How Do Stalks Wither?
advertisement

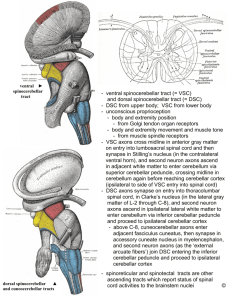
More Than Just Three Pairs of Stalks: Comprehensive Interactive Case Review of Bilateral Cerebellar Peduncle Abnormalities Yin Jie Chen1, Andreas Rauschecker1, Arastoo Vossough2, Laurie A. Loevner1, Suyash Mohan1 1. 2. Department of Radiology, Hospital of the University of Pennsylvania Department of Radiology, Children’s Hospital of Philadelphia Control #: 1252 eEdE-02-7538 Disclosure Statement • No relevant disclosures Goals & Objectives • Goals – Review neurologic diseases exhibiting bilateral superior, middle, and/or inferior cerebellar peduncle abnormalities – Illustrate important imaging and clinical features that help narrow the relevant differential diagnoses • Objectives – Review the anatomy of cerebellar peduncles & associated fiber tracts – Offer approach to narrow differential diagnoses for bilateral cerebellar peduncle abnormalities – Present an interactive case series to improve diagnostic accuracy Cerebellar Peduncles*# • Anatomy, Blood Supply, and Associated Fiber Tracts • Interactive Case Series By Age Group – – – – – Congenital & Genetic Etiologies Neurodegenerative Etiologies Metabolic Etiologies Infectious & Inflammatory Etiologies Neoplastic Etiologies * A stalk bearing a flower or flower cluster or a fructification # Root in New Latin - pedunculus, diminutive of Latin ped-, pes, first known use, 1702 - Merriam-Webster Dictionary, 2015 MCP ICP SCP SCP PS MCP MCP ICP SCP MCP ICP PS PS PS T1 MPRAGE MRI depicting cerebellar peduncles and pons. SCP – superior cerebellar peduncle, MCP – middle cerebellar peduncle, ICP – inferior cerebellar peduncle, PS – pons. SCP SCA MCP AICA ICP PICA T1 MPRAGE MRI images depicting vascular territories: basilar artery, superior cerebellar artery (SCA), anterior inferior cerebellar artery (AICA), & posterior inferior cerebellar artery (PICA). T H SCP MCP ICP A T H P S R F O N P S R F O N SCP MCP D C ICP T H T H R N R N SCP SCP MCP MCP ICP ICP D C B Main afferent (A) and efferent (B) fiber tracts between cerebral cortex and cerebellum through cerebellar peduncles. Olivary nucleus – ON, thalamus – TH, red nucleus – RN, deep cerebellar nucleus – DC, corticopontocerebellar tract, cerebro-olivocerebellar tract, cerebroreticulocerebellar tract, globose-emboliform-rubral tract, dentothalamic tract. Important Fiber Tracts • Corticopontocerebellar tract – Conveys information on planning and initiation of movement – From cerebral cortex to contralateral cerebellum • Cerebro-olivocerebellar tract – Conveys control from cerebral cortex to cerebellar cortex via inferior olivary nuclei and climbing fibers – Terminate directly on Purkinje cells • Cerebroreticulocerebellar tract – Involved in regulation of voluntary movement – In particular adjustment of muscle activity as result of cortical input – Input primarily from sensorimotor areas • Globose-emboliform-rubral tract – Controls ipsilateral motor activity – Connection from globose and emboliform nuclei to contralateral red nucleus, then crossing via rubrospinal tract to ipsilateral motor neurons in spinal cord • Dentothalamic tract – Affects ipsilateral motor activity – Connection from dentate nucleus to contralateral ventrolateral nucleus of the thalamus, in turn connecting to contralateral cerebral motor cortex INTERACTIVE CASE SERIES PEDIATRIC POPULATION 15 M boy with developmental delay, hypotonia, abnormal breathing patterns, and polydactyly T1-Pre T2 T1-Pre Axial T1 MPRAGE pre-contrast and axial T2 images show “molar tooth” sign with deep interpeduncular fossa and thick straight SCPs, as well as hypoplastic vermis. Dx: Joubert Syndrome Joubert Syndrome • Clinical features – – – – – – – Autosomal recessive 1 of 13 mutations in >75% Patient pos with Syndrome DefectsJoubert in primary cilium Facial dysmorphism Polydactyly Most children reach adulthood Outcome not related to severity of imaging findings – Spectrum of abnormalities • Diagnostic pearls – "Molar tooth" sign • Deep interpeduncular fossa Patient •Normal Thick, straight SCP • Hypoplastic vermis – Absence of fiber decussation – Joubert Syndrome-related Disorders • “Molar tooth” sign plus other signs • Cerebello-oculo-renal syndrome • COACH syndrome (Coloboma, oligophrenia, ataxia, cerebellar vermis hypoplasia, hepatic fibrosis) • Developmental delay / mental retardation • Differential considerations • Hypotonia – Dandy-Walker continuum • Respiratory difficulties • "Molar tooth" sign not a feature • Seizures Diffusion tensor imaging shows absence decussation of fibers – of Chiari malformation • Occulomotor, oral-motor, and speech (transversely oriented fibers in red) at the of SCPs in magna • level Obliteration of cisterna problems patient with Joubert Syndrome, compared to cisterna normalmagna patient – Mega • No associated malformation 16 Y/M with developmental delay now with progressive gait abnormality & palatal myoclonus FLAIR T1-Pre T1-Pre T1-Post Axial T1 pre-contrast image show intrinsic T1 hyperintensities in the supratentorial deep white matter. Axial T1 pre and post images demonstrate faint enhancement in deep cerebellar structures. Axial FLAIR images show supratentorial and infratentorial FLAIR hyperintensities, with sparing of the deep gray structures and subcortical white matter. Dx: Alexander Disease Alexander Disease • Diagnosed by genetic testing – GFAP gene (D360H missense mutation for this patient) – Autosomal dominant – Infantile (birth – 2 y/o), juvenile (2-12 y/o), adult (> 12 y/o) forms – Accumulation of Rosenthal fibers (RFs) in astrocytes & hypo-/demyelination – Diagnostic pearls • Enhancement in brainstem and cerebellar peduncles typically exist early in disease course (non-infantile forms) • Infantile form more localized abnormalities in bifrontal white matter • Rostral-caudal gradient less pronounced in juvenile/adult forms Infantile Alexander Disease with bifrontal white matter abnormalities 6 Y/F with severe dystonia, chorea, and slow motor deterioration over 4 years T1-Pre T1-Pre T1-Pre T1-Pre Patient had very elevated manganese levels that responded to chelation for short periods of time, without any identifiable exposure source. Therefore she was given the presumed diagnoses of congenital hypermanganesemia, although no specific genetic mutation has been able to be identified so far. Axial T1 pre-contrast images show intrinsic T1 hyperintensities in the basal ganglia, midbrain, SCP, and cerebellar hemispheres. No signal alterations on other sequences. Dx: Congenital Hypermanganesemia Other Congenital & Genetic Etiologies • Other leukodystrophies – Krabbe Disease – X-linked adrenoleukodystrophy – Mitochondrial leukodystrophy • Pontine tegmental cap dysplasia (PTCD) • Maple syrup urine disease (MSUD) Restricted diffusion in bilateral MCP and Hypoplasia of pons and posterior internal MCPsininneonate newbornwith with capsule feeding difficulty who MSUD was diagnosed with PTCD INTERACTIVE CASE SERIES GERIATRIC POPULATION 81 Y/M with progressive gait abnormalities, urinary incontinence, & cognitive decline T2 T2 T1-Pre http://www.sugarspunmarketing.com/wpcontent/uploads/2013/10/hummingbird.jpg Axial T2 image demonstrates bilateral MCP hyperintensities. Coronal T2 image depicts diffuse supratentorial and infratentorial volume loss. Sagittal T1 image shows midbrain atrophy, so called “hummingbird” sign. Dx: Progressive Supranuclear Palsy Progressive Supranuclear Palsy (PSP) • Part of Parkinson-plus syndromes • Mean age 65 yrs • Clinical presentation – Gait instability – Supranuclear ophthalmoplegia • Diagnostic pearl – severe midbrain atrophy • Differential consideration – Multiple system atrophy (MSA), cerebellar subtype (MSA-C) • Also known as, sporadic olivopontocerebellar atrophy • Gait ataxia, limb akinetic ataxia, dysarthria, cerebellar oculomotor disturbance – Diagnostic pearls • Atrophy isolated to pons & cerebellum • “Hot cross bun” sign 62 Y/O M with MSA-C noting “hot cross bun” sign Other Neurodegenerative Etiologies • Spinocerebellar ataxia • Creutzfeldt-Jakob disease • Fragile X-associated Tremor/Ataxia Syndrome • Autosomal recessive spastic ataxia of Charlevoix- Saguenay • Wolfram syndrome 68 Y/O M with gait instability and presumed diagnosis of Fragile X INTERACTIVE CASE SERIES ALL AGES 60 Y/F with long history of alcohol abuse present with headache, speech disturbance, & tremors Six Months Later T1-Pre FLAIR FLAIR Axial T1 image shows intrinsic T1 hyperintensity in basal ganglia bilaterally. Axial FLAIR image demonstrates FLAIR hyperintensity in MCP bilaterally. After receiving proper treatment, axial FLAIR image from six months later depicts decreased hyperintensity in MCP bilaterally. Dx: Hepatic Encephalopathy Hepatic Encephalopathy • • • Occurs in severe liver dysfunction Occurs in more than 50% cirrhotic patients Clinical presentation – Altered mental status – Motor abnormalities (e.g., tremor, ataxia, etc) – Fetor hepaticus • Diagnostic pearls – Liver dysfunction, most commonly caused by alcohol – T1 hyperintensity in basal ganglia • • Thought to be secondary to manganese deposition Similar to congenital hypermanganesemia – FLAIR hyperintensity within hemispheric white matter and corticospinal tract Companion Case: 31 Y/M with alcohol abuse , tremors, & Wernicke's encephalopathy (symptoms improved with thiamine & folate). T2 hyperintensities within bilateral mammillary bodies and MCP. Other Metabolic Etiologies • Wilson disease • Extra-pontine myelinolysis • Hypoglycemia • Toluene toxicity 23 Y/F with Wilson’s Disease, noting T1 hyperintensity in basal ganglia and bilateral MCP T2 hyperintensity 56 Y/F with AML admitted for acute renal failure presented with abnormal eye movements DWI FLAIR FLAIR FLAIR ADC Dx: Posterior Reversible Encephalopathy Syndrome Axial FLAIR images demonstrate FLAIR hyperintensities in bilateral posterior internal capsule, right occipital lobe, and MCP. Axial DWI and ADC images depict a focus of restricted diffusion in right MCP. Posterior Reversible Encephalopathy Syndrome (PRES) • Most commonly seen in acute / malignant hypertension – Disruption of auto-regulation and blood brain barrier – Several other causes including drug toxicity • Diagnostic pearls – Patchy foci of T1 hypo- and T2 hyper-intensities in posterior circulation – Usually only vasogenic edema, but can have foci of cytotoxic edema Companion Case: Cyclosporine toxicity with FLAIR hyperintensity in thalami, pons, parieto-occipital white matter & cerebellum. Note: vasogenic edema Other Cerebrovascular Etiologies •• Bilateral Unknown anterior Case One •Wallerian Unknown Case Two degeneration POP• QUIZ inferior cerebellar pontocerebellar What is the arterial bloodof supply to the MCP?tracts arteries (AICA) infarct A. Superior cerebellar artery B. Anterior inferior cerebellar artery C. Posterior inferior cerebellar artery D. Basilar artery 43 Y/F status post TEVAR, noting bilateral restricted diffusion in AICA territory 61 Y/M with recent pontine infarct due to basilar artery stenosis now with bilateral MCP FLAIR hyperintensities 60 Y/M with fever, lethargy, nausea, vomiting and difficulty with micturition; returned from a safari in Tanzania 3 weeks ago FLAIR FLAIR FLAIR images of the brain and spine demonstrate FLAIR hyperintensities in the subcortical / deep white matter, midbrain, MCP, and spine cord. CSF studies showed 8 RBC, 385 WBC (86% lymphocytes), Glu 62, Protein 223, and negative Gram stain and culture. Dx: Acute Disseminated Encephalomyelitis Acute Disseminated Encephalomyelitis (ADEM) • Autoimmune-mediated acute demyelination • Prodromal phase (fever, malaise, myalgia), followed by symptoms such as headache and drowsiness, with progression to lethargy or even coma • Diagnostic pearls – Multifocal T2/FLAIR white matter hyperintensities, – Possibly also deep grey structures – Following recent infection, often viral (can be post-vaccination) Companion Case: 51 Y/M with AML s/p SCT with acute encephalopathy FLAIR hyperintensities in periventricular WM, midbrain, and cerebellar peduncles (bilateral SCP, MCP, and ICP, top to bottom) Dx: Immune-mediated Demylination (Presumed to be related to SCT) 37 Y/F with stiffness in the mornings and leg twitches in the evenings Three years ago T2 Current Study T2 MRI from three years ago shows scatter periventricular T2 hyperintensities. Current study shows new T2 hyperintensities involving both ICPS, in addition to the periventricular lesions. Dx: Multiple Sclerosis Multiple Sclerosis • Demographics – – – – Age: 20-40 years Prevalence: F > M Caucasian most common Variable symptoms • • • • Weak, numb, tingling, gait disturbance, Optic neuritis, other cranial nerve palsies Spinal cord involved in 80% Diagnostic pearls – Multiple periventricular/perivenular T2 hyperintensities • “Dawson fingers” – Infratentorial in 10% – Acutely demyelinating lesions can enhance (nodular or ring) – Polyphasic • • • • Relapsing-remitting – most common (>80%) Secondary-progressive Primary-progressive Progressive-replapsing – rare Companion Case: MS patient with scattered FLAIR hyperintensities in periventricular white matter and bilateral MCP Other Infectious & Inflammatory Etiologies •• Neurosarcoidosis History of sarcoidosis •• Progressive multifocal History of HIV/AIDS leukoencephalopathy (PML) FLAIR hyperintensities and small foci of enhancement in bilateral MCP in this patient with transbronchial biopsy proven sarcoidosis FLAIR hyperintensities in bilateral MCP in this patient with HIV/AIDS 60 Y/M with renal cell carcinoma present with horizontal diplopia suspicious for sixth and seventh nerve palsies T1-Pre T1-Post FLAIR CBV Short TE MRS Axial T1 pre and post contrast images shows a heterogeneously enhancing mass centered in the pons, associated with surrounding FLAIR hyperintensities extending into bilateral MCP, as well increased relative cerebral blood volume. Short TE MR spectroscopy demonstrates elevation of lipid-lactate peaks. Dx: Metastatic RCC Metastatic RCC • • Stereotactic biopsy - clear cell carcinoma consistent with renal origin Diagnostic pearls – Known primary malignancy, especially with known metastases elsewhere – Mass with aggressive features on perfusion and spectroscopy studies • Differential consideration – Glioma • • Enhancement pattern varies depending on type Often less surrounding vasogenic edema than metastases – Lymphoma • • More homogenous enhancement Usually hyperdense on CT and can show restricted diffusion – Radiation changes / necrosis • • Expect to decrease over time Necrosis – – Most often 12-24 months post radiation Expect very low NAA, Cho, and Cr peaks on MR spectroscopy FLAIR hyperintensity in bilateral MCP from radiation change related to prior treatment of left temporal lobe astrocytoma 15 Y/M with tectal pilocytic astrocytoma s/p resection & proton therapy, now with refusal to speak Pre-Operative T1-Pre Current Exam T1-Pre FLAIR FLAIR T1-Post T1-Post Pre-operative T1-MPRAGE pre-/post-contrast images show avidly enhancing tectal mass. Post-treatment MRI (when patient presented with mutism) show no residual enhancing tumor and increased FLAIR signal in the both SCPs. Dx: Cerebellar Mutism Syndrome Cerebellar Mutism Syndrome • Also called posterior fossa syndrome • Typically occur after resection of posterior fossa tumors • Incidence post midline posterior fossa tumor resection as high as 40% • Clinical symptoms – Transient mutism (days to weeks) – Cognitive & behavioral issues – Emotional liability – Persistent ataxia and motor coordination issues can occur • Attributed to damage of bilateral dentate nuclei or cerebellar output pathways (SCPs) • SCPs vulnerable during resection due to their close relationship to the 4th ventricle • Ojemann JG, et al., showed that diffusion tensor imaging of SCPs can identify patients who did and did not develop cerebellar mutism syndrome in a small sized patient population Conclusions • SCP, MCP, and ICP are vital to proper communication between cerebral cortex and cerebellum • Bilateral cerebellar peduncle abnormalities can be seen in many disease processes • Considering image findings in the appropriate clinical settings is vital in narrowing differential diagnoses • Diagnostic considerations – Congenital & genetic causes common in pediatric population – Neurodegenerative causes common in geriatric population – Most other causes can be seen in all age groups Conclusions • Disease specific diagnostic pearls – Congenital & Genetic • Joubert Syndrome – “Molar tooth” sign • Alexander Disease - enhancement in brainstem and cerebellar peduncles early in disease course (non-infantile forms) • Congenital hypermanganesemia – abnormal heavy metal labs • Pontine tegmental cap dysplasia – newborn with hypoplasia of pons and cerebellar peduncles – Neurodegenerative • PSP - severe midbrain atrophy, “Hummingbird” sign • MSA – pons atrophy, “hot cross bun” sign Conclusions • Disease specific diagnostic pearls, continued – Metabolic • Hepatic encephalopathy – alcohol most common causative agent • Wilson disease - T1 hyperintensity in basal ganglia – Cerebrovascular • PRES – HTN or drug toxicity, posterior circulation abnormalities • Stroke – AICA territory, rare to have bilateral • Wallerian degeneration of pontocerebellar tracts – prior pontine insult – Infectious & inflammatory • ADEM – most commonly follow viral infection, monophasic • MS – multiple lesions separate in space and time Conclusions • Disease specific diagnostic pearls, continued – Neoplastic • • • • • Metastases - Known primary malignancy Glioma – less surrouding vasogenic edema Lymphoma – more homogenous enhancement Radiation changes / necrosis – within radiation portal Cerebellar mutism syndrome – post-resection of posterior fossa tumor, abnormal signal in SCPs References • • • • • • • • • • • • • • • Apartis E, Blancher A, Meissner WG, et al. FXTAS: new insights and the need for revised diagnostic criteria. Neurology. 2012;79(18):1898-907. Graff-Radford J, Schwartz K, Gavrilova RH, et al. Neuroimaging and clinical features in type II (late-onset) Alexander disease. Neurology. 2014;82(1):49-56. Ito S, Sakakibara R, Hattori T. Wolfram syndrome presenting marked brain MR imaging abnormalities with few neurologic abnormalities. AJNR Am J Neuroradiol. 2007;28(2):305-6. Kataoka H, Izumi T, Kinoshita S, et al. Infarction limited to both middle cerebellar peduncles. J Neuroimaging. 2011;21(2):e171-2. Lee NK, Lee BH, Hwang YJ, et al. Serial computed tomography and magnetic resonance imaging findings of biphasic acute hemorrhagic leukoencephalitis localized to the brain stem and cerebellum. Jpn J Radiol. 2011;29(3):212-6. Liptai Z, Papp E, Barsi P, et al. Progressive multifocal leukoencephalopathy in an HIV-infected child. Neuropediatrics. 2007;38(1):32-5. Maria B, Quisling RG, Rosainz LC, et al. Molar tooth sign in Joubert Syndrome: clinical, radiologic, and pathologic significance. J Child Neurol. 1999;14:368-76. Nishida T, Tokumaru AM, Doh-Ura K, et al. Probable sporadic Creutzfeldt-Jakob disease with valine homozygosity at codon 129 and bilateral middle cerebellar peduncle lesions. Intern Med. 2003;42(2):199-202. Ojemann JG, Partridge SC, Poliakov AV, et al. Diffusion tensor imaging of the superior cerebellar peduncle identifies patients with posterior fossa syndrome. Childs Nerv Syst. 2013;29:2071-7. Okamoto K, Tokiguchi S, Furusawa T, et al. MR features of diseases involving bilateral middle cerebellar peduncles. AJNR. 2003;24(10):1946-54. Preziosa P, Rocca MA, Mesaros S, et al. Relationship between damage to the cerebellar peduncles and clinical disability in multiple sclerosis. Radiology. 2014;271(3):822-30. Reginold W, Lang AE, Marras C, et al. Longitudinal quantitative MRI in multiple system atrophy and progressive supranuclear palsy. Parkinsonism Relat Disord. 2014;20(2):222-5. Shimazaki H, Takiyama Y, Honda J, et al. Middle cerebellar peduncles and Pontine T2 hypointensities in ARSACS. J Neuroimaging. 2013;23(1):82-5. Suzuki K, Wakayama Y, Takada H, et al. A case of chronic toluene intoxication with abnormal MRI findings: abnormal intensity areas in cerebral white matter, basal ganglia, internal capsule, brain stem and middle cerebellar peduncle. Rinsho Shinkeigaku. 1992;32(1):84-7. Wells EM, Khademian ZP, Walsh KS, et al. Postoperative cerebellar mutism syndrome following treatment of medulloblastoma: neuroradiographic features and origin. J Neurosurg Pediatrics. 2010;5:329-34. Thank You Very Much For Reviewing Our Exhibit Yin.Chen@uphs.upenn.edu Suyash.Mohan@uphs.upenn.edu