essential - British Society of Gastroenterology
advertisement
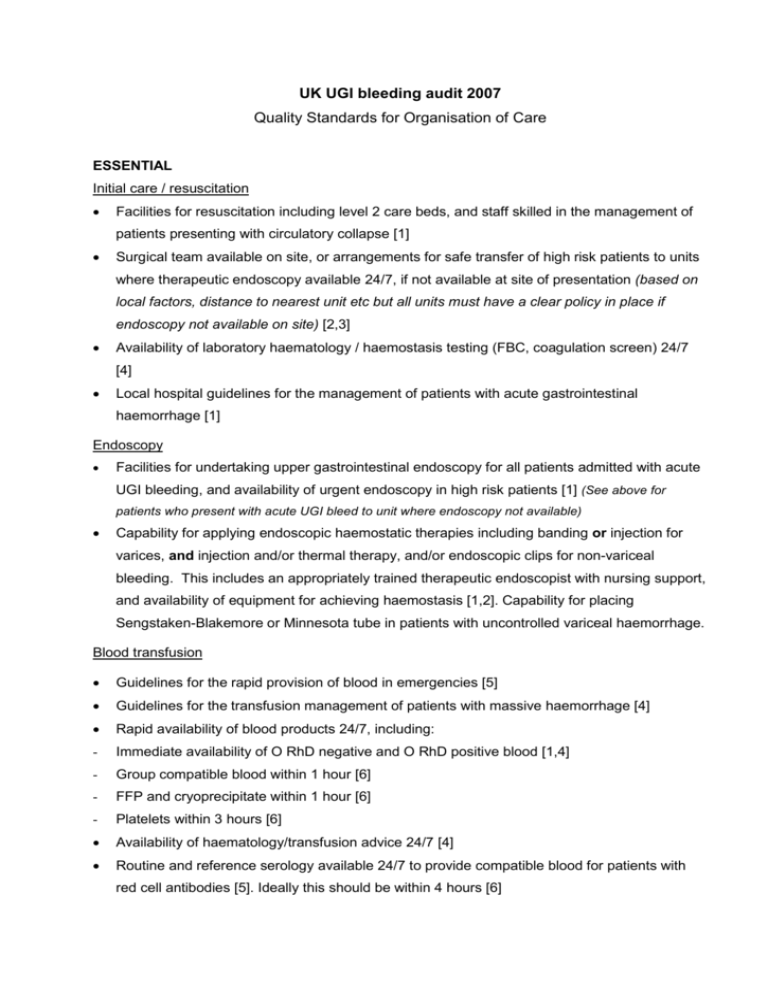
UK UGI bleeding audit 2007 Quality Standards for Organisation of Care ESSENTIAL Initial care / resuscitation Facilities for resuscitation including level 2 care beds, and staff skilled in the management of patients presenting with circulatory collapse [1] Surgical team available on site, or arrangements for safe transfer of high risk patients to units where therapeutic endoscopy available 24/7, if not available at site of presentation (based on local factors, distance to nearest unit etc but all units must have a clear policy in place if endoscopy not available on site) [2,3] Availability of laboratory haematology / haemostasis testing (FBC, coagulation screen) 24/7 [4] Local hospital guidelines for the management of patients with acute gastrointestinal haemorrhage [1] Endoscopy Facilities for undertaking upper gastrointestinal endoscopy for all patients admitted with acute UGI bleeding, and availability of urgent endoscopy in high risk patients [1] (See above for patients who present with acute UGI bleed to unit where endoscopy not available) Capability for applying endoscopic haemostatic therapies including banding or injection for varices, and injection and/or thermal therapy, and/or endoscopic clips for non-variceal bleeding. This includes an appropriately trained therapeutic endoscopist with nursing support, and availability of equipment for achieving haemostasis [1,2]. Capability for placing Sengstaken-Blakemore or Minnesota tube in patients with uncontrolled variceal haemorrhage. Blood transfusion Guidelines for the rapid provision of blood in emergencies [5] Guidelines for the transfusion management of patients with massive haemorrhage [4] Rapid availability of blood products 24/7, including: - Immediate availability of O RhD negative and O RhD positive blood [1,4] - Group compatible blood within 1 hour [6] - FFP and cryoprecipitate within 1 hour [6] - Platelets within 3 hours [6] Availability of haematology/transfusion advice 24/7 [4] Routine and reference serology available 24/7 to provide compatible blood for patients with red cell antibodies [5]. Ideally this should be within 4 hours [6] DESIRABLE Audit of local outcomes of emergency admission for UGI bleeding with review of outcomes [7] Participation in national / UK audit of UGI bleeding [7] Surgical team available on site Availability of TIPSS either in the unit or following reasonable transfer Availability of endoscopy for patients with acute UGI bleeding on daily endoscopy list, for those who do not require out of hours endoscopy [8] Nurses trained in the use of therapeutic endoscopic techniques to be available for all emergency endoscopy A policy should be available for warfarin reversal [9] Trainees to be under direct supervision for emergency endoscopy until passed as competent at interventional techniques for endoscopic haemostasis [10] References 1. BSG Endoscopy Committee. Non-variceal upper gastrointestinal haemorrhage: guidelines. Gut 2002; 51: iv1-iv6 2. Care of patients with gastrointestinal disorders in the United Kingdom, a strategy for the future, BSG 2006 3. Out of hours gastroenterology – A position paper. 2007 4. British Committee for Standards in Haematology. Guidelines on the management of massive blood loss. Br J Haematol 2006; 135: 634-641 5. British Committee for standards in haematology. Guidelines for compatibility procedures in blood transfusion laboratories. Transfusion Medicine; 2004 14: 59-73 6. Consensus opinion (Professor M Murphy, Dr S Allard, Dr A Copplestone, Dr J Wallis) 7. Good medical practice for physicians. RCP London 2004 : 8. BSG working party report. Provision of endoscopy related services in district general hospitals. 2001 9. T. P. Baglin, D. M. Keeling, H. G. Watson, the British Committee for Standards in Haematology (2006) Guidelines on oral anticoagulation (warfarin): third edition - 2005 update British Journal of Haematology 132 (3), 277–285. 10. JAG guidelines for the training appraisal and assessment of trainees in gastrointestinal endoscopy. 2004