Treacher Collins Syndrome
advertisement
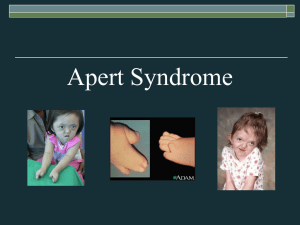
Treacher Collins Syndrome What is Treacher Collins Syndrome? Treacher Collins Syndrome, also called mandibulofacial dysostosis, affects the head and face. Characteristics include: down-slanting eyes notched lower eyelids underdevelopment or absence of cheekbones and the side wall and floor of the eye socket lower jaw is often small and slanting forward fair in the sideburn area underdeveloped, malformed and/or prominent ears Most children with Treacher Collins have normal development and intelligence; however, it is important that there be early hearing tests. Most children with Treacher Collins Syndrome benefit from early intervention speech and language programs. Why did this happen? Treacher Collins Syndrome is believed to be caused by a change in the gene on chromosome 5, which affects facial development. About 40 percent of the time, one parent has the Treacher Collins Syndrome gene. Geneticists can now determine whether the Treacher Collins gene is a new mutation or one that has been passed on. Will this happen to children I have in the future? Treacher Collins Syndrome may be inherited from a parent affected with Treacher Collins. There is a 50% change of passing it on if you have it. If may also occur in children of unaffected parents. However, the chances of Treacher Collins occurring again in children of unaffected parents is minute. What kinds of problems could my child have? In addition to the physical characteristics common to Treacher Collins syndrome, your child may have some or all of the following problems: breathing problems and/or eating difficulties most children have a 40% hearing loss in each ear due to abnormalities of the outer and middle ear, which conduct sound to the nerve endings the eyes have a tendency to dry out, which can lead to infection some children have abnormally small or absent thumbs cleft palate often occurs with Treacher Collins Syndrome Will my child need surgery? Depending on the severity of the Treacher Collins, your child may need some or all of the following procedures: a conductive hearing aid correction of the cleft palate repair of the sidewall and floor of the eye socket repair of the cheekbones repair of the eyelid notches correction of the undeveloped jaw and chin surgery to correct the beak-like nose reconstruction of the ears New advances in the procedures to treat Treacher Collins Syndrome are constantly being developed. Be an advocate for your child! How do I get help for my child? Your child should be treated by a qualified craniofacial medical team at a craniofacial center. Currently, FACES has information on thirty-two craniofacial teams located in 20 states, the District of Columbia, and Canada. This is by no means a comprehensive list of all the craniofacial teams. Please contact FACES for details on possible locations closer to you. Klippel-Feil Syndrome In 1912, Maurice Klippel and Andre Feil were independently the first to describe Klippel-Feil syndrome. They described patients who had a short neck, increased range of motion (ROM) in the cervical spine, and a low hairline. Feil subsequently classified the syndrome into 3 categories. Type I is described as a massive fusion of the cervical spine. Type II is present when the fusion of 1 or 2 vertebrae occurs. Type III occurs when thoracic and lumbar spine anomalies are associated with type I or type II Klippel-Feil syndrome. Patients with Klippel-Feil syndrome usually present during childhood but may present later in life. The challenge to the clinician is to recognize the associated anomalies that can occur with Klippel-Feil syndrome and to perform the appropriate workup for diagnosis. Frequency: The true incidence of Klippel-Feil syndrome is unknown. No one has ever studied a cross-section of healthy people to determine the true incidence. The incidence of Klippel-Feil syndrome has been investigated in 2 studies, using 2 different means. Gjorup reviewed all of the radiographic cervical spine films in a single hospital in Copenhagen. From these radiographs, he determined an incidence of 0.2 cases per 1000 people. Brown reviewed 1400 skeletons from the Terry collection at Washington University School of Medicine. He found an incidence of 0.71%. Etiology: The etiology of Klippel-Feil syndrome and its associated conditions is unknown. The syndrome can present with a variety of other clinical syndromes, including fetal alcohol syndrome, Goldenhar syndrome, and other anomalies in the extremities. Gunderson suggested that it is a genetic condition, while Gray found a low incidence of inheritance. Others have considered it to be some type of global fetal insult, which could explain the other associated conditions. Others have considered it to be caused by vascular disruption. The true etiology has yet to be determined. Clinical: Clinical presentation is varied because of all of the associated syndromes and anomalies that can occur in patients with Klippel-Feil syndrome. A complete history and careful physical examination may reveal some associated anomalies. From an orthopedic standpoint, most of the workup is with imaging (see Imaging Studies). The condition is detected throughout life, often as an incidental finding. Patients with upper cervical spine involvement tend to present at an earlier age than those whose involvement is lower in the cervical spine. Most patients present with a short neck, decreased cervical ROM, and a low hairline, which occurs in 40-50% of patients. Decreased ROM is the most frequent clinical finding. Rotational loss usually is more pronounced than is the loss of flexion and extension. Other patients present because of cosmesis or facial asymmetry. Neurological problems may develop in 20% of patients. Pouliken found that 5 of 19 patients with Klippel-Feil syndrome had neurological involvement; of these 5 patients, 2 had neurological problems due to hypermobility at one level. Occipitocervical abnormalities were the most common cause of neurological problems (see Images 1-4). Some patients present with pain. Hensinger and colleagues described the constellation of anomalies that can occur with Klippel-Feil syndrome, and others have added to this list. Scoliosis occurs in approximately 60% of patients (see Images 5-6). In some patients, this is congenital scoliosis (see Image 7) due to the involvement of other parts of the thoracic or lumbar spine. Other patients develop compensatory scoliosis in the thoracic spine to compensate for the cervical or cervicothoracic scoliosis. In addition to the fusion anomalies in the cervical spine, cervical spinal stenosis can occur. While uncommon, this can increase the risk of neurological involvement. Anomalies of the craniocervical junction can cause instability at lower segments. Traumatic tetraplegia has been reported following minor trauma. A Sprengel anomaly occurs in 20-30% of patients (see Image 7). Always check ROM of the shoulders. Look for an omovertebral bone (see Image 8). This is an osteocartilaginous connection that tethers the scapula to the spine. An omovertebral bone ossifies with age, further limiting the ROM. A CT scan best demonstrates an omovertebral bone; however, palpation or radiographs also can detect an omovertebral bone. Other upper extremity anomalies occur less frequently. A thorough examination of the ROM and function of the upper extremity must be performed. Synkinesia is mirror movement of the upper extremity. Patients with this condition are unable to perform a movement of the right hand without performing the same movement of the left hand (see Image 9). This is disabling in activities of daily living (ADL). Synkinesia often may be improved with therapy and usually improves with age. Renal anomalies are common in individuals with Klippel-Feil syndrome, and they can be quite serious. Hensinger reviewed 50 patients, and 41 of them had an intravenous pyelogram (IVP). Renal anomalies were present in 16 (34%). Minor renal anomalies were detected in 6 individuals, including a double collecting system, renal ectopia, and bilateral tubular ectasia. Major renal anomalies were detected in 10 individuals, including hydronephrosis, absence of a kidney (see Image 10), and a horseshoe kidney. As Hensinger notes, the patient of Klippel and Feil died of renal failure and uremia. Patients with Klippel-Feil syndrome now have ultrasound as the initial test to demonstrate the presence of 2 functioning kidneys. Torticollis and facial asymmetry occur in 21-50% of patients with Klippel-Feil syndrome. These patients also may have a muscular torticollis. Craniofacial anomalies also can occur. Hearing loss is common with Klippel-Feil syndrome. The hearing loss can be sensorineural, conductive (one third of cases), or mixed. Hensinger found the incidence of hearing loss to be 36%. Early audiometric evaluation and otologic evaluation are indicated in all children when the diagnosis of Klippel-Feil syndrome is established. Cardiovascular anomalies occur in 14-29% of cases. The most common cardiovascular defect is an interventricular septal defect. Other less common anomalies are congenital limb deficiencies, craniosynostosis, ear abnormalities, iniencephaly, and craniofacial abnormalities. Patients with Klippel-Feil syndrome present at different ages with varying clinical presentations. Indications for the complexity of the workup vary individually. For the orthopedic surgeon, the most usual indications for surgery depend upon the amount of deformity, its location, and its progression with time. Other indications include instability of the cervical spine and/or neurological problems. These indications can occur with craniocervical junction anomalies and also when 2 fused segments are separated by a normal segment. Some patients present early in life with complex cervical and cervicothoracic deformity that is progressive and disfiguring. Some of these patients require cervical spine fusions to prevent progression. Other patients may develop compensatory or associated congenital scoliosis, which also can be progressive over time and requires fusion to prevent progressive deformity. Over one half of the patients in Hensinger's study had scoliosis. Treatment of the scoliosis with bracing or surgery was required in 18 of the 50 patients. Contraindications: Since this is a syndrome with a constellation of possible abnormalities, no set of definite contraindications exists. If a surgeon believes that an operation is indicated, it is incumbent upon him/her to make certain none of the other conditions that could cause morbidity or mortality are present. Cervical or occipitocervical instability could cause increased risk during intubation. An underlying heart defect could increase anesthetic risk. An increased risk of neurologic damage during spinal fusion for correction of deformity could result from underlying spinal stenosis or spinal cord abnormality. A thorough workup of the patient is imperative prior to surgical intervention. Imaging Studies: Plain radiography is the basis for the diagnosis of Klippel-Feil syndrome. o Initial studies include anteroposterior (AP) and lateral views of the cervical spine. o If anomalies are found, carefully assess the craniocervical junction to detect anomalies at that level. o Flexion-extension radiographs are indicated if instability is suspected at the craniocervical junction or if 2 fused segments are separated by an open segment. o Obtain plain radiographs of the entire spine to detect other spinal anomalies. o Examine the chest to rule out involvement of the heart. Examine the chest wall for the possibility of rib anomalies, which can include multiple rib fusions. Rib fusions can be revealed with plain radiography. CT scan often is more useful at the spinal level. o For patients being evaluated for surgery, CT scan with 3-dimensional reconstruction can be a very valuable tool to assess the anatomy. o A unilateral unsegmented bar or cervical stenosis may be revealed on a CT scan, which helps the physician plan the surgical procedure. MRI o MRI is indicated in patients with neurological deficits. o Flexion-extension MRI may reveal cord compression and is useful in evaluating spinal stenosis. o In patients with neurological deficits, obtain an MRI of the entire spine to search for central nervous system anomalies, such as a syringomyelia. Ultrasound initially is performed to visualize the kidneys. Perform intravenous pyelography if any kidney abnormality is suspected with ultrasound. Other Tests: Due to the high incidence of hearing loss with Klippel-Feil syndrome, an audiologist or an otologist should evaluate all children Medical therapy: Medical therapy is dependent upon the congenital anomalies present in the syndrome. Primary care physicians may not be familiar with all of the possible associated anomalies. Patients with genitourinary abnormalities are referred to a nephrologist or urologist. Patients with cardiovascular abnormalities are cared for by a cardiologist or primary care physician. Patients with auditory abnormalities are referred to an audiologist or otologist. Surgical therapy: Surgery is indicated for a variety of situations in patients with Klippel-Feil syndrome. Due to fusion anomalies and the difference in growth potential between the 2 sides of the spine, deformity may be progressive. Instability of the cervical spine can develop because of craniocervical abnormalities. Instability of the cervical spine also can develop between 2 sets of fusion anomalies separated by normal segment. Neurologic deficits or persistent pain are indications for surgery. Development of a compensatory curve in the thoracic spine may require surgical intervention or bracing. Symptomatic spinal stenosis may require decompression and fusion. Koop and colleagues studied 13 cases of children who were skeletally immature with a variety of disorders that caused instability of the upper part of the cervical spine from the occiput to C5. These researchers were looking at the efficacy of posterior arthrodesis and halo-cast mobilization. Many of these patients did not have Klippel-Feil syndrome, but the surgical indications were instability. Posterior arthrodesis with external mobilization by halo-cast was carried out. In 2 of the patients, internal fixation with wire was utilized. A solid arthrodesis was obtained in 12 patients treated with autogenous bone graft. One patient treated with allograft rib developed a pseudoarthrosis. Koop et al cautioned that the use of wires for fixation carries risk of neural injury and often is not applicable in children with anomalous vertebra. They stress the need for delicate exposure, decortication using an air drill, and placement of autologous iliac graft. They recommended mobilization by halo-cast, which they thought would minimize the risk of neural damage and provide a reliable means of obtaining arthrodesis. Preoperative details: Patients must have a comprehensive workup to detect the anomalies previously mentioned. Adequate imaging studies must be obtained. Three-dimensional CT scan reconstruction often is useful. Crouzon syndrome craniofacial dysostosis autosomal dominant premature closure of sutures(craniosynostosis) o usually coronal ==> brachycephaly o all sutures ==> Kleeblatschaedel hypoplasia of facial bones beaked ("parrot") nose A Guide to Understanding Apert Syndrome from the Children's Craniofacial Association highly recommended reading! What is Apert Syndrome? The following was developed from information contained in an article entitled Clinical Assessment and Multispecialty Management of Apert Syndrome, written by Lawrence C. Kaplan, MD, and published in Clinics in Plastic Surgery-Vol. 18, No. 2, April 1991. Major Features of Apert Syndrome Prematurely fused cranial sutures A retruded midface Fused fingers Fused toes Possible Related Features of Apert Syndrome These have been observed in some cases of Apert syndrome, although whether they were caused by Apert syndrome is uncertain. Various heart defects Dextrorotation Pulmonary Atresia Patent Ductus Arteriosus (PDA) Tracheoesophageal Fistula Pyloric stenosis Polycystic kidneys Bicornate uterus Hydrocephalus Ear infections Sleep Apnea Severe acne Increased incidence of eye injuries Definition Apert Syndrome is a genetic defect and falls under the broad classification of craniofacial/limb anomalies. It can be inherited from a parent who has Apert, or may be a fresh mutation. It occurs in approximately 1 per 160,000 to 200,000 live births. Apert syndrome is primarily characterized by specific malformations of the skull, midface, hands, and feet. The skull is prematurely fused and unable to grow normally; the midface (that area of the face from the middle of the eye socket to the upper jaw) appears retruded or sunken; and the fingers and toes are fused together in varying degrees. Apert syndrome is named for the French physician who first described it, E. Apert, in 1906. In a normal child, the skull is made up of several "plates" which remain loosely connected to one another, gradually growing together to form the adult skull. The Apert child's skull, by contrast, has a premature fusion of these plates, restricting brain growth, and causing increased pressure in the brain as it grows. This is known as craniosynostosis. Early surgery relieves the pressures by allowing the plates to be detached from one another. During this early surgery some "cranial remodeling" may be done to give the child a more normal appearance. The "retrusion" or hypoplasia of the midface is what could be described as a concave or dished in profile. As the skull grows, the upper and lower thirds of the face tend to grow at normal rates, but the middle third of the face grows slower, resulting in a more pronounced retrusion over time. A surgical procedure known as the LeFort III is used to correct this condition. The procedure is usually done after substantial growth is complete (preadolescence) and may be repeated as necessary. The LeFort procedure involves detaching the facial bones from mid eye to upper jaw and spacing this area out with bone grafts so that a proper alignment is made. In the last few years, some surgeons have come to prefer the Rigid External Distraction (RED) system or internally placed distractors, instead of or in conjunction with, traditional craniofacial surgery. The fusion of the fingers and toes along with the craniofacial problems mentioned above is what really separates Apert from other similar syndromes. This condition is called syndactyly. It always involves fusion of the soft tissues of the first, middle, and ring fingers, and often there is fusion of the bones themselves. Joint mobility is usually nonexistent past the first joint. The thumb may be fused into the hand, or may be free. Surgery is used to separate the fingers to obtain the highest degree of functionality, and may or may not ultimately result in five digits on each hand. It varies according to the degree of malformation. The feet and toes are affected similarly, but surgery is usually only recommended in cases where the ability to walk would be impaired. Ideally, treatment of Apert begins at birth with the proper diagnosis, identification of the child's individual needs, and the proper facilities to administer what is needed. A multidisciplinary approach is used by physicians in the best arrangements. A craniofacial anomalies team may consist of a craniofacial surgeon, neurosurgeon, ENT, audiologist, speech pathologist, oral surgeon, psychologist, ophthalmologist, and an orthodontist. The team approach is used by these physicians to determine the best collaborative corrective plan for the deficiencies of the child. Genetics Apert syndrome is a result of genetic mutation. When you have Apert syndrome, you have a 1 in 2 (50%) chance of passing this condition to your child. This is because each of us gets 1/2 of our genetic makeup from each parent. However, Apert is not a recessive trait, which means that the UNaffected child of a parent with Apert syndrome is no more likely to have a child with Apert than any other person; also, if you have a child with Apert and you do NOT have Apert, YOU are no more likely to have another child with Apert than anyone else in the population. Studies have shown that Apert occurs more often in children of older fathers. Recently studies were conducted at Oxford University and they managed to identify the actual genetic change which occurs in Apert. The following is a quote from a letter sent to the test families by Oxford. "A total of 86 children and adults affected with Apert syndrome have been seen. From the blood samples which have been donated for research, we have identified the genetic change that causes the condition. The change is in a gene on chromosome number 10 called 'Fibroblast Growth Factor Receptor 2' (FGFR2 for short). We all have two copies of this gene (one from mother, one from father), which is composed of a string of about 2000 of the chemical building blocks that make up the genetic material called DNA. When Apert syndrome occurs, just one particular building block in one of these two gene copies has been exchanged for another. The other gene copy is entirely normal. This one tiny change in the FGFR2 gene results in the physical features of Apert syndrome." CHARGE ASSOCIATION/SYNDROME 1. Definition 2. Epidemiology 3. Etiology 4. Clinical Manifestations 5. Treatment 6. Prognosis 7. Reference Page Definition: CHARGE association (or syndrome) is an acronym referring to children with a specific pattern of birth defects. The acronym is: "C" for coloboma, "H" for heart defects, "A" for atresia choanae, "R" for retardation of growth and development, "G" for genitourinary problems, and "E" for ear abnormalities.19 Epidemiology: The incidence of CHARGE is about 1 out of 10,000-12,000 births. It affects males and females of all races equally.20 Etiology: Etiology is unknown, but it has been suggested that deficiency in migration of neural crest cells, deficiency of mesodermal formation, or defective interaction between neural crest cells and mesoderm play a part in these defects of blastogenesis.21 Some findings suggest that a gene or genes causing some of the anomalies of CHARGE association may reside in the region 14q22-q24.3. All malformation occur in the first trimester. Clinical Manifestations: Traditionally, CHARGE association includes: Coloboma is cleft or failure of the eyeball to close resulting in abnormalities of the retina or optic nerve. This may result in significant loss of vision, defects in visual acuity resulting in near or farsightedness, and oversensitivity to light. Heart defects include Tetralogy of Fallot, the most frequent type of heart defect reported in the CHARGE association. The tetralogy is "an anatomic abnormality with severe or total right ventricular outflow tract obstruction and a ventricular septal defect allowing right ventricular unoxygenated blood to bypass the pulmonary arteries and enter the aorta directly.17(p2059) Atresia choanae is the blocking (atresia)of the airways (choanae) from the back of the nose to the throat that would allow breathing through the nose. Retardation of growth and development is usually due to heart problems, nutritional problems, or growth hormone deficiency. The developmental delay often is associated with sensory deficits (vision and hearing loss). Some children with CHARGE will be mentally retarded. Genitourinary problems, in boys includes genital hyposplasia and possibly undescended testes. The girls may have small labia. Reflux of the urinary tract or kidneys is common. Ear abnormalities include a common finding of unusually shaped ears (short and wide with very little or no earlobe). Hearing loss, conductive and/or nerve, ranges from mild to deafness. Recent literature has supported the classification of CHARGE as a syndrome. They define major criteria specific to CHARGE as the four C's: coloboma (80-90%); choanal atresia (50-60%); characteristic ear abnormalities (90%), and cranial nerve dysfunction (70-90%). Cranial nerve dysfunctions include: CN I (anosmia); CN VII (facial palsy); CN IX/X (swallowing problems, reflux, and drooling); CN VIII (sensorineural hearing loss). Minor criterion, which are less specific to CHARGE, includes genital hypoplasia (70-80%), developmental delay (100%), orofacial cleft (15-20%), distinct facial patterns (70-80%), and altered palmar creases (50%). 22 Diagnosis: At least four of these abnormalities should be present if a child is to be diagnosed as having CHARGE Association. In any child suspected to have CHARGE, cardiorespiratory, ophthalmological, and audiological evaluations may be performed as well as abdominal ultrasound and chromosome evaluation. Treatment: Many of the structural anomalies can be surgically corrected. Due to developmental delay most children with CHARGE will not be mobile until 20-25 months and will not ambulate independently until 35-57 months making early intervention crucial. Many will demonstrate a "five-point" crawl with their head down dragging on the floor. Because of the developmental delay, early intervention would play an important role in mobility, improving static postures, transitioning towards ambulation, and teaching self care skills. 22 Prognosis: Choanal atresia is life-threatening because young infants cannot establish the habit of breathing through their mouths. Prognosis is based on the severity of factors. For example, a severe case with major developmental delay and growth retardation has a poor prognosis while one with surgically correctable malformations may lead a happy, healthy life. Goldenhar Syndrome Goldenhar syndrome is variant of Hemifacial Microsomia. It's severity can vary and the effects can be unilateral or bilateral. The physical manifestations of this disorder match those of Hemifacial Microsomia with the addition of epibulbar dermoids which are benign tumors located just inside the opening of the eye or the eyeballs. Characteristics: The physical characteristics of Goldenhar syndrome include: Unilateral or Bilateral underdevelopment of the Mandible Unilateral or Bilateral Microtia Unilateral or Bilateral reduction in size and flattening of the Maxilla (upper jaw) Narrowing of the opening of the eye Epibulbar Dermoids which can cause problems with vision. The lack of growth and facial asymmetry of Hemifacial Microsomia are accompanied by epibulbar dermoids. Causes: The origin of this syndrome is thought to be a vascular accident in the fetus. This accident causes the blood supply to be cut off and production of blood clots in the area of those tissues which will develop into the structures of the ear and lower jaw. The amount of damage caused by the vascular accident is directly related to the period of development in which it occurs as well as the degree of tissue destruction that takes place. Since it is not genetically linked, most cases of Goldenhar syndrome are sporadic and the risk of an effected individual to have an affected child is minimal. Expectations: Due to the delayed growth and development of the effected areas, the effects of this syndrome will be more evident as the child grows. The lack of the development of the upper and lower jaws can cause breathing problems as well as a dental malocclusion which will need to be addressed surgically and orthodontically. Treatment: For these patients, treatment generally requires the expertise of both a craniofacial surgeon and an orthodontist with experience with these problems. The jaw deformity is addressed as early as 3 years of age if the mandibular retrusion is severe enough to cause airway difficulty. This jaw reconstruction can be achieved by extending the mandible with a rib graft or with the utilization of a distraction device to "stretch" the bone. The best approach to reconstructing the jaw is determined by the surgeon and is specific for each patient. If it is needed, ear reconstruction is performed in four stages and usually begin at the age of six years. Throughout life, these patients must maintain adequate dental occlusion through ongoing orthodontic treatment.