Cranial Nerve Syndrome
advertisement
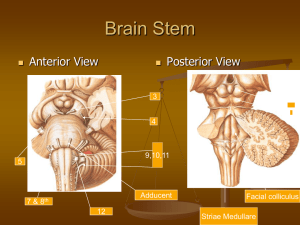
Cranial Nerves Conforming Superior Orbital syndrome (see VI nerve palsy) Cavernous sinus syndrome (see VI nerve palsy) Cerebellar Pontine Angle syndrome o Involvement V1-3 (tinnitus and deafness earliest symptom then vertigo; loss of corneal reflex is the earliest sign) VI VII VIII IX Cerebellar o Causes Tumor Primary o “Acoustic neuromas” – schwannomas of the vestibular o Meningiomas, haemangioblastomsa, medulloblastomas o Choleastoma Secondaries o NPC ( loss of corneal reflex and V2 early) o Lymphoma Aneurysm For bilateral lesions Bilateral “acoustic neuromas” in NF type 2 o Examination Examine CNs ULs for cerebellar signs Proceed to check neck for LNs Look for NF features (café au lait spots, neurofibroma, freckling and Lisch nodules) o Presentation Sir, this patient has righ/left CPA lesion as evidenced by There is no enlarged Cx LNs to suggests secondaries There is also no evidence of NF Possible etiologies includes o Questions What is the CPA? Shallow trangular fossa lying between the cerebellum, lateral pons and the petrous temporal bone Histology? Schawannoma Ix? Imaging – CT/MRI/Angio Audiography ENT to exclude NPC Mx Microsurgical resection Stereotaxic radiosurgery (Cx rate same as surgery) Lateral medullary syndrome o 5 vessels involved (wedge shaped infarction of the lateral aspect of the medulla and the inferior surface of the cerebellum) PICA Vertebral artery (most common artery that is involved) Lateral medullary artery (superior, middle, inferior) o Areas affected Descending sympathetic fibres Ipsilateral Horner’s syndrome Ptosis, meiosis and anhidrosis Spinothalamic tract Contralateral hemi-sensory loss of pain and temperature Descending tract and nucleus of V Ipsilateral loss of pain and temperature of the face Nucleus ambiguus(X) and IX Hoarsenss of voice, dysphagia, hiccups Vestibular nuclei Nystagmus, vertigo, nausea Cerebellar (restiform body of the inferior cerebellar peduncle) Ipsilateral ataxia and gait ataxia o Examination CN examination Go to ULs for loss of pain and temperature and cerebellar Check for AF and DM dermopathy Visual Fields for homonymous hemianopia (posterior circulation) o Sir this patient has right/left LMS as evidenced by State the findings Mention NG Aetiology – infarction affecting the vertebral artery or the PICA, LMA Did not find any xanthelesma or DM dermopathy, or AF Request for BP and asking patient on symptoms of dysphagia Medial medullary syndrome o Triad of XII, medial lemniscus and pyrimidal tract o Ipsilateral wasted tongue, contralateral loss of vibration and propioception and contralateral hemiparesis respectively o Either vertebral artery or lower basilar Bulbar palsy o Bilateral involvement of LMN IX, X, XI and XII o Examination Proceed with CN Do Jaw jerk Requests to examine speech, and gag reflex Requests to examine ULs for fasciculations and dissociated sensory loss o Presentation Patient has bulbar palsy as evidenced by weakness of the soft palate, wasted tongue with fasciculations a/w a nasal voice and a normal or absent jaw jerk o Causes (MGS, NNNP) MND GBS Syringomyelia Poliomyelitis, NPC, neurosyphilis and neurosarcoid Pseudobulbar palsy o Bilateral UMN lesions of the IX, X and XII, V and VII (III/IV and VI are spared) o Examination Proceed with CN Do jaw jerk Request for speech, gag reflex and enquire emotional lability Request for AF, DM dermopathy and xanthelesma Requests for ULs to look for UMNs o Presentation Patient has PBP as evidenced by presence of sluggish palatal movement, small, stiff and spastic tongue a/w brisk jaw jerk with “Donald duck” speech (slow, thick and indistinct) No AF, DM or xanthelasma No evidence of mix UMN and LMN signs to suggest MND No RAPD or INO to suggest multiple sclerosis Possible causes (BMM) Bilateral stroke MND Multiple sclerosis Syringobulbia o See syringomyelia o Extension of syrinx to involve the brainstem o V(descending tract of V), VII, IX, X, XI, XII and Horner’s syndrome o Usually unilateral Jugular foramen syndrome o Involvement of the IX, X, XI (XII maybe affected due to proximity) o Unilateral o Examination CN exams Proceed to check for enlarged Cx LNs And request to assess speech for husky voice and bovine cough o Presentation Sir, this patient has right/left JFS as evidenced by Notice that this patient is on NG No enlarged Cx LNs Possible etiologies includes o Questions Causes Ca of the pharynx (commonest cause), tumor, neurofibroma Basal meningitis Paget’s disease, trauma Thrombosis of the jugular vein IX, X and XI leaves the skull via jugular foramen (between the lateral part of occiput and the petrous part of the temporal bone) XII leaves via the anterior condylar foramen Isolated XI implies injury to XI in the neck eg stab wounds Non-Conforming Myasthenia Gravis (see Myasthenia Gravis) Miller Fisher Syndrome o Variant of Guillain Barre syndrome o Characterise by triad of ophthalmoplegia, ataxia and areflexia o Cs by anti G1Qb antibodies o Rare o Good prognosis with recovery beginning within 1 month of onset and complete recovery within 6 months o Some maybe left with residual weakness and 3% will have relapses Guillain-Barre syndrome Mononeuritis multiplex Migraine (paralytic) Paget’s Base of skull (trauma) Basal meningitis Brainstem strokes or multiple sclerosis