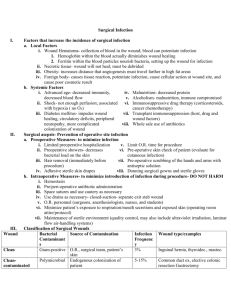
Surgical Infections
advertisement

Surgical Infections MS-3 Surgery Clerkship Lecture Natalia Hannan M.D. 07/05/11 Ignaz Semmelweis 1847 Realized that washing hand with a chlorinated lime solution decreased incidence of newborn death from “puerperal fever’. Joseph Lister • 1883-1897 • British surgeon • Used Carbolic Acid (Phenol) to clean hands, instruments and wipe on surgical wounds drastically decreased infections. Overview • Recognizing Infection • Soft Tissue Infections • Post-operative Infections – Surgical Site Infection – Hospital Acquired Infections • Antibiotic Prophylaxis • Blood Born Pathogens Infection Infection is defined by: 1. Microorganisms in host tissue or the bloodstream 2. Inflammatory response to their presence. Inflammatory Response Localized: – Rubor, Calor, Dolor, Tumor, and functio laesa (loss of function) Systemic: – Systemic Inflammatory Response Syndrome (SIRS) S.I.R.S. Any Two of the Following Criteria 1. 2. 3. 4. Temperature: < 36.0, >38.0 Heart Rate : >90 Respiratory Rate: >20 WBC: <4,000, >12,000 Sepsis Definition: SIRS plus evidence of local or systemic infection. Septic Shock Definition: Sepsis plus end organ hypoprofusion. Mortality of up to 40% Soft Tissue Infections: 1. Cellulitis 2. Abscess 3. Necrotizing Infections Cellulitis Cellulitis Definition: Diffuse infection with severe inflammation of dermal and subcutaneous layers of the skin Diagnosis: Pain, Warmth, Hyperesthesia Treatment: Antibiotics. Common Pathogens: Skin Flora (Streptococcus/Staphylococcus) Abscess Abscess Definition: Infectious accumulation of purulent material (Neutrophils) in a closed cavity Diagnosis: Fluctuant: Moveable and compressible Treatment: Drainage Necrotizing Soft Tissue Infection Necrotizing Soft Tissue Infection Definition: Deep infection of skin and soft tissue that may spread rapidly along facial planes. Diagnosis: Purely Clinical, dishwater discharge, gray tissue, pain out of proportion to examination, bulla, and dark, golden discoloration. Treatment: True Surgical Emergency, Antibiotics Necrotizing Soft Tissue Infection • Common Pathogens – Clostridium – Group A streptococcus – Polymicrobial • Toxic Shock Syndrome – Streptococcus – Staphylococcus Post-Operative Infections • Fever After Surgery • The “Five W’s” – – – – – Wind: Atelectisis Water: UTI Walking: DVT Wonder Drug: Medication Induced Wound: Surgical Site Infection Surgical Site Infections • 3rd most common hospital infection • Incisional – Superficial – Deep • Organ Space – Generalized (peritonitis) – Abscess Types of Surgery Clean CleanContaminated Contaminated Dirty/infected Hernia repair breast biopsy Cholecystectomy planned bowel resection Non-preped bowel resection 1.5% perforation, abscess 5-30% 2-5% 5-30% Host Risk Factors • • • • • • • • Diabetes mellitus Hypoxemia Hypothermia Leukopenia Nicotine (tobacco smoking) Immunosuppression Malnutrition Poor skin hygiene Perioperative Risk Factors • • • • • • • • Operative site shaving Breaks in operative sterile technique Improper antimicrobial prophylaxis Prolonged hypotension Contaminated operating room Poor wound care postoperatively Hyperglycemia Wound closure technique Treatment • Incisional: open surgical wound, antibiotics for cellulitis or sepsis • Deep/Organ space: Source control, antibiotics for sepsis Operative Antibiotic Prophylaxis • Decreases bacterial counts at surgical site • Given within 30 minutes prior to starting surgery • Vancomycin 1-2 hours prior to surgery • Redose for longer surgery • Do not continue beyond 24 hours Other Hospital Acquired Infections 1. Urinary Tract Infection 2. Indwelling Catheter Infection 3. Pneumonia Use/Choice of Antibiotics • Use only when indicated • Start with broad spectrum antibiotics designed to cover likely pathogens • Take cultures when possible • Deescalate spectrum once pathogen is know • Have a plan for duration Occupational Blood Bourne Virus Infections HBV HCV HIV Risk from Needle stick Chemoprophylaxis 30% 2% 0.3% Yes No Yes Vaccine Yes No No