with seronegative spondyloarthropathies: • • • • ankylosing spondylitis (AS) (up to 90%) IBD (25-50%) psoriatic arthritis (<25%) reactive arthritis (50-75%) • Less than 20% patients with HLA-B27 develop AS Complements • Used to document complement consumption and diagnose rare complement deficiencies • CH50 (overall complement level) is decreased in SLE, MCTD, and immune complex vasculitis • Most common congenital complement deficiency is C2 • Low C3 and C4 levels seen in active lupus • Complement levels help follow disease activity and response to treatment in SLE • Considered a diagnostic and evaluative test Antiphospholipid Antibodies (aPL antibodies) • Group of antibodies against a variety of phospholipids and phospholipid binding plasma proteins • Associated with syndrome of coagulopathy, thrombocytopenia, recurrent spontaneous abortions, livedo reticularis, migraines, TTP, chorea, myelitis, and avascular necrosis of bone • Can occur with SLE (30-40%), or seen without other autoimmune disease (antiphospholipid antibody syndrome) 1. Positive anti-cardiolipin antibodies (aCL) • • 2. 3. 4. IgG – associated with thrombosis IgM – associated with thrombocytopenia only Positive lupus anticoagulant: misnomer; antibody on the phospholipid of the prothrombin activator complex that causes in vitro anticoagulation (elevated aPTT and positive DRVVT) but in vivo paradoxical thrombosis Dilute Russell Viper Venom Test (DRVVT) β2glycoprotein-1 IgG and IgM Practice Question #1a • A 3 year old girl with a two month history of a swollen and painful knee and eye findings Practice Question #1b • A 15 year old girl with multiple joint pains and joint swelling Practice Question #1c • A 8 yo boy with persistent fevers, intermittent rashes, and joint pain Answer for Question 1a-c: Juvenile Idiopathic Arthritis • • • • • CBC-D ESR ANA to determine uveitis risk If polyarticular course, add RF If older onset with sacroiliac tenderness and tendon insertion site tenderness, add HLA-B27 • If systemic course, add LFTs, Ferritin, DDimer Practice Question #2 • A 13 year old Hispanic girl with a facial rash, joint pain, mouth sores, fatigue, and blood in her urine Answer for Question #2: Systemic Lupus Erythematosus • • • • • • • CBC-D ESR ANA dsDNA C3/C4 levels Urinalysis and Urine protein/creatinine ratio Antiphospholipid Antibodies (Anti-cardiolipin ab, PTT, DRVVT, and LAC, B2glycoprotein) Practice Question #3 • A 6 year old boy with muscle weakness, leg pains, and rash over his eyelids and on his elbows Answer for Question #3: Dermatomyositis • • • • • CBC-D ESR ANA CPK, Aldolase, LDH (muscle enzymes) AST/ALT (in this case, as a muscle enzyme)