Upper GI Bleeding
advertisement
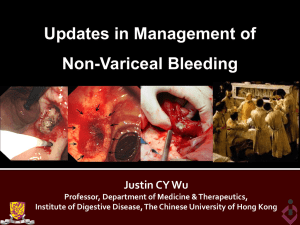
Upper GI Bleeding Dr.Vimalan Ambikaipaker Gastro Advanced trainee JHH “blood and guts”” Upper GIH Potential life threatening problem Upper GIT is 4times more common than Lower GIT Most common course – peptic ulcer 80% stop bleeding Increasing age and co-morbidity increases mortality Important to indentify patients with low probability of rebleeding from patients with a high probability of rebleeding. Upper GI anatomy Lower GI anatomy Aetiology Peptic ulcer disease 35-50% Duodenal ulcers 25% Gastric Ulcer 20% Gastroduodenal erosions 8-15% esophagitis 5-15% Esophageal varices 5-10% Malignancy 1% Aetiology - rare Dieulafoy’s lesions Angiodysplasia Haemobilia Pancreatic pseudocyst and pseudo aneursym Bleeding diathesis Ehlers-danlos syndrome Gastric antral vascular ectasia Rendu-osler-weber-syndrome Pseudoxanthoma elasticum NVUGIB Consensus Guidelines A - Resuscitation, risk assessment and pre-endoscopy management B - Endoscopic management C – Pharmacological management D – Non-endoscopic, non- meds in hospital treatment E – Medication review, ASA, Clopidrogel, warfarin dabigratan (Pradaxa) and NSAIDS. F – Discharge planning and Communication to GP G – Need for gastro liaison service to be involved A - Resuscitation, risk assessment and pre-endoscopy management History taking >vomiting large amounts of red blood (active bleeding) >Coffee-ground vomitus (older-non active bleeding) > History melaena (black, tarry, smelly, difficulty to flush and iron tablets) >Haematochezia in rectum ? Bowel obstruction Weight lost, diffuse or localised abdominal, retching History Co- morbidity and risk factors GERD, Peptic ulcers ,alcohol intake ,bleeding before Liver cirrhosis Liver malignancy Haematological disease – Low platelets, bleeding diathesis Abdominal Aneurysm Lung disease ,OSA, sedation issues Medications Aspirin Clexane Clopidrogel Dabigratan (pradaxa) Warfarin NSAIDS Steroids Iron tablets and bismuth Sedation issues – opiods,Marijuana,Methadone Examination Vital signs Signs of chronic liver disease Decompensated liver disease Acute abdomen Encephalopathy PR rectal examination A - Resuscitation, risk assessment and pre-endoscopy management ABC 2 IV lines FBC,U/E, LFT, Coags, group and save/ crossmatch,ECG Need for FFP, Prothrombin X and platelets and correct coagulopathy(<2.5) IV fluid resuscitation Blood transfusion (Hb<70) Imaging CXR and AXR IV PPI Infusion and consider OCTREOTIDE infusion if suspect varices bleed. Reduce risk of aspiration , IV maxolon or IV erythromycin) Aims- BP >100mmHg,HR<100bpm,HCT>24%,Platelets>50 Correct INR,? ICU/Haematologist Urgent endoscopy Contact gastroenterologist on call (Urgency made clearly to the consultant) A - Resuscitation, risk assessment and pre-endoscopy management PPI Infusion Before endoscopy, accelerate the resolution of endoscopic stigmata of bleeding ulcers and reduce the need for endoscopic therapy but should not delay endoscopy. Does not result in improved clinical outcomes such as decrease transfusions, rebleeding, surgery or death. PPI initiated after endoscopic diagnosis of peptic ulcer bleed significantly reduces rebleeding and surgery rates Effects are more pronounced in Asian compared to with nonAsian populations Continue IV infusion for 3days Octreotide infusion Reduces rebleeding rates similar to endoscopic sclerotherapy Continue infusion for 5days Risk assessment Rockall Score Factors – Age,shock,C0-mobidity,Diagnosis Major stigmata – blood in GI tract, adherent clot, visible and spurting vessel * * * * rebleeding Longer stay in hospital Rescoping But always use clinical judgement How to provoke homicidal rage in the Gastroenterologist Tell them the patient is “haemodynamically stable” Don’t tell them anything but fast the patient “just in case” Insert a venous cannula of 24 gauge or less Do not cross match Start a PPI infusion without any plans for an endoscopy Perform Faecal Occult Blood test Don’t call them early Post endoscopy – no blood or stool chart monitoring Fail to identify rebleeding in post endoscopy patients God gave you hands – use the one finger though!!! What to the gastroenterologist need to know Accurate history Co-morbidity Medication and sedation issues Physical examination and PR findings Resuscitation Plan and monitoring plan Retrieval plan Discuss time for endoscopy or the need to be done in theatre Booking of endoscopy unit and theatre nurse in charge is aware. Red slip!! and consent Gastroenterologist needs to know early B- Endoscopic management Early endoscopy , within 24hrs More urgent (vomiting bright red blood or haematochezia Endoscopic hemostatic tx is not indicated for patients with low-risk stigmata (clean based ulcer, or a non-protuberant pigmented dot in an ulcer bed) Finding of clot in ulcer bed warrants target irrigation an attempt dislodgement and with an appropriate treatment of underlying lesion (adrenaline with APC) or PPI might be enough. Endoscopic hemostatic tx is indicated for patients with highrisk stigmata. Combination – epinephrine with either (APC, Clip or sclerosant injection) If rebleed – need second look Need for surgical team involvement Esophagus Esophagus Stomach Duodenum Video clip Endoscopic haemostatic Treatment Esophageal varices Stomach Varices Video clip Video clip D- non-endoscopic, non meds in hospital treatment Rockall score <3 with low risk of bleeding or death can be considered for early discharge. Full Rockwall score >3 indicates patients needs further close observation as an in patient. Careful monitoring needed post endoscopy Need for re-endoscopy If patient is at low-risk after endoscopy can be fed after 24hrs If patient having undergone endoscopic haemostasis for high risk stigmata should be hospitalised for at least 72hrs thereafter Bleeding peptic ulcer and duodenal ulcer – should have testing for H. Pylori but not when acute bleeding. C14 urea breath test, serology- should receive eradication with confirmation of eradication(2weeks later) E-Mediation review In patients with prior ulcer bleed who require an NSAID, it should be recognized that treatment with traditional NSAID plus PPI or a COX-2 alone still associated with clinically important risk of bleeding In patients with prior ulcer bleeding who require NSAID the combination of PPI and cox-2 is recommended to reduce the risk of recurrent bleeding from that of cox-2 alone. Inpatients receiving low-dose ASA who develop an acute ulcer bleed, ASA should be started as soon as the risk of Cardiovascular complication is thought to outweigh the risk of bleeding. In patients with a prior bleed who require CVA prophylaxis it should be recognized that clopidrogel alone has a higher risk of rebleeding vs ASA and PPI A good discharge summary with follow-up plan. Discuss with GP before discharge. If plan for re-scoping don’t forget RFA Resident of the team Clinical Pearls History, clinical exam, sedation issues and resuscitation Please take note of the operative report (Endoscribe/ ProvationMD database) Post-operative plan High risk patients – Potential rebleeding Medication – to be restarted/ withheld Discharge planning and follow-up Discharge summary – Upper GIH - Cause identified * where is the lesion? - Treatment, risk of rebleed,variceal banding - medication update - Further follow-up…. - Talk to the GP – Ensure updated medication list and H.pylori testing Outstanding pathology results In the last 12months Inappropriate resuscitation – PPI infusion, IV fluids, NBM Nursing Monitoring – Prolonged hypotension – No review Bright PR bleeding noted by family, nursing staff, medical RMO and Registrar aware but gastroenterologist not informed ED noted Haematemesis and malaena but discharge home without endoscopy Peripheral shutdown, difficult access, call made to ICU for cannula assistance. Metcall Vs consult Delay in referral made to gastroenterologist for patient with HB 56! No discussion with operation suite for add on emergency list NO per-rectal examination- carried information from triage, patient, ED staff. PLEASE DO IT YOURSELF. Summary A good history and proper clinical examination Per-rectal examination Resuscitate the patient, risk assessment Plan for endoscopy discussed with gastroenterologist Medical registrar/AT to be aware of the patient Most GIH will stop spontaneously however, only endoscopy will identify which lesions will not therefore: never assume that a lesion is controlled without endoscopy Thank you Course notes from the 4th Annual Westmead Endoscopy Symposium,3rd and 4th March 2011. Dr.Gurvinder rull- Article on Upper GIH Practical gastroenterology and Hepatology- Nicholas J.talley,Kemeth R.devault,David E.Fleischer Prof. Aidan Foy slides.