Prophylactic Antibiotics in Surgery
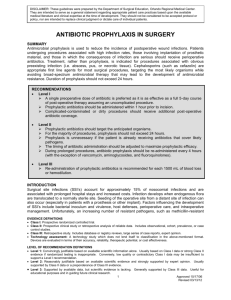
advertisement
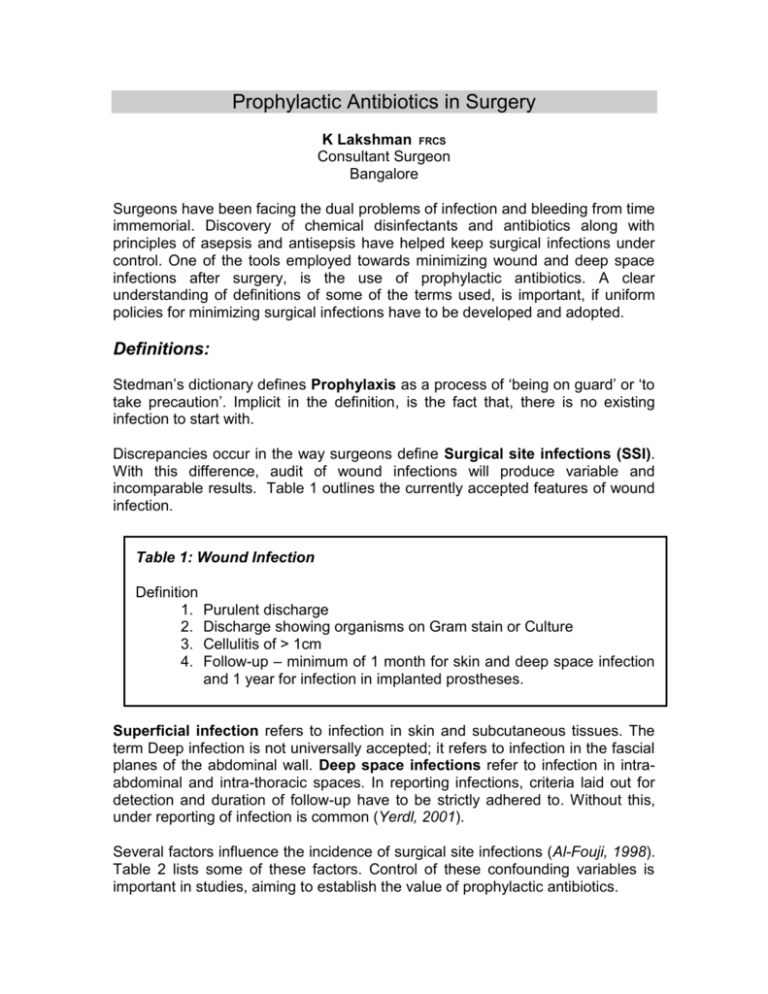
Prophylactic Antibiotics in Surgery K Lakshman FRCS Consultant Surgeon Bangalore Surgeons have been facing the dual problems of infection and bleeding from time immemorial. Discovery of chemical disinfectants and antibiotics along with principles of asepsis and antisepsis have helped keep surgical infections under control. One of the tools employed towards minimizing wound and deep space infections after surgery, is the use of prophylactic antibiotics. A clear understanding of definitions of some of the terms used, is important, if uniform policies for minimizing surgical infections have to be developed and adopted. Definitions: Stedman’s dictionary defines Prophylaxis as a process of ‘being on guard’ or ‘to take precaution’. Implicit in the definition, is the fact that, there is no existing infection to start with. Discrepancies occur in the way surgeons define Surgical site infections (SSI). With this difference, audit of wound infections will produce variable and incomparable results. Table 1 outlines the currently accepted features of wound infection. Table 1: Wound Infection Definition 1. 2. 3. 4. Purulent discharge Discharge showing organisms on Gram stain or Culture Cellulitis of > 1cm Follow-up – minimum of 1 month for skin and deep space infection and 1 year for infection in implanted prostheses. Superficial infection refers to infection in skin and subcutaneous tissues. The term Deep infection is not universally accepted; it refers to infection in the fascial planes of the abdominal wall. Deep space infections refer to infection in intraabdominal and intra-thoracic spaces. In reporting infections, criteria laid out for detection and duration of follow-up have to be strictly adhered to. Without this, under reporting of infection is common (Yerdl, 2001). Several factors influence the incidence of surgical site infections (Al-Fouji, 1998). Table 2 lists some of these factors. Control of these confounding variables is important in studies, aiming to establish the value of prophylactic antibiotics. Table 2: Factors influencing SSIs. Class of surgery Co-morbid conditions ASA grading Shaving Skin preparation Duration of surgery Table 3: Class of Procedure Clean Hernia repair Clean contaminated Biliary tract, Stomach Contaminated Gross spillage, Bowel Resection The degree of contamination at the time of surgery is a significant factor in the causation of SSI. Wounds are classified as clean, clean-contaminated, contaminated or dirty, depending on the estimated degree of contamination (Table 3). Dirty wounds have gross faecal or purulent material contamination; use of antibiotics in this situation is treatment of established infection, and not strictly, prophylaxis. It is universally accepted that prophylaxis is used in cleancontaminated and contaminated operations. Clean operations with implanted material also attract prophylaxis. Its use in clean operations without implanted material is not universally accepted. The low incidence of infection without antibiotics in this group of patients and the unfavourable cost-benefit ratio, have lead to this controversy. Principles of Prophylaxis: Principles of prophylaxis address the selection of the antibiotic to be used and the mode and time of administration of the antibiotic (Dunn DL, 2001). Clearly, the cost–benefit ratio, in terms of the cost of the antibiotic and the ‘cost’ in side effects like anaphylaxis, gastro-intestinal disturbance (Harbarth S, 2001), bone marrow suppression and hepatic and renal toxicity, must weigh in favour of the antibiotic. The first 2-4 hours after making the surgical incision form the ‘golden period’ for prophylaxis. It is important that blood levels of the antibiotic are above minimum inhibitory levels from about 10 minutes before incision is made to about 4 hours after the completion of the operation. If the surgery lasts longer than four hours, it would be prudent to repeat the dose of the antibiotic. Contaminating organisms are endogenous; from the patient himself/herself. With modern sterilization methods, exogenous contamination is almost completely avoided. Endogenous sources include the organisms on the skin and those in the viscera. Knowledge of the ‘normal’ organisms at various sites in the body is essential for choosing the correct antibiotic for prophylaxis. It is important to develop data locally regarding the organisms found at various sites of the body. Extrapolating results of studies from other parts of the world, may lead to the choice of the incorrect drug. Antibiotic levels are maintained for about 12 hours after the surgery; some studies have protocols lasting 24 hours. Certainly any antibiotic course lasting more than 48 hours becomes treatment and cannot be called prophylaxis. Antibiotics commonly used for treatment are avoided as the drugs for prophylaxis; this is to avoid selecting out resistant organisms. Availability, cost, side effects and allergies may preclude use of the first choice antibiotic. It is, thus, important to have a second line drugs ready, to be used if the need arises. Suggested Regimen It is incorrect to specify the use of a single prophylactic antibiotic regime to be applied at different institutions. The principles laid down above have to be followed by each institution, or at the most, institutions within a confined geographical area, in drawing up an antibiotic policy. The following table has been reproduced from a standard surgical textbook (Bailey and Love, 2001) as a general guideline. Source Organism Antibiotic Oesophago-Gastric Enterobact. Enterococci Cefuroxime+ ?Metranidazole Biliary Enterobact. Enterococci Cefuroxime Small Bowel Enterobact. Anaerobes Cefuroxime+ Metranidazole Colorectal Enterobact. Anaerobes Vascular S aureus S epidermidis Aerobic Gm –ve S aureus / Epid Aerobic Gm –ve Anaerobes Cefuroxime+ Metranidazole+ Bowel Prep. Fluclox + Genta Cefuroxime Lower limb amputations Cefuroxime + Metranidazole Special Situations: Most of the operations come under the principles and guidelines outlined above. However certain special situations need a modified approach. These situations include dental procedures in patients with implants (Segreti J, 1999), the asplenic and other immuno-compromised patient (Brigden, 2001) and procedures in the presence of valvular disease of the heart and implanted pace makers(Lee, 2001). Detailed discussion of these situations is outside the purview of this paper. In general, treatment is individualized. Risk stratification of the patient and the procedure is done and decision taken regarding the use of antibiotic. Our Practice: We have been routinely using prophylactic antibiotics in all classes of operations. Our reason in using antibiotics even in clean cases without implants has been to ‘cover’ variations in operating room techniques in different institutions. A single dose of Cefuroxime 750mg IV is given at the time of induction of anaesthesia. This ensures that the drug has been given under direct supervision. Also unexpected delays in starting the surgery will not compromise the time interval between administration of the antibiotic and the making of the incision. A similar IV dose is repeated if the surgery lasts longer than 4 hours. In clean contaminated cases, an additional dose is given 6 hours after the completion of surgery. Metranidazole is added if anaerobes form a part of the potential contaminating flora. If contamination from oral organisms is a possibility, a combination of ampicillin and metranidazole or amoxicillin+Clavulenic acid is used. What is needed in future? We need to generate data regarding the pattern of flora in various centres in our country. Susceptibility pattern of these organisms have to be determined. We also need to have a survey of current practice. It is likely that there are great variations in the use of antibiotics both as prophylaxis and treatment. We need to normalize this by drawing up a uniform policy for the use of antibiotics. Finally we need to monitor how well this policy is being followed. The general experience in this regard, even in developed countries, has been disappointing (Llemand S, 2001). Conclusion: This paper outlines the need for antibiotic prophylaxis. The principles governing such use are explained. The importance of having locally drawn up guidelines for antibiotic use is stressed. Finally, it is emphasized that monitoring the adherence to guidelines and regular audit of SSI are necessary if the goal of good surgical care to our patients, is to be achieved. References: Al-Fouji AR, 1998 in Postgraduate Surgery – A Candidate’s Guide 2nd Edition, Butterworth-Heinmann, pp 180-182 Bailey and Love’s Short Practice of Surgery, 2000, 23rd Edition, Wound Infection, Arnold, pp 93-95 Brigden ML, 2001, Detection, Education and Management of the Asplenic or Hyposplenic Patient, Am Fam Phy, 63(3):499-506 Dunn DL, 2001, Diagnosis and treatment of infection in Surgery – Basic Science and Clinical Evidence, Ed. Norton JA, Bollinger RR, Springer, pp 206-208 Harbarth S, Samore MH, Carmeli Y, 2001, Antibiotic prophylaxis and the risk of Clostridium difficile-associated diarrhea, J Hosp Inf, 48(2):93-7 Lee TH, 2001, Prevention, Evaluation, and Management of Infective Endocarditis: AHA/ACC Guidelines Summary, ACC/AHA Cardiology Guideline Summaries Braunwald: Heart Disease: A Textbook of Cardiovascular Medicine, 6e W. B. Saunders Company, pp 748-749 Llemand S, Albin C, Huc B, 2001, Antibiotic prophylaxis and surgery. Prescription compliance in Franche-Comte with the national reference system, Ann Chir, 126(5); 463-471 (compliance to guidelines) Segreti J, 1999, Is antibiotic prophylaxis necessary for preventing prosthetic device infection?, Inf Dis Clin NA, 13(4): 871-877 Yerdl MA, Emin BA, Sukru D, 2001, Effect of Single-Dose Prophylactic Ampicillin and Sulbactam on Wound Infection After Tension-Free Inguinal Hernia Repair With Polypropylene Mesh, Ann Surg 233(1):