Laryngology seminar
advertisement
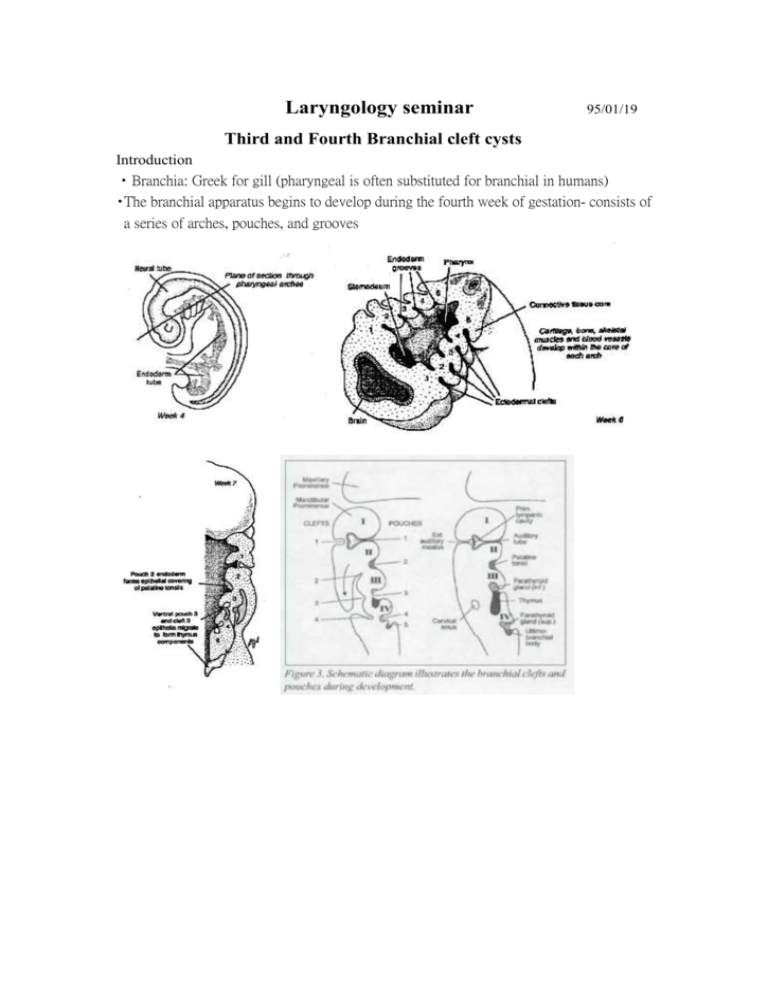
Laryngology seminar 95/01/19 Third and Fourth Branchial cleft cysts Introduction •Branchia: Greek for gill (pharyngeal is often substituted for branchial in humans) •The branchial apparatus begins to develop during the fourth week of gestation- consists of a series of arches, pouches, and grooves •Branchial anomalies may result from abnormal persistence of branchial apparatus remnants- cyst, sinus, or fistula •von Baer, in 1827: the earliest description of the branchial apparatus •von Ascherson, in 1832: perhaps the earliest recognition of branchial cleft anomalies •Heusanger, in 1864: the term branchial fistula is reported (cysts of the lateral neck were being ascribed to branchial origin) First branchial cleft anomalies •Account for 8% to 10% of all branchial cleft and pouch anomalies •Classification by Arnot in 1971 (based on the anatomic location) - Type I: a. lies in the lower pole of the parotid gland, often closely associated with the lower branches of facial nerve b. passing between the mandible and the stylohyoid ligment and lying anterior to the carotid artery - Type II: a. lying anterior to and below the angle of the mandible b. passing inferior to the parotid gland and ending at the bony-cartilaginous junction of the external auditory canal •Classification by Work in 1972 (based on the embryonic derivation) _ Type I: a. ectodermal in origin, b. run parallel to the external auditory canal, involving parotid tissue but usually passing superior to the main trunk of the facial nerve - Type II: a. ectodermal and mesodermal in origin b. located within the substance of the parotid gland •D.D.: inflammatory adenitis, dermoid cysts, cystic hygoma, lipoma, neurofibroma, hemangioma, sarcoidosis, metastatic carcinoma, lymphoma, and primary parotid tumor •Surgery - after acute infection has resolved a standard cervico-mastoid-facial parotidectomy incision with formal dissection of the facial nerve and superficial parotidectomy (for facial nerve preservation and complete removal of the anomalous tract) Second branchial cleft and pouch anomalies •The most commonly encountered branchial defects (between 67% and 93%) •Pathway - deeply to second arch, superficially to third arch - from external opening in the mid- or lower neck along the line of the anterior SCM platysma m. superiorly along the carotid sheath the level of hyoid bone over the hypoglossal n. between the internal and external carotid arteries and over the glossopharyngeal n. deep to stylohyoid ligament internal opening within the tonsillar fossa - most commonly presents just lateral to the internal jugular vein at the level of the carotid bifurcation •Recurrent unilateral tonsillitis or parapharyngeal space abscess •Symptoms: progressive swelling, pain, infection, pressure symptoms such as dyspnea and dysphagia •D/D: metastatic malignant neoplasms, tuberculous cervical adenitis, cystic hygroma, hemangioma, dermoid cysts, primary lymphoma, carotid body tumors and carotid aneurysms, aberrant thyroid nodules, suppurative cervical lymph nodes, neurofibromas, lipomas, thyroglossal duct cysts, cystic tumors in the tail of the parotid gland, accessory thymic remanants, and bronchiogenic carcinoma •Surgery - complete surgical excision with preservation of surrounding neurovascular structures Stepladder technique for second branchial sinuses and fistulas Functional neck dissection has been suggested as an appropriate treatment for recurrent second branchial remnants Third and fourth branchial pouch anomalies •Third and fourth branchial clefts and pouches are relatively uncommon - third branchial anomalies: 2%-8% fourth branchial anomalies: 1%-2% the distinction between third and fourth branchial pouch sinuses remained controvertial a. common piriform fossa origin and similar clinical presentation as a neck or thyroid abscess b. inflammatory neck mass requiring repeated incision and drainage, recurrent deep neck space infection, and airway obstruction •First English-language literature to suggest that a sinus tract originating from the piriform fossa might represent a branchial anomaly (4th)- case reports in 1972 by Sandborn and Shafer and in 1973 by Tucker and Skolnick •In 1979, Takai et al.: causative association of a persistent sinus tract of the piriform fossa with recurrent acute suppurative thryoiditis a smattering of case reports identifying third and fourth branchial pouch anomalies and linking them to recurrent cervical abscesses and thyroiditis •Pathway of third branchial cleft and pouch fistula - deep to third arch structures and superficial to fourth arch structures begin at the piriform fossa of the hypopharynx pierce the thyrohyoid membrane passing cranial to the superior laryngeal nerve pass superficial to the hypoglossal nerve deep to the glossopharyngeal nerve and the internal carotid artery pierce the platysma •Pathway of fourth branchial pouch abnormality ( by Liston in 1981) - Between the mesodermal derivatives of the fourth and sixth arches - Begin at the piriform fossa exit the larynx near the cricothyroid joint pass between the superior and recurrent laryngeal nerve descend alongside the trachea and esophagus 1. left side: into the mediastinum to the level of aorta ( loop around it ) 2. right side: to the level of subclavian artery ascend the neck (posterior to the internal and common carotid artery) pass superior to the hypoglossal nerve exit to SCM m. in the lower neck •Key importance in distinguishing a third from a fourth arch sinus ( only on surgical exploration): - the relationship of the anomalous tract to the superior and recurrent laryngeal nerves th 4 arch anomaly should be caudal to the cricothyroid muscle and thyroid cartilage and external to the recurrent laryngeal nerve - No relation with the carotid sheath as is present in second and third arch defects •Fourth branchial pouch anomalies: - most were diagnosed in childhood - 97% occur on the left side - A slight female preponderance - Two distinct clinical presentations: - a. In neonates: as lateral neck cysts or abscesses with associated obstructive airway symptoms b. In children, adolescents, and occasionally adults: recurrent lateral cervical abscesses or recurrent acute suppurative thyroiditis •Some authors have recommended an immediate search for an internal pharyngeal sinus, including a barium swallow and computed tomography scan, after a child’s first episode of acute thryoiditis •Most effective method for determining the presence of a sinus tract of the piriform fossa: direct laryngoscopy •The preferred treatment for third and fourth branchial nomalies: complete surgical excision, including resection of the piriform fossa attachment, (partial or total thyroid lobectomy often needed for fourth branchial pouch sinuses) •cannulated to aid in identification: lacrimal probe or Fogarty balloon catheter •Most fourth branchial pouch sinuses (surgically): begin at the piriform fossa apex and terminate either in scar tissue within the perithyroid space or in the substance of the thyroid gland itself •Because of previous infection and scar tissue, dissections can be difficult •J.A. Jordan et al. in 1998: endoscopic cauterization for treatment of fourth branchial cleft sinuses - total 7 cases: 1 of 7 cases, electrocautery and sutures placed with endoscopy to close the sinus tract; 6 of 7 cases, the wound was allowed to heal without suturing - 4 of 7 patients have been followed up for more than 18 months •D.J. Verret et al. in 2004: 10 children with fourth branchial cleft sinuses treated with endoscopic cauterization between 1995 and 2002 ( 2: recurrent neck abscess, 6: abscess of the left side of the neck, 1: suppurative thyroiditis, 1: neck abscess after open excision of a branchial cleft sinus) - 7 of 10 cases showed no recurrence with an average follow-up of 3 years - 3 of 10 cases were unavailable for follow-up ( no additional admission at medical records) •D/D: lymphadenitis associated with URI, cystic hygroma, atypical thyroglossal duct remnants, thymic cysts, ectopic thyroid tissue, tuberculous adenitis, lymphoma, hemangioma, and metastatic malignant neoplasms Reference 1. Diagnostic Imaging Head and Neck, Harnsberger, IV-1-6 to IV-1-18 2. Mendell DL. Head and neck anomalies related to the branchial apparatus. Otolaryngol Clin North Am. 2000: 33; 1309-1332 3. Link TD, Bite U. Kasperbauer JL. Hamer SG, Fourth branchial pouch sinus: a diagnostic challenge. Plast Reconstr Surg. 2001: 108; 695-701 4. J.A. Jordan, J.E. graves, S.C. Manning, J.E. McClay, M.J. Biavati. Endoscoic cauterization for treatment of fourth branchial cleft sinuses, Arch. Otolaryngol. Head Neck Surg. 124 (9) (1998) 1021-1024 5. D.J. Verret, J McClay, A. Murray, M. Biavati, O. Brown. Endoscopic cauterization of fourth branchial cleft sinus tracts 6. Sandborn WD. Snafer AD. A branchail cleft cyst of fourth pouch origin. J Pediatr Surg. 1972; 7:82 7. H.M. Tucker, M.L. Skolnick, Fourth branchial cleft (pharyngeal pouch) remnant, Trans. Am. Acad. Othalmol. Oto 77 (1973) 368-371 8. A. Jeyakumar, A. Hengerer, Various presentations of fourth branchial pouch anomalies, Ear, Nose & Throat Journal, Sep. 2004, 640-644 9. http://cats.med.uvm.edu/cats_teachingmod/radiology/radiology_html/teaching/radio_ad ult/branchial_cleft_cyst/branchial_cleft_cyst_1.html 10. http://www.med.howard.edu/anatomy/gas/wk7/Lecture%2024.htm