Pain
advertisement
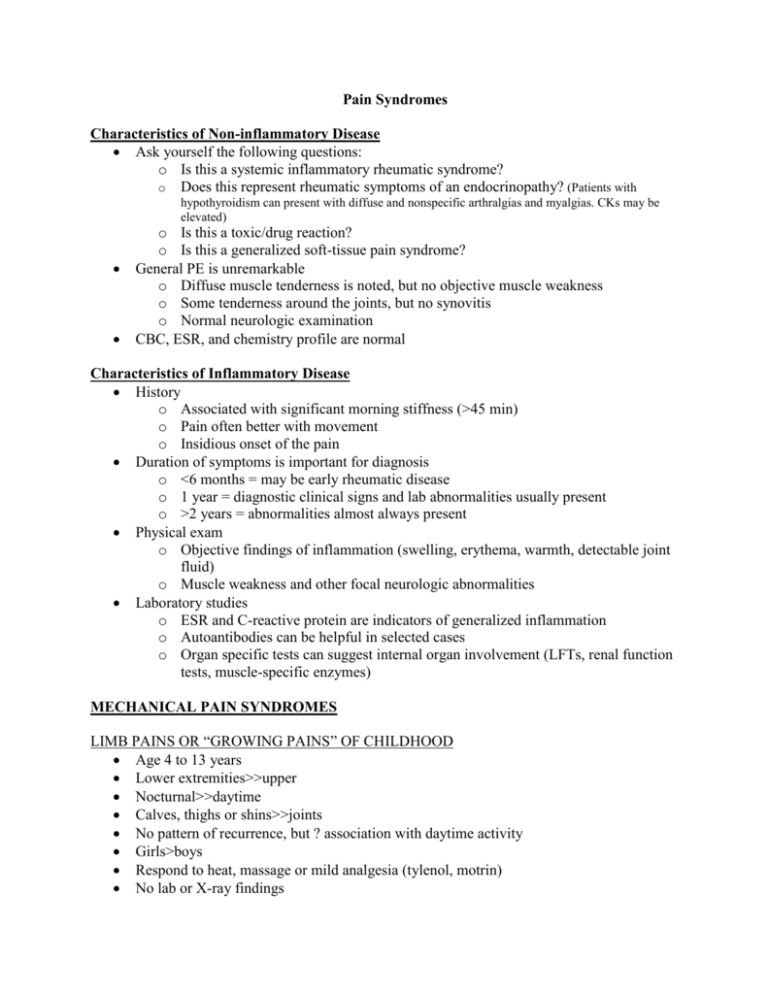
Pain Syndromes Characteristics of Non-inflammatory Disease Ask yourself the following questions: o Is this a systemic inflammatory rheumatic syndrome? o Does this represent rheumatic symptoms of an endocrinopathy? (Patients with hypothyroidism can present with diffuse and nonspecific arthralgias and myalgias. CKs may be elevated) o Is this a toxic/drug reaction? o Is this a generalized soft-tissue pain syndrome? General PE is unremarkable o Diffuse muscle tenderness is noted, but no objective muscle weakness o Some tenderness around the joints, but no synovitis o Normal neurologic examination CBC, ESR, and chemistry profile are normal Characteristics of Inflammatory Disease History o Associated with significant morning stiffness (>45 min) o Pain often better with movement o Insidious onset of the pain Duration of symptoms is important for diagnosis o <6 months = may be early rheumatic disease o 1 year = diagnostic clinical signs and lab abnormalities usually present o >2 years = abnormalities almost always present Physical exam o Objective findings of inflammation (swelling, erythema, warmth, detectable joint fluid) o Muscle weakness and other focal neurologic abnormalities Laboratory studies o ESR and C-reactive protein are indicators of generalized inflammation o Autoantibodies can be helpful in selected cases o Organ specific tests can suggest internal organ involvement (LFTs, renal function tests, muscle-specific enzymes) MECHANICAL PAIN SYNDROMES LIMB PAINS OR “GROWING PAINS” OF CHILDHOOD Age 4 to 13 years Lower extremities>>upper Nocturnal>>daytime Calves, thighs or shins>>joints No pattern of recurrence, but ? association with daytime activity Girls>boys Respond to heat, massage or mild analgesia (tylenol, motrin) No lab or X-ray findings Fine in morning PATELLO-FEMORAL SYNDROME Female>male Age at onset 11-13 years Knee pain--grating, catching, instability Pain increased with descending stairs, squatting, kneeling, running Unable to sit for long periods without extending knee Physical findings--crepitance, +patellar apprehension test, patellar compression test BENIGN HYPERMOBILITY SYNDROME • Carter and Wilkinson Score – Extend little finger > 90 degrees (1 point each) – Bring back thumb parallel to touch forearm – Hyperextend elbow > 10 degrees – Hyperextend knee > 10 degrees – Touch floor with flat of hands, legs straight • Score > 6 equals hypermobility (max = 9) Up to 10% of normal population Arthralgias common Injuries common (dislocation of affected joints, back pain, meniscal and tendon injuries) Increased incidence of mitral valve prolapse Genetically determined ?Generalized laxity of tissues? Ehlers-Danlos syndrome type 3? CENTRALLY MEDIATED PAIN SYNDROMES/ GENERALIZED SOFT TISSUE PAIN SYNDROMES Evidence for central desensitization: Neurophysiologic testing reveals abnormal nociceptive processing Dysautonomia Increased (3X) substance P in CSF Regional modulation in CNS blood flow in hemithalami, caudate nuclei, pontine tegmentum Abnormal summation of pain signals “wind-up” Abnormal somatomedin, prolactin and cortisol stress response Fibromyalgia, Myofascial pain syndrome, Irritable bowel syndrome, Migraines, Tension headaches, TMJ disorder, Irritable bladder, interstitial cystitis all related as a centrally mediated pain syndrome MYOFASCIAL PAIN Localized, muscular pain No generalized aching, stiffness of fatigue Responds to local therapy COMPLEX REGIONAL PAIN SYNDROME (CRPS) Age: prepubertal through early to mid adolescence Females>males One or more extremities may be involved Diagnosis requires the presence of physical abnormalities including temperature and color changes or swelling (autonomic signs) Diffuse exquisite pain to light touch (allodynia) and severe dysfunction are hallmarks Frequently see high-achieving, perfectionistic children with close (enmeshed?) family units FIBROMYALGIA SYNDROME Widespread musculoskeletal pain, aching, stiffness Decreased pain threshold and tolerance May have tenderness in specific regions (tender points) Associated fatigue, sleep, somatic complaints No objective inflammation seen on physical examination Normal laboratory findings Occurs in prepubertal, pubertal and adolescents Females>>>males Parasthesias, headaches, depression and anxiety Treatment o active physical therapy/ conditioning exercises- to increase function in spite of pain not to eliminate pain. o NSAIDs, amitriptyline, but duration of response to pharmacological agents is usually limited Fibromyalgia Tender Points 11 out of 18 tender points Control points – thumb-nail, mid-forearm, and forehead MAJOR DEPRESSION WITH MUSULOSKELETAL PAIN Significant depression is seen in o 49% of patients with chronic soft-tissue pain o 37% of patients with rheumatoid arthritis o 33% of patients with osteoarthritis Depression is associated with increased pain levels in arthritis Depression is more prevalent with loss of valued activities SOMATOFORM PAIN DISORDERS Chronic pain that cannot be explained by a known general medical condition These nonintentional symptoms cause significant distress and impairment of social, occupational, and functional activities Psychological factors play a role in the onset, severity, or maintenance of the pain Somatoform disorders are commonly seen (15%) and nonrecognized (71%) in the primary-care setting Have a high index of suspicion for the presence of amplified musculoskeletal pain especially in: Adolescent girls who are mature beyond years, accomplished, perfectionistic pleaser Prolonged school absence due to pain Marked dysfunction Pain is continuing to worsen Normal examination except pain (no enthesitis or arthritis, normal neurological exam) Localized or widespread pain on examination o Allodynia (variable border) o Autonomic signs o Incongruent affect (la belle indifference) o Multiple painful points o Nonorganic back signs Failure of all prior therapies Once an amplified musculoskeletal pain syndrome is recognized Acknowledge the pain and explain that it is amplified, not indicative of underlying damage or disease Stop further medical investigations and stop medications Restore function o Aerobic exercise up to 5 h/day of intense tx focused on functional activities that may take 2-3 weeks o If allodynia is present, desensitize with tactile stimulation o Resume full school attendance o Resume social and recreational activities Have psychological dynamics evaluated and treated: stress management, coping skills Key Points Early diagnosis—the pediatrician’s job Confidence of diagnosis Clear, concrete plan of treatment Patient/family/treating team/payer in full support of plan