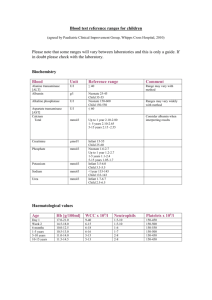
Blood and endocrine system diseases
advertisement
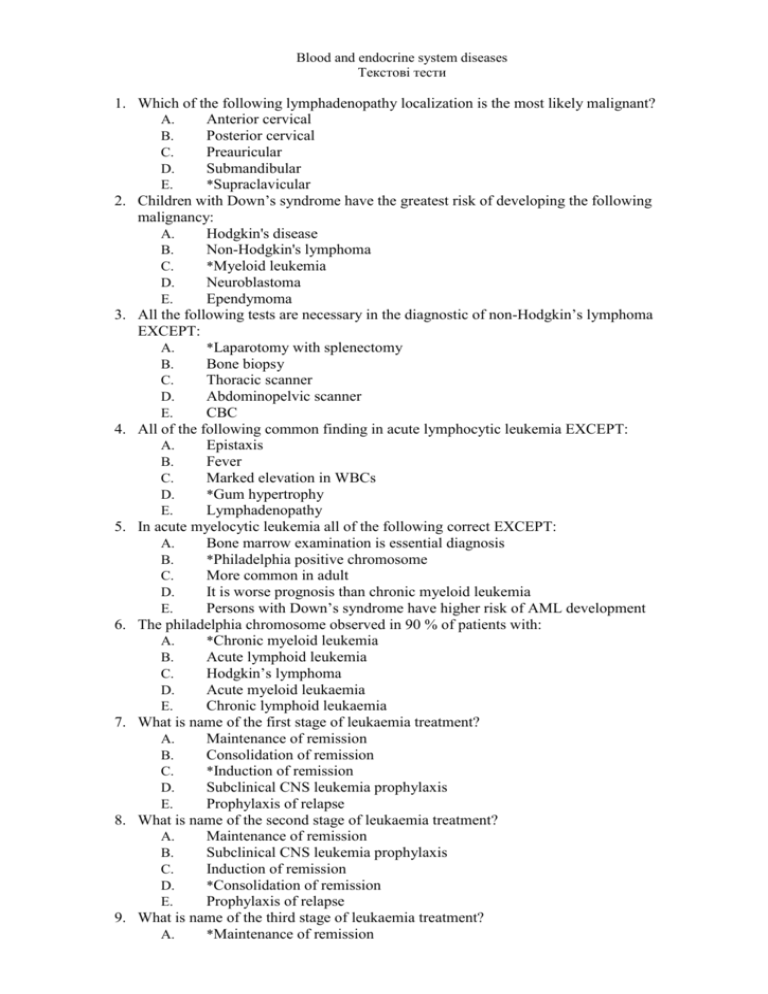
Blood and endocrine system diseases Текстові тести 1. Which of the following lymphadenopathy localization is the most likely malignant? A. Anterior cervical B. Posterior cervical C. Preauricular D. Submandibular E. *Supraclavicular 2. Children with Down’s syndrome have the greatest risk of developing the following malignancy: A. Hodgkin's disease B. Non-Hodgkin's lymphoma C. *Myeloid leukemia D. Neuroblastoma E. Ependymoma 3. All the following tests are necessary in the diagnostic of non-Hodgkin’s lymphoma EXCEPT: A. *Laparotomy with splenectomy B. Bone biopsy C. Thoracic scanner D. Abdominopelvic scanner E. CBC 4. All of the following common finding in acute lymphocytic leukemia EXCEPT: A. Epistaxis B. Fever C. Marked elevation in WBCs D. *Gum hypertrophy E. Lymphadenopathy 5. In acute myelocytic leukemia all of the following correct EXCEPT: A. Bone marrow examination is essential diagnosis B. *Philadelphia positive chromosome C. More common in adult D. It is worse prognosis than chronic myeloid leukemia E. Persons with Down’s syndrome have higher risk of AML development 6. The philadelphia chromosome observed in 90 % of patients with: A. *Chronic myeloid leukemia B. Acute lymphoid leukemia C. Hodgkin’s lymphoma D. Acute myeloid leukaemia E. Chronic lymphoid leukaemia 7. What is name of the first stage of leukaemia treatment? A. Maintenance of remission B. Consolidation of remission C. *Induction of remission D. Subclinical CNS leukemia prophylaxis E. Prophylaxis of relapse 8. What is name of the second stage of leukaemia treatment? A. Maintenance of remission B. Subclinical CNS leukemia prophylaxis C. Induction of remission D. *Consolidation of remission E. Prophylaxis of relapse 9. What is name of the third stage of leukaemia treatment? A. *Maintenance of remission Consolidation of remission Induction of remission Subclinical CNS leukemia prophylaxis Prophylaxis of relapse 10. What is normal lymphoblast concentration in bone marrow? A. Not more than 1 % B. *Not more than 5 % C. Not more than 25 % D. Not more than 35 % E. Not more than 50 % 11. What number of lymphoblast in bone marrow prove diagnose of leukemia? A. Any number (they should be absent in healthy) B. More than 5 % C. More than 10 % D. *More than 25 % E. More than 50 % 12. What test is definitive for leukemia diagnostic? A. Lymph node biopsy B. CT-scan C. Complete blood count D. *Bone marrow smear E. Coagulogram 13. All the following are poor prognostic signs in leukemia EXCEPT of: A. High WBC count B. Presence of chromosomes translocations C. Blasts with T-cell phenotype. D. Age less than 1 year old E. *Female sex 14. All the following are good prognostic signs in leukemia EXCEPT of: A. Low WBC count B. Absence of L3 cells C. Platelet count greater 100 G/L D. *Age less than 1 year old E. Absence of lymphomatous features 15. The atrophyc glossitis is the typical symptom of the: A. Hemolytic anemia B. Acute leukemia C. *B12-deficiency anemia D. Iron-deficiency anemia E. ITP 16. The most sensitive and accurate laboratory determination in the diagnosis of iron-deficiency anemia nd in monitoring the treatment of the disease is A. The serum iron level B. *The serum ferritin level C. The hemoglobin level D. The total iron-binding capacity E. Hemoglobin electrophoresis 17. The highest hemoglobin level normally is present in: A. *Newborns B. Six months old infants C. Adolescence D. Young adult male E. Pregnant woman 18. Which of the following is INCORRECT concerning aplastic anemia? B. C. D. E. Can be caused by drugs There is decreased platelet counts *Bone marrow may show increased number of megakaryocytes Bone marrow may show decreased red cell formation Can be elevation of serum iron 19. All of the following conditions are characterized by hypochromic, microcytic red cells EXEPT: A. Iron deficiency anemia B. alfa thalassemia major C. beta thalassemia minor D. *G6PD deficiency E. anemia of chronic disease 20. Which of the following statements regarding the anemia of chronic disease is true? A. MCV is elevated B. Serum iron level is elevated C. Serum iron-binding capacity is elevated D. *Marrow iron stores are increased E. Iron therapy is required to raise hemoglobin level 21. Hemolytic-uremic syndrome is a disorder of which of the following? A. The red cell membrane B. *The vascular endothelium C. Hemoglobin D. The glycolytic pathway E. Immune regulation 22. Which of the following hemolytic anemias is NOT associated with an intracorpuscular defect? A. Hereditary sherocytosis B. Sickle cell anemia C. *Autoimmune hemolytic anemia D. G6PD deficiency E. Hereditary elliptocytosis 23. Which of the following is NOT a characteristic of Fanconi’s anemia? A. *Hematologic abnormalities in infancy B. Pancytopenia C. Skeletal abnormalities D. Chromosome fragility E. Renal abnormalities 24. What level of hemoglobin is suggestive of anemia in children between 6 month to 5 years old? A. *Below 110 g/L B. Below 120 g/L C. Below 130 g/L D. Below 140 g/L E. Below 150 g/L 25. What level of hemoglobin is suggestive of anemia in children older than 5 years old? A. *Below 12 g/L B. Below 13 g/L C. Below 14 g/L D. Below 15 g/L E. Below 16 g/L 26. All of the following conditions are characterized by hypochromic, microcytic red cells EXEPT: A. Lead poisoning B. Beta thalassemia major A. B. C. D. E. Pyridoxine responsive anemia *Sickle cell disease Dyserythropoietic anemia 27. Choose the condition which is characterized by hypochromic, microcytic anemia: A. Iron deficiency B. Beta thalassemia major C. Pyridoxine responsive anemia D. Lead poisoning E. *All is correct 28. Choose the condition which is characterized by normochromic, normocytic anemia: A. Iron deficiency B. Beta thalassemia major C. Pyridoxine responsive anemia D. Lead poisoning E. *Fanconi’s anemia 29. Which of the following tests is the most helpful in diagnosis of thalassemia : A. Serum iron and iron binding capacity B. Bone marrow examination C. *Hemoglobin electrophoresis D. Coomb’s test E. Platelets level 30. Anemia characterized by increase RBCs production is: A. Iron-deficiency anemia B. *Hereditary Spherocytosis C. Fanconi's Anemia D. Anemia of chronic disease E. Megaloblastic anemia 31. All the following can be associated with sickle cell anemia EXCEPT: A. Vaso-occlusive crisis B. Infection C. *Bleeding disease D. Splenic sequestration E. Acute chest syndrome 32. Which of the following haemoglobin (Hb) estimation will be diagnostically helpful in a case of beta thalassemia trait? A. Hb-S B. Hb-C C. *Hb-A2 D. Hb-A E. Hb-C2 33. All of the following are true of ? thalassemia major, except: A. Splenomegaly B. Target cells on peripheral smear C. Microcytic hypochromic anemia D. *Increased osmotic fragility E. Growth failure 34. Choose the essential links of a hemostasis: A. Vascular integrity B. Qualitative and quantative characteristics of platelets C. Presence of coagulation factors in blood D. All is incorrect E. *All is correct 35. What is the synonym of the Schonlein-Henoch purpura? A. Idiopathic thrombocytopenic purpura C. D. E. Von Willebrand disease *Hemorrhagic vasculitis Fanconi pancytopenia Allergic dermatitis 36. What is NOT the synonym of the hemorrhagic vasculitis? A. *Von Willebrand disease B. Schonlein-Henoch purpura C. Allergic angiitis D. Anaphylactoid purpura E. Henoch-Schonlein disease 37. All the following disorders are associated with prolonged bleeding time EXEPT: A. *Hemophilia A B. von Willebrand’s disease C. Aspirin-induced thrombocytopathia D. Bernard-Soulier syndrome E. ITP 38. Patients with DIC present with all of the following hematologic abnormalities EXEPT: A. Thrombocytopenia B. Microangiopathic blood smear C. Hypofibrinogenemia D. Prolonged PTT E. *Low levels of fibrin degradation products 39. The most common cause for acute onset of thrombocytopenia in an otherwise well child is: A. von Willebrand disease B. Acute leukemia C. *Idiopathic (immune) thrombocytopenic purpura D. Aplastic anemia E. Thrombotic thrombocytopenic purpura 40. Choose the correct statement concerning ITP in children: A. 60 to 80 % of children who present with acute ITP will have spontaneous resolution of their ITP ithin 6 mo B. Less than 1 % will develop intracranial hemorrhage C. About 10 to 20 % of children who present with acute ITP go on to develop chronic ITP D. The presence of abnormal finding such as hepatosplenomegaly or remarkable lymphadenopathy suggests another diagnosis E. *All is correct 41. Choose the INCORRECT statement concerning ITP in children: A. 60 to 80 % of children who present with acute ITP will have spontaneous resolution of their ITP ithin 6 mo B. *Intracranial hemorrhage is very frequent complication of acute ITP C. About 60 to 80 % of children who present with acute ITP go on to develop chronic ITP D. The presence of abnormal finding such as hepatosplenomegaly or remarkable lymphadenopathy suggests another diagnosis E. All is correct 42. What maximal level of thrombocytes is suggestive for ITP? A. Less than 250,000/mm3 B. Less than 180,000/mm3 C. *Less than 150,000/mm3 D. Less than 100,000/mm3 E. Less than 50,000/mm3 43. What laboratory findings are typical for acute ITP? A. Anemia and thrombocytopenia B. C. D. E. B. C. D. E. *Isolated thrombocytopenia Thrombocytopenia and leukocytosis Thrombocytopenia and leucopenia Presence of blasts 44. What bone marrow examination results are typical for acute ITP? A. *Normal granulocytic and erythrocytic series with increased number of megakaryocytes B. Decreased granulocytic, erythrocytic and megakaryocytic series C. Increased granulocytic, erythrocytic and megakaryocytic series D. Decreased granulocytic and erythrocytic series with increased number of megakaryocytes E. Increased granulocytic and erythrocytic series with decreased number of megakaryocytes 45. If the VII plasma coagulation factor is decreased, it will be abnormal: A. Platelets count B. Prothrombin time C. *Clotting time D. Amount of fibrinogen E. Bleeding time 46. If the IX plasma coagulation factor is decreased, it will be abnormal: A. *Partial thromboplastin time B. Thrombin time C. Clotting time D. Amount of fibrinogen E. Bleeding time 47. What rush characteristics are typical for ITP? A. Polymorphous B. Polychromatic C. Asymmetric D. Petechiae and purpura E. *All is correct 48. Which rush characteristic is NOT typical for ITP? A. Polymorphous B. Polychromatic C. *Symmetric D. Petechial E. Purpuric 49. What is normal time of plasma recalcification? A. 20-40 sec B. *60-120 sec C. 160-180 sec D. 200-250 sec E. 250-300 sec 50. What is normal partial thromboplastin time? A. 5-10 sec B. 15-20 sec C. *25-35 sec D. 40-60 sec E. 80-120 sec 51. What is normal prothrombin time? A. 2-5 sec B. *10-12 sec C. 20-22 sec D. 40-60 sec E. 80-120 sec 52. What is normal bleeding time by Duke? A. 30-60 sec B. 1-2 min C. *2-5 min D. 5-10 min E. 10-15 min 53. What is normal clotting time by Lee-White? A. 30-60 sec B. 1-2 min C. 2-5 min D. *5-10 min E. 10-15 min 54. Choose the CORRECT statement concerning ITP treatment: A. It doesn’t require treatment B. *Children who have platelet counts > 30,000/mm3 and are asymptomatic or have only minor purpura do not require routine treatment C. Children who have platelet counts < 10,000/mm3 and are asymptomatic or have only minor purpura do not require routine treatment D. Treatment doesn’t depend on the platelets level and is performed only in bleedings E. All is incorrect 55. What medicines are the most effective in ITP treatment? A. *Intravenous immune globulin (IVIG) and prednisone B. Antibiotics and non-steroid anti-inflammatory C. Slow acting antirheumatoid drugs (SAARDS) and cytostatics D. Whole blood transfusion E. Bone marrow transplantation 56. What is usual prednisolone dose for ITP treatment? A. 0,1-0,2 mg/ kg/day B. *1-2 mg/ kg/day C. 3-4 mg/ kg/day D. 10 mg/ kg/weekly E. 30 mg/ kg/day 57. What does NOT include supportive care in acute ITP? A. Restriction of physical activities B. Avoidance of aspirin C. Avoidance of intramuscular injections D. *Daily massages E. Hypoallergic diet 58. Choose the optimal age for splenectomy in ITP (in case of need): A. Till 1 year B. 1-2 years C. 3-4 years D. 4-5 years E. *After 6 years 59. Intracranial hemorrhage in ITP is the most common when platelets count is: A. More 50,000/mm3 B. Below 50,000/mm3 C. More 20,000/mm3 D. *Below 20,000/mm3 E. Below 100,000/mm3 60. The classic triad of the Wiskott-Aldrich syndrome includes: A. Thrombocytopenia, mental retardation and immunodeficiency Thrombocytosis, mental retardation and immunodeficiency *Thrombocytopenia, eczema and immunodeficiency Thrombocytosis, eczema and immunodeficiency Thrombocytopenia, eczema and seizures 61. What is the etiology of the Wiskott-Aldrich syndrome: A. *X-linked recessive B. Autosomal recessive C. Autosomal dominant D. Infectious E. Autoimmune 62. Choose the thrombocytopathia with thrombocytopenia: A. Glanzmann’s thromboasthenia B. Gray platelet syndrome C. Thrombosis D. Dence body deficiency E. *Bernard Soulier syndrome 63. Choose the platelets disorder with normal platelets count: A. *Glanzmann’s thromboasthenia B. ITP C. Bernard Soulier syndrome D. TAR-syndrome E. Wiskott-Aldrich syndrome 64. An infant or young child with ITP, which was undergone splenectomy, has an increase risk of: A. Thrombocytosis B. Polycytemia C. Leukemia D. *Severe bacterial infection E. Hemolytic anemia 65. Choose the correct statement concerning idiopathic thrombocytopenic purpura in children: A. *Often follows a viral infection B. Typically has a chronic course, with relapses following each remission C. Is characteristically associated with splenomegaly D. Is associated with reduction of megacaryocytes on bone marrow examination E. Requires splenectomy in more than 20 % cases 66. Platelet transfusion may be indicated in patients with: A. Haemophylia B. Henoch- Schoenlein purpura C. *Aplastic anemia D. Chronic ITP E. Lupus erythematosus 67. Choose the INCORRECT statement concerning hemophilia A: A. All males with defective gene have hemophilia B. *It’s inherited in an autosomal dominant pattern C. 100% of daughter's of hemophilic man will be carriers D. It’s the most common type of hemophylia E. There is factor VIII deficiency 68. What is the synonym of idiopathic thrombocytopenic purpura? A. Von Willebrand's disease B. *Werlhof’s disease C. Schonlein-Henoch purpura D. Bernard-Soulier syndrome E. All is incorrect 69. What symptom is the most indicative for platelets problems? B. C. D. E. Delayed bleeding from old wounds Hemorrhage into joint space Bleeding from multiple sites *Presence of petechiae on skin and mucosal surfaces Gastrointestinal bleeding 70. What symptom is NOT indicative for platelets problems? A. *Delayed bleeding from old wounds B. Epistaxis C. Hematuria D. Menorrhagia E. Gastrointestinal bleeding 71. What symptom is the most indicative for DIC syndrome? A. Delayed bleeding from old wounds B. Hemorrhage into joint space C. *Bleeding from multiple sites D. Presence of petechiae on skin and mucosal surfaces E. Gastrointestinal bleeding 72. What is the inheritance pattern of the von Willebrand disease? A. X-linked B. Y-linked C. *Autosomal dominant D. Autosomal recessive E. It is aquired problem 73. What is the inheritance pattern of the hemophilia? A. *X-linked B. Y-linked C. Autosomal dominant D. Autosomal recessive E. It is aquired problem 74. What is the inheritance pattern of the Shoenlein-Genoch's disease? A. X-linked B. Y-linked C. Autosomal dominant D. Autosomal recessive E. *It is an acquired problem 75. What is the inheritance pattern of the hemophilia C? A. X-linked B. Y-linked C. Autosomal dominant D. *Autosomal recessive E. It is aquired problem 76. The Christmas disease is the synonym of the: A. Hemophilia A B. *Hemophilia B C. Hemophilia C D. Hemorrhagic vasculitis E. Thrombocytopenic purpura 77. The reason of hemophilia A is: A. Factor VII deficiency B. *Factor VIII deficiency C. Factor IX deficiency D. Factor XI deficiency E. Vitamin K deficiency 78. The reason of hemophilia B is: A. B. C. D. E. Factor VII deficiency Factor VIII deficiency *Factor IX deficiency Factor XI deficiency Vitamin XII deficiency 79. The reason of hemophilia C is: A. Factor VII deficiency B. Factor VIII deficiency C. Factor IX deficiency D. *Factor XI deficiency E. Vitamin XII deficiency 80. What index is the specific for the von Willebrand disease diagnostic in difference from other oagulation disorders? A. Time of bleeding B. PTT C. Time of clotting D. *Ristocetin cofactor activity E. Platelets level 81. What coagulation factor is NOT vitamin K dependent? A. Factor II B. *Factor V C. Factor VII D. Factor IX E. Factor X 82. What coagulation factor measurement is useful to distinguish liver disease from vitamin K deficiency? A. Factor II B. *Factor V C. Factor VII D. Factor IX E. Factor X 83. What coagulation factor measurement is useful to distinguish DIC from vitamin K deficiency and liver disease? A. Factor II B. Factor V C. *Factor VIII D. Factor IX E. Factor X 84. What is platelet survival time in healthy persons? A. 1-2 days B. *7-10 days C. 20-30 days D. 50-60 days E. 120 days 85. What is the indication for bone marrow evaluation in ITP? A. Nasal bleedings B. *If steroid therapy is to be used C. Isolated thrombocytopenia D. Numerous skin petechia E. All is correct 86. What is NOT indication for bone marrow evaluation in ITP? A. *Nasal bleedings B. If steroid therapy is to be used C. Other cell lines (besides of platelets) are involved A. B. C. D. E. Weight loss Splenomegaly 87. What medicines give the best and the fastest response in the most children with ITP? A. Glucocorticoids B. *IVIG (Intravenous immune globulin) C. Anti-D immunoglobulin D. Splenectomy E. Cytostatics 88. What should be minimal persistence of acute ITP to define it as a chronic ITP? A. More than 1 month B. More than 3 - 6 months C. *More than 6 - 12 months D. More than 18 - 24 months E. More than 36 months 89. Initially urticarial lesions which may itch or burn and then develop into pink maculopapules are typical for the: A. von Willebrand’s disease B. Wiskott-Aldrich syndrome C. Hemophilia A D. *Hemorrhagic vasculitis E. ITP 90. Which organ involvement is typical for Schoenlein-Henoch purpura? A. Kidneys B. GI tract C. Musculosceletal system D. Scrotum E. *All is correct 91. Scrotal involvement with epididimidis, orchitis, testicular torsion and scrotal bleeding are typical for the: A. von Willebrand’s disease B. Wiskott-Aldrich syndrome C. Hemophilia A D. *Hemorrhagic vasculitis E. ITP 92. Renal involvement which ranges in severity from microscopic hematuria to nephritic syndrome is typical for the: A. *Schoenlein-Henoch purpura B. Wiskott-Aldrich syndrome C. Hemophilia A D. von Willebrand’s disease E. Werlhof’s disease 93. What are the characteristic laboratory findings in Schoenlein-Henoch purpura? A. Prolonged time of bleeding and thrombocytopenia B. Prolonged thromboplastin time and PTT C. Prolonged clotting time and leukocytosis D. *Elevated Ig A and leukocytosis E. Elevated Ig A and thrombocytopenia 94. Joint involvement with periarticular swelling of the knees, ankles, wrists and elbows is typical for the: A. *Schonlein-Henoch purpura B. Wiskott-Aldrich syndrome C. Hemophilia A D. von Willebrand’s disease E. Werlhof’s disease D. E. 95. Treatment for the patient with in the Hashimoto thyroiditis includes: A. Iodine B. *Hormonal replacement therapy if she becomes hypothyroid C. PTU (propylthiouracil) D. Psychiatry consult E. Surgical removal of thyroid gland 96. What is the main etiologic medicine in thyroid storm? A. Insulin B. Methimazole C. Propranolol D. *Propylthiouracil E. Prednisone 97. What is the alternative (second) etiologic medicine in thyroid storm? A. Insulin B. *Methimazole C. Propranolol D. Propylthiouracil E. Prednisone 98. What is the medicine for minimizing of tachycardia and hypertension in thyroid storm? A. Dopamin B. Methimazole C. *Propranolol D. Propylthiouracil E. Prednisone 99. What is mechanism of propylthiouracil action in thyroid storm? A. *Blocks peripheral conversion of T4 to T3 B. Increase TSH secretion with pituitary gland C. Decrease TSH secretion with pituitary gland D. Stimulates peripheral conversion of T4 to T3 E. Stumulates TRH secretion with hypothalamus 100. What is daily hydrocortizon dose for continuous infusion in adrenal crisis? A. 1-2 mg/kg B. 5-10 mg/kg C. *10-15 mg/kg D. 15-20 mg/kg E. 20-25 mg/kg 101. What symptom is NOT typical for Grave’s disease? A. Nervousness B. Moist skin C. *Bradycardia D. Tremor E. Exophthalmia 102. What symptom is NOT typical for Grave’s disease? A. *Mental retardation B. Moist skin C. Tachycardia D. Tremor E. Exophthalmia 103. What symptom is typical for Grave’s disease? A. Jaundice B. *Moist skin C. Bradycardia D. Mental retardation E. Obesity 104. A. B. C. D. E. 105. A. B. C. D. E. 106. What symptom is typical for Grave’s disease? Obesity Dry skin Bradycardia Mental retardation *Tremor What hormones are secreted by adenohypophysis? Growth hormone, ACTH, aldosterone Growth hormone, ACTH, antidiuretic hormone Parathyroid hormone, TSH, luteinizing hormone *ACTH, TSH, luteinizing hormone Growth hormone, ACTH, glucagons Name the target organ of somatotropic hormone? *Bone Mammary gland Testis Stomach Thyroid gland A. B. C. D. E. 1. 108. A. ch hypophyseal hormone has antidiuretic action? B. Somatotropic hormone (STH) C. Adrenocorticotrophic hormone (ACTH) D. *Thyroid-stimulating hormone (TSH) E. Vasopressin F. Oxytocin 109. Name the target organ of prolactin? A. Bone B. *Mammary gland C. Testis D. Stomach E. Thyroid gland 110. Epinephrine is produced by: A. Cortex of adrenal glands B. Zona glomerulosa of adrenal glands C. Zona reticularis of adrenal glands D. Zona fasciculata and reticularis of adrenal glands E. *Medulla of adrenal glands 111. Glucocorticoids are produced by: A. *Cortex of adrenal glands B. Zona glomerulosa of adrenal glands C. Zona reticularis of adrenal glands D. Zona fasciculata and reticularis of adrenal glands E. Medulla of adrenal glands 112. What glands are the regulators of all endocrine system? A. *Hypothalamus and hypophysis B. Hypophysis and epiphysis C. Hypothalamus and epiphysis D. Hypothalamus, hypophysis and epiphysis E. Hypothalamus 113. Sex hormones (androgens, estrogens, progesterone) are produced by: A. Cortex of adrenal glands B. Zona glomerulosa of adrenal glands C. *Zona reticularis of adrenal glands D. Zona fasciculata and reticularis of adrenal glands 114. 115. 116. 117. 118. 119. 120. 121. 122. E. Medulla of adrenal glands Mineralocorticoids are produced by: A. Cortex of adrenal glands B. *Zona glomerulosa of adrenal glands C. Zona reticularis of adrenal glands D. Zona fasciculata and reticularis of adrenal glands E. Medulla of adrenal glands Acromegaly is the result of: A. Hypersecretion of growth hormone in the childhood B. *Hypersecretion of growth hormone in the elder age C. Hypersecretion of adrenocorticotropic hormone in the elder age D. Hyposecretion of growth hormone in the childhood E. Hypersecretion of adrenocorticotropic hormone in the childhood Gigantism is the result of: A. *Hypersecretion of growth hormone in the childhood B. Hypersecretion of growth hormone in the elder age C. Hypersecretion of adrenocorticotropic hormone in the elder age D. Hyposecretion of growth hormone in the childhood E. Hypersecretion of adrenocorticotropic hormone in the childhood Growth hormone deficiency is usually associated with: A. *Hypopituitarism B. Hypothyroidism C. Hypogonadism D. Hypoaldosteronism E. Hypoinsulinism What hormone is secreted by adenohypophysis? A. Aldosterone B. *Growth hormone C. Parathyroid hormone D. Vasopressin E. Glucagon What hormone is secreted by neurohypophysis? A. Aldosterone B. Growth hormone C. Parathyroid hormone D. *Vasopressin E. Glucagon In the female the analogue of male’s interstitial cell-stimulating hormone (ICSH) is: A. Prolactin B. Melanocyte-stimulating hormone C. *Luteinizing hormone D. Estradiol E. Cortisol What process is controlled with parathyroid glands? A. Protein metabolism B. Lipid metabolism C. *Phosphoric-calcium metabolism D. Vitamin metabolism E. Carbohydrates metabolism What is hypopinealism? A. Hypothalamus hypofunction B. *Epiphysis hypofunction C. Hypophysis hypofunction D. Adrenals hypofunction 123. 124. 125. 126. 127. 128. 129. 130. 131. E. Testis hypofunction Dwarfism can be caused with? A. Epinephrin deficiency B. Cortisol deficiency C. Glucagon deficiency D. Prolactin deficiency E. *Somatotropin deficiency What does appear in the case of growth hormone hyposecretion? A. Addison’s disease B. Diabetes mellitus C. *Dwarfism D. Acromegaly E. Cushing's disease Simmond’s disease is the result of dysphunction of: A. Hypothalamus B. *Pituitary gland C. Thyroid gland D. Adrenal gland E. Gonads What are the clinical features of Addison’s disease? A. Pale color of skin, fatigue, sexual development retardation, obesity B. Dry skin, thirst, polyuria, weight loss C. Moist skin, ophthalmic symptoms, tachycardia D. Dry skin, edemas, mental development retardation, bradycardia E. *Dark color of skin, fatigue, weight loss, hypotension What is another name of Addison’s disease? A. *Chronic adrenal insufficiency B. Congenital hypothyroidism C. Congenital adrenal hyperplasia D. Acquired hyperthyroidism E. Hyperadrenocorticism What is another name of Conn's syndrome? A. Chronic adrenal insufficiency B. *Congenital hyperaldosteronism C. Congenital adrenal hyperplasia D. Acquired hyperthyroidism E. Hyperadrenocorticism What is another name of Cushing syndrome? A. Chronic adrenal insufficiency B. Congenital hyperaldosteronism C. Congenital adrenal hyperplasia D. Acquired hyperthyroidism E. *Hyperadrenocorticism What are the clinical features of Cushing syndrome? A. *Purple striae on skin, fatigue, hirsutism, obesity B. Dry skin, thirst, polyuria, weight loss C. Moist skin, ophthalmic symptoms, tachycardia D. Dry skin, edemas, mental development retardation, bradycardia E. Dark color of skin, fatigue, weight loss, hypotension What is laboratory method of Cushing syndrome diagnostic? A. Serum calcium estimation B. Estimation of 17-ketosteroids level in urine C. Iodine excretion test D. Glucose tolerance test (GTT) 132. 133. 134. 135. 136. 137. 138. 139. 140. E. *24-hour urine test for free cortisol What laboratory method should be used to differentiate Cushing syndrome from Cushing disease? A. 24-hour urine test for free cortisol B. Estimation of 17-ketosteroids level in urine C. The measurement of 17-hydroxyprogesterone in serum D. Glucose tolerance test (GTT) E. *Dexamethasone suppression test What is laboratory method of Addison’s disease diagnostic? A. *Estimation of electrolytes and cortisol level in plasma B. Estimation of 17-ketosteroids level in urine C. The measurement of 17-hydroxyprogesterone in serum D. Glucose tolerance test (GTT) E. Dexamethasone suppression test What are the clinical features of hypothyroidism? A. Pale color of skin, fatigue, sexual development retardation, obesity B. Dry skin, thirst, polyuria, weight loss C. Moist skin, ophthalmic symptoms, tachycardia D. *Dry skin, edemas, mental development retardation, bradycardia E. Dark color of skin, fatigue, weight loss, hypotension What is another name of Grave’s disease? A. Chronic adrenal insufficiency B. Congenital hypothyroidism C. Congenital adrenal hyperplasia D. *Acquired hyperthyroidism E. Hyperadrenocorticism What is another name of mixedema? A. Chronic adrenal insufficiency B. *Acquired hypothyroidism C. Congenital adrenal hyperplasia D. Congenital hypothyroidism E. Hyperadrenocorticism What examination is the most helpful to prove the diagnosis of congenital hypothyroidism? A. Ultrasound of thyroid gland B. *Serum thyroid-stimulating hormone (TSH) C. Serum iodine D. MRI of thyroid gland E. Excretion of iodine with urine What examination is the most helpful to prove the diagnosis of endemic goiter? A. Ultrasound of thyroid gland B. Serum thyroid-stimulating hormone (TSH) C. *Serum iodine D. MRI of thyroid gland E. Excretion of cortisol with urine What are the clinical features of Grave’s disease? A. Pale color of skin, fatigue, sexual development retardation, obesity B. Dry skin, thirst, polyuria, weight loss C. *Moist skin, ophthalmic symptoms, tachycardia D. Dry skin, edemas, mental development retardation, bradycardia E. Dark color of skin, fatigue, weight loss, hypotension Choose the correct statement about hormones in Grave’s disease? A. Increase T3 and T4, increase TSH B. *Increase T3 and T4, decrease TSH Increase T3 and T4, normal TSH Decrease T3 and T4, increase TSH Normal T3 and T4, decrease TSH Choose the correct statement about hormones in congenital hypothyroidism? A. Increase T3 and T4, increase TSH B. Increase T3 and T4, decrease TSH C. Increase T3 and T4, normal TSH D. *Decrease T3 and T4, increase TSH E. Normal T3 and T4, decrease TSH What is another name of Hashimoto disease? A. *Autoimmune thyroiditis B. Acquired hypothyroidism C. Endemic goiter D. Congenital hypothyroidism E. Acquired hyperthyroidism How many hormones types are secreted with thyroid gland? A. 5 B. 4 C. 3 D. *2 E. 1 Choose the most correct definition of I stage goiter: A. No palpable or visible goiter B. *Goiter is palpable but not visible when the neck is in the normal position C. Goiter that is visible and palpable when the neck is in a normal position D. Goiter that is palpable only when neck is fully extended E. Goiter that is visible only when neck is fully extended Choose the most correct definition of II stage goiter: A. No palpable or visible goiter B. Goiter is palpable but not visible when the neck is in the normal position C. *Goiter that is visible and palpable when the neck is in a normal position D. Goiter that is palpable only when neck is fully extended E. Goiter that is visible only when neck is fully extended How many stages of goiter in endocrinology according WHO classification do you know? A. 5 B. 4 C. *3 D. 2 E. 1 What is another name of cretinism? A. Chronic adrenal insufficiency B. Acquired hypothyroidism C. Congenital adrenal hyperplasia D. *Congenital hypothyroidism E. Hyperadrenocorticism What symptom is NOT typical for Cushing syndrome? A. *Hypoglycaemia B. Moon-like face C. Hirsutism D. Striae on skin E. Acne vulgaris What symptom is NOT typical for Cushing syndrome? A. Hyperglycaemia C. D. E. 141. 142. 143. 144. 145. 146. 147. 148. 149. Moon-like face Hirsutism Striae on skin *Hypotonia What is typical symptom of mixedema? A. Polyuria B. Hirsutism C. Tachycardia D. *Cold skin E. Loss of weight What symptom is NOT typical for mixedema? A. Mental retardation B. *Hirsutism C. Bradycardia D. Cold skin E. Obesity What complication can occur after treatment with glucocorticoids? A. Diabetes insipidus B. Conn’s syndrome C. *Cushing syndrome D. Graves’ disease E. Addison’s disease What symptom is NOT typical for Grave’s disease? A. Nervousness B. Moist skin C. *Bradycardia D. Tremor E. Exophthalmia What is the typical symptom of hypoparathyroidism? A. Dry skin B. Mental retardation C. Obesity D. *Seizures E. Exophthalmia What is the typical symptom of hyperparathyroidism? A. Mental retardation B. *Osteoporosis C. Obesity D. Seizures E. Exophthalmia What can be the reason of secondary (hypogonadotropic) hypogonadism? A. *Tumor of hypophysis B. Turner syndrome C. Noonan syndrome D. Orchitis E. Klinefelter's syndrome What can be the reason of primary (hypergonadotropic) hypogonadism? A. Tumor of hypophysis B. *Turner's syndrome C. Hypopituitarism D. Laurence-Moon-Biedl syndrome E. Hypothyroidism The 2-years old boy has positive Trousseau and Hvostek symptoms, sometimes seizures, poor hair and nails growth. What is possible diagnosis? B. C. D. E. 150. 151. 152. 153. 154. 155. 156. 157. 158. Addison’s disease *Hypoparathyroidism Diabetes mellitus Grave’s disease Cushing syndrome What symptom is NOT typical for Addison’s disease? A. Bradycardia B. Hyperpigmentation C. Hypotonia D. *Mental retardation E. Vomiting All of the following are features of congenital hypothyroidism, EXCEPT: A. Lethargy B. Prolonged jaundice C. *Persistent diarrhea D. Hoarse cry E. Feeding difficulties All of the following are features of Addison's disease, EXCEPT: A. Weakness B. Anorexia C. Hypoglycemia D. *Hypertension E. Hyperpigmentation of the skin What types of diabetes mellitus glycemic control do you know? A. *Ideal, optimal, suboptimal, high risk for the life B. Normal, subnormal, poor, high risk for the life C. Excellent, problematic, suboptimal, high risk for the life D. Very good, good, bad, terrible E. Satisfactory, unsatisfactory What is NOT included in the clinical diagnose of diabetes mellitus type 1? A. Severity B. Glycemic control C. Type of diabetes mellitus D. *Stage E. Complications What is the most frequent endocrine pathology in children? A. Diabetes mellitus B. Addison’s disease C. *Goiter D. Grave’s disease E. Dwarfism What is term which describes frequent urinations? A. *Pollakiuria B. Nicturia C. Polyuria D. Oliguria E. Hypoisostenuria What is typical for diabetes insipidus? A. Glucosuria B. Proteinuria C. Oliguria D. *Hypoisostenuria E. Ketonuria What can be the reason of diabetes mellitus? A. B. C. D. E. 159. 160. 161. 162. 163. 164. 165. 166. 167. Excessive intake of sweets Stress Heredity Pancreatitis *All is correct What can be the reason of diabetes insipidus? A. Excessive intake of sweets B. *Tumor of hypophysis C. Tumor of adrenal gland D. Pancreatitis E. All is correct What is the most informative laboratory index about diabetes mellitus control? A. Glucose in blood B. Glucose in urine C. Cholesterol in blood D. *Glucosylated hemoglobin E. Protein in urine What food should be limited for the first time in patients with diabetes mellitus? A. Meat B. Seafood C. Milk D. Vegetables E. *Fruits What is dose of glucose for glucose tolerance test (GTT)? A. 0,75 grams/kg B. 1 gram/kg C. *1,75 grams/kg D. 2 grams/kg E. 2,5 grams/kg What minimal 2-hours glucose level in blood indicates diabetes mellitus according glucose tolerance test (GTT)? A. More than 8,5 mmol/L B. More than 9,0 mmol/L C. *More than 11,1 mmol/L D. More than 14,0 mmol/L E. More than 16,1 mmol/L What minimal fasting plasma glucose level in blood indicates diabetes mellitus according glucose olerance test (GTT)? A. More than 5,5 mmol/L B. *More than 7,0 mmol/L C. More than 7,7 mmol/L D. More than 8,0 mmol/L E. More than 11,0 mmol/L What is not typical for diabetes mellitus? A. Pollakiuria B. Nicturia C. Polyuria D. *Oliguria E. Glucosuria What is term which describes increased amount of urine? A. Pollakiuria B. Nicturia C. *Polyuria D. Oliguria A. B. C. D. E. 168. 169. 170. 171. 172. 173. 174. 175. 176. 177. 178. 179. 180. 181. 182. 183. 184. E. Anuria What symptom is NOT typical for diabetes mellitus type 2? A. Polyuria B. Weakness C. Polydipsia D. Dry skin E. *Loss of weight What symptom is not typical for diabetes mellitus type 1? A. Polyuria B. *Hirsutism C. Polydipsia D. Dry skin E. Loss of weight What is the best laboratory method to prove diabetes mellitus diagnosis if blood glucose level is controversial? A. Estimation of insulin level in plasma B. Estimation of glucose level in urine C. Insulin tolerance test D. *Glucose tolerance test (GTT) E. Estimation of glucose level in blood several times What is screening laboratory method of diabetes mellitus diagnostic? A. Estimation of insulin level in plasma B. Estimation of glucose level in urine C. Insulin tolerance test D. Glucose tolerance test (GTT) E. *Estimation of glucose level in blood What are the laboratory signs of diabetic ketoacidosis? A. Hyperglycaemia, glucosuria, hyperbilirubinemia B. Hyperglycaemia, glucosuria, proteinuria C. *Hypoglycaemia, glucosuria, ketonuria D. Acidosis, normoglycaemia, ketonuria E. Hyperglycaemia, glucosuria, ketonuria The antagonist of insulin is: A. Thyroxin B. Cortisol C. *Glucagon D. Prolactin E. Growth hormone What is the place of insulin synthesis in pancreas? A. Follicular cells B. Lutein cells C. Interstitial cells of Leydig D. *The islets of Langerhans E. Medullar substance What should be an initial intravenous bolus dose of regular insulin in diabetic coma? A. 0.01 U/kg body weight B. *0.1 U/kg body weight C. 1 U/kg body weight D. 1, 5 U/kg body weight E. Insulin should not be injected intravenously What should be dose of regular insulin for continuous intravenous infusion in diabetic coma? A. 0.01-0,02 U/kg/hour B. *0.1-0,2 U/kg/hour 0.1-0,2 U/kg/day 1-2 U/kg/hour 1-2 U/kg/day What is the criterion of blood glucose level in diabetic coma to start subcutaneous injections? A. Less than 7 mmol/L B. Less than 10 mmol/L C. *Less than 14 mmol/L D. Less than 18 mmol/L E. Less than 20 mmol/L What should NOT be included in the clinical diagnose of DM in children? A. Severity B. Type C. Level of glycemic control D. *Symptoms E. Complications What should be included in the clinical diagnose of DM in children? A. Stage of disease B. Etiologic factor C. *Severity D. Symptoms E. Insulin dose To estimate severity of the DM doctor should be informed about: A. Presence of comas on anamnesis B. Presence of acute complications C. Current patient’s treatment D. Presence of chronic complications E. *All is correct To estimate the severity of the DM doctor doesn’t need to be informed about: A. Presence of chronic complications B. Presence of acute complications C. *Age of patient D. Presence of ketoacidosis and comas in anamnesis E. Current patient’s treatment What maximal fasting glycemia in diabetic patient is appropriate for the ideal glycemic control? A. 2,2 – 5,5 mmol/L B. *3,6 – 6,1 mmol/L C. 4,0 - 7,0 mmol/L D. 8,0 – 9,0 mmol/L E. More than 9,0 mmol/L What maximal fasting glycemia in diabetic patient is appropriate for the optimal glycemic control? A. 2,2 – 5,5 mmol/L B. 3,6 – 6,1 mmol/L C. *4,0 - 7,0 mmol/L D. 8,0 – 9,0 mmol/L E. More than 9,0 mmol/L What maximal fasting glycemia in diabetic patient is appropriate for the suboptimal glycemic control? A. 2,2 – 5,5 mmol/L B. 3,6 – 6,1 mmol/L C. 4,0 - 7,0 mmol/L D. *8,0 – 9,0 mmol/L C. D. E. 185. 186. 187. 188. 189. 190. 191. 192. 193. 194. 195. 196. 197. 198. 199. 200. E. More than 9,0 mmol/L What fasting glycemia in diabetic patient is appropriate for the high risk for the life glycemic control? A. 2,2 – 5,5 mmol/L B. 3,6 – 6,1 mmol/L C. 4,0 - 7,0 mmol/L D. 8,0 – 9,0 mmol/L E. *More than 9,0 mmol/L What maximal after food glycemia in diabetic patient is appropriate for the ideal glycemic control? A. 3,6 – 6,1 mmol/L B. *4,4 – 7,0 mmol/L C. 5,0 - 11,0 mmol/L D. 11,0 – 14,0 mmol/L E. More than 14,0 mmol/L What maximal after food glycemia in diabetic patient is appropriate for the optimal glycemic control? A. 3,6 – 6,1 mmol/L B. 4,4 – 7,0 mmol/L C. *5,0 - 11,0 mmol/L D. 11,0 – 14,0 mmol/L E. More than 14,0 mmol/L What maximal after food glycemia in diabetic patient is appropriate for the suboptimal glycemic ontrol? A. 3,6 – 6,1 mmol/L B. 4,4 – 7,0 mmol/L C. 5,0 - 11,0 mmol/L D. *11,0 – 14,0 mmol/L E. More than 14,0 mmol/L What after food glycemia in diabetic patient is appropriate for the high risk for the life glycemic ontrol? A. 3,6 – 6,1 mmol/L B. 4,4 – 7,0 mmol/L C. 5,0 - 11,0 mmol/L D. 11,0 – 14,0 mmol/L E. *More than 14,0 mmol/L What maximal glycated hemoglobin (Hb Alc) level is appropriate for the ideal glycemic control in iabetic patient? A. Less then 4, 0 % B. Less than 5,0 % C. *Less than 6,0 % D. Less than 7,6 % E. Less than 9,0 % What maximal glycated hemoglobin (Hb Alc) level is appropriate for the optimal glycemic control in diabetic patient? A. Less then 4, 0 % B. Less than 5,0 % C. Less than 6,0 % D. *Less than 7,6 % E. Less than 9,0 % What maximal glycated hemoglobin (Hb Alc) level is appropriate for the suboptimal glycemic control in diabetic patient? A. Less then 4, 0 % B. Less than 5,0 % Less than 6,0 % Less than 7,6 % *Less than 9,0 % What symptom is NOT typical for the Nobekur’s syndrome? A. Growth retardation B. *Obesity C. Diabetic hepatosis D. Sexual development retardation E. All symptoms are typical for this syndrome C. D. E. 201. 202. 203. 204. 205. 206. 207. 208. 209. Which lymph nodes enlargement is usually NOT caused by hematological disease? A. Anterior cervical B. Posterior cervical C. * Preauricular D. Submandibular E. Supraclavicular What concomintant problem is NOT typical for children with Down’s syndrome ? A. Hodgkin's disease B. Non-Hodgkin's lymphoma C. Myeloid leukemia D. Neuroblastoma E. * Ependymoma In plan of examination of patient with non-Hodgkin’s lymphoma should be included all EXCEPT: A. * Bronchoscopy B. Bone biopsy C. MRI D. CT-scan E. CBC For acute lymphocytic leukemia is NOT typical: A. Skin haemorrhages B. Fever C. Marked elevation in WBCs D. * Pain in epigastric region E. Long bones pain Choose the wrong statement about acute myelocytic leukemia: A. Bone marrow examination is essential diagnosis B. More common in adult C. It is worse prognosis than chronic myeloid leukemia D. Persons with Down’s syndrome have higher risk of AML development E. *All is correct Philadelphia chromosome is observed in more than 70 % patiens with: A. * Chronic myeloid leukemia B. Acute lymphoid leukemia C. Hodgkin’s lymphoma D. Acute myeloid leukaemia E. Chronic lymphoid leukaemia Philadelphia chromosome is usually NOT observed in patients with: A. Chronic myeloid leukemia B. Acute lymphoid leukemia C. * Hodgkin’s lymphoma D. Acute myeloid leukaemia E. Chronic lymphoid leukaemia The treatment of leukaemia should be started with: Maintenance of remission Consolidation of remission * Induction of remission Subclinical CNS leukemia prophylaxis Prophylaxis of relapse On the second year of leukaemia treatment should be started stage of: A. Maintenance of remission B. Subclinical CNS leukemia prophylaxis C. Induction of remission D. * Consolidation of remission E. Prophylaxis of relapse On the third year of leukaemia treatment should be started stage of: A. * Maintenance of remission B. Consolidation of remission C. Induction of remission D. Subclinical CNS leukemia prophylaxis E. Prophylaxis of relapse A. B. C. D. E. 210. 211. 212. Choose normal count of reticulocytes in peripheral blood in adults: A. * Not more than 1 % B. Not more than 5 % C. Not more than 25 % D. Not more than 35 % E. Not more than 50 % 213. We diagnose increased level of lymphoblasts in bone marrow if their content is: A. more than 2 % B. more than 3 % C. * more than 5 % D. more than 20 % E. more than 50 % Diagnostic criterion of leukemia in bone marrow is: A. Any number of lymphoblasts (they should be absent in healthy) B. More than 5 % of lymphoblasts C. More than 10 % of lymphoblasts D. * More than 25 % of lymphoblasts E. More than 50 % of lymphoblasts Choose the examination which can finally prove leukemia: A. Lymph node biopsy B. CT-scan C. Complete blood count D. * Bone marrow puncture E. Lumbar puncture All the following are poor prognostic signs in leukemia EXCEPT of: A. High WBC count B. Presence of chromosomes translocations C. Blasts with T-cell phenotype. D. Age less than 1 year old E. * All of above means poor prognosis All the following are good prognostic signs in leukemia EXCEPT of: A. Low WBC count B. Absence of L3 cells C. Platelet count greater 100 G/L D. * Presence of chromosomes translocations E. All of above means good prognosis What pathology is usually characterized by atrophyc glossitis: 214. 215. 216. 217. 218. Hodgkin’s lymphoma Chronic leukemia leukemia * B12-deficiency anemia Iron-deficiency anemia Allergic vasculitis What index does demonstrate the effectiveness of the iron-deficiency anaemia treatment? A. The serum iron level B. * The serum ferritin level C. The hemoglobin level D. The total iron-binding capacity E. Hemoglobin electrophoresis The haemoglobin level 160 g/L is typical for: A. * Neonates B. Tree months old infants C. Teenagers D. Young adult male E. Pregnant woman What is NOT typical for aplastic anemia? A. Can be caused by drugs B. There is decreased platelet counts C. * Bone marrow may show increased number of megakaryocytes D. Bone marrow may show decreased red cell formation E. Can be elevation of serum iron Small size of erythrocytes is NOT typical for: A. Iron deficiency anemia B. alfa thalassemia major C. beta thalassemia minor D. * G6PD deficiency E. anemia of chronic disease Decreased color index is NOT typical for: A. Iron deficiency anemia B. alfa thalassemia major C. beta thalassemia minor D. * G6PD deficiency E. anemia of chronic disease What is correct about the anemia of chronic disease: A. Blasts are elevated in bone marrow B. Serum iron level is decreased C. Serum iron-binding capacity is elevated D. * Marrow iron stores are increased E. Iron therapy is required to raise hemoglobin level One of etiological factors of hemolytic-uremic syndrome is: A. Staphylococcus aureus B. * E. coli C. Streptococcus viridans D. Candida E. Proteus What problem is NOT associated with an intracorpuscular defect of erythrocytes: A. Hereditary sherocytosis B. Sickle cell anemia C. * Autoimmune hemolytic anemia D. G6PD deficiency E. Hereditary elliptocytosis A. B. C. D. E. 219. 220. 221. 222. 223. 224. 225. 226. 227. 228. 229. 230. 231. 232. 233. 234. 235. What is NOT typical for the Fanconi’s anemia? A. * Hematologic abnormalities in infancy B. Pancytopenia C. Skeletal abnormalities D. Chromosome fragility E. Renal abnormalities We can diagnose anemia in children between 6 month to 5 years old in case if: A. * Haemoglobin below 11 g/L B. Haemoglobin below 12 g/L C. Haemoglobin below 13 g/L D. Haemoglobin below 14 g/L E. Haemoglobin below 15 g/L We can diagnose anemia in children older 5 years old in case if: A. * Haemoglobin below 12 g/L B. Haemoglobin below 13 g/L C. Haemoglobin below 14 g/L D. Haemoglobin below 15 g/L E. Haemoglobin below 16 g/L What disease is NOT characterized by hypochromia and microcytosis? A. Pyridoxine responsive anemia B. * Sickle cell disease C. Dyserythropoietic anemia D. Lead poisoning E. Beta thalassemia major What disease is characterized by hypochromia and microcytosis? A. Iron deficiency B. Beta thalassemia major C. Pyridoxine responsive anemia D. Lead poisoning E. * All is correct What disease is characterized by normochromic, normocytic anemia: A. Iron deficiency B. Beta thalassemia major C. Hemolytic disesase of newborns D. Lead poisoning E. * Fanconi’s anemia What is the best method to prove thalassemia diagnosis? A. Serum iron and iron binding capacity B. Liver biopsy C. * Hemoglobin electrophoresis D. Coomb’s test E. Coagulogram Presence of the increased RBCs production before treatment is typical for: A. B12 deficient anemia B. * Hereditary Spherocytosis C. Aplastic anemia D. Anemia of chronic disease E. Megaloblastic anemia Sickle cell anemia is not characterized by: A. Reticulocytosis B. Jaundice C. * Hypochromia of erythrocytes D. Splenic sequestration E. Acute chest syndrome 236. 237. 238. 239. 240. 241. 242. 243. 244. What hemoglobin type do we need to find in blood diagnose beta thalassemia trait? A. Hb-S B. Hb-C C. * Hb-A2 D. Hb-A E. Hb-C2 What is NOT typical for thalassemia major? A. Jaundice B. Target cells on peripheral smear C. Microcytic hypochromic anemia D. * Hemorrhagic syndrome E. Growth failure Choose the important link of hemostasis: A. Vascular integrity B. Qualitative and quantative characteristics of platelets C. Presence of coagulation factors in blood D. All is incorrect E. * All is correct What is Schonlein-Henoch purpura? A. Hemolytic-uremic syndrome B. Von Willebrand disease C. * Anaphylactoid purpura D. Fanconi pancytopenia E. Allergic dermatitis What is NOT another name of hemorrhagic vasculitis? A. * Hemolytic-uremic syndrome B. Schonlein-Henoch purpura C. Allergic angiitis D. Anaphylactoid purpura E. Henoch-Schonlein disease The prolonged bleeding time is NOT typical for the: A. * Hemophilia B B. von Willebrand’s disease C. Aspirin-induced thrombocytopathia D. Bernard-Soulier syndrome E. ITP What of the following is NOT typical for DIC? A. Thrombocytopenia B. Microangiopathic blood smear C. Hypofibrinogenemia D. Hemorrhagic syndrome E. * All of above typical for this disease In case of acute onset of thrombocytopenia in children we have to think first of all about: A. von Willebrand disease B. Acute leukemia C. * Idiopathic (immune) thrombocytopenic purpura D. Aplastic anemia E. Thrombotic thrombocytopenic purpura Find the INCORRECT statement concerning ITP in children: A. 60 to 80 % of children who present with acute ITP will have spontaneous resolution of their ITP ithin 6 mo B. Less than 1 % will develop intracranial hemorrhage C. About 10 to 20 % of children who present with acute ITP go on to develop chronic ITP The presence of abnormal finding such as hepatosplenomegaly or remarkable lymphadenopathy uggests another diagnosis E. * Level of platelets in the blood can be normal Find the INCORRECT statement concerning ITP in children: A. 60 to 80 % of children who present with acute ITP will have spontaneous resolution of their ITP ithin 6 mo B. Intracranial hemorrhage is very rare complication of acute ITP C. About 60 to 80 % of children who present with acute ITP go on to develop chronic ITP D. All statements are wrong E. * All statements are correct The criterion of trombocytopenia in blood according to the level of platelets is: A. Less than 250,000/mm3 B. Less than 180,000/mm3 C. * Less than 150,000/mm3 D. Less than 100,000/mm3 E. Less than 50,000/mm3 What is typical for the acute ITP? A. Anemia and thrombocytopenia B. * Isolated thrombocytopenia C. Thrombocytopenia and leukocytosis D. Positive Coomb’s test E. Presence of blasts in peripheral blood What is typical for acute ITP in bone marrow: A. * Normal granulocytic and erythrocytic series with increased number of megakaryocytes B. Decreased granulocytic, erythrocytic and megakaryocytic series C. Increased granulocytic, erythrocytic and megakaryocytic series D. Decreased granulocytic and erythrocytic series with increased number of megakaryocytes E. Increased granulocytic and erythrocytic series with decreased number of megakaryocytes What will be abnormal in plasma if patient has decreased VII plasma coagulation factor? A. Platelets count B. Prothrombin time C. * Clotting time D. Amount of fibrinogen E. Bleeding time What will be abnormal in plasma if patient has decreased IX plasma coagulation factor ? A. * Partial thromboplastin time B. Thrombin time C. Clotting time D. Amount of fibrinogen E. Bleeding time What kind of rush is typical for ITP? A. Polymorphous B. Polychromatic C. Asymmetric D. Petechiae and purpura E. * All is correct What kind of rush is NOT typical for ITP? A. Polymorphous B. Polychromatic C. * Symmetric D. 245. 246. 247. 248. 249. 250. 251. 252. Petechial Purpuric What statement is NOT correct about treatment of ITP in children? A. It doesn’t require treatment B. * Children who have platelet counts > 30,000/mm3 and are asymptomatic or have only minor purpura do not require routine treatment C. Children who have platelet counts < 10,000/mm3 and are asymptomatic or have only minor purpura do not require routine treatment D. Treatment doesn’t depend on the platelets level and is performed only in bleedings E. Clotting time is increased in 30 % of patients Choose the best combination of medicnes for ITP treatment: A. * Intravenous immune globulin (IVIG) and prednisone B. Antibiotics and non-steroid anti-inflammatory C. Slow acting antirheumatoid drugs (SAARDS) and cytostatics D. Antibiotics and cytostatics E. Non-steroid anti-inflammatory drugs and antibiotics What is usual dose of prednisolon for children? A. 0,5-1 mg/ kg/day B. * 1-2 mg/ kg/day C. 5-10 mg/ kg/day D. 10-15 mg/ kg/weekly E. more than 20 mg/ kg/day What is NOT part of recommendations for children with acute ITP? A. Restriction of physical activities B. Avoidance of aspirin C. Avoidance of intramuscular injections D. * Daily massages E. Hypoallergic diet When is recommended to perform splenectomy in the forth stage of ITP? A. Newborns B. Infants C. 1-2 years D. 3-4 years E. * After 6 years What platelets level in ITP is dangerous for development of intracranial hemorrhages? A. More 50,000/mm3 B. Below 50,000/mm3 C. More 20,000/mm3 D. * Below 20,000/mm3 E. Below 100,000/mm3 Typical triade of Wiskott-Aldrich syndrome is: A. Thrombocytopenia, mental retardation and immunodeficiency B. Thrombocytosis, mental retardation and immunodeficiency C. * Thrombocytopenia, eczema and immunodeficiency D. Thrombocytosis, eczema and immunodeficiency E. Thrombocytopenia, eczema and seizures Thrombocytopathia and thrombocytopenia are typical for: A. Hemorrhagic vasculitis B. Hemophilia C. Idiopathic thrombocytopenic purpera D. Aplastic anemia E. * Bernard Soulier syndrome D. E. 253. 254. 255. 256. 257. 258. 259. 260. 1. 2. 3. 4. 5. Blood and endocrine system diseases Ситуаційні задачі The 8-years old girl notes the pain in left foot joint. She had upper respiratory tract viral infection a week before. Objectively: the joint is moderately edematous, painful during palpation and movements, skin is normal. The joint size became normal on the background of anti-inflammatory therapy, but pain remained, mostly at night. Spleen enlargement and lymphadenopathy also appeared. General blood test results: anemia, leucocytosis and lymphocytosis. The most reasonable is to perform the following examination: A. Level of platelets B. Lymph node puncture C. *Sternal puncture D. Acute inflammation reactants E. Joint puncture The 6 years old boy has been treated because of stomatitis during 10 days, but on background of treatment has increased intoxication, ulceration of oral cavity, appeared nasal bleeding, hepatosplenomegaly. In general blood test: Hb - 70 g/l, leukocytes – 30 T/L, blasts - 28%, bands - 2%, segments - 18%, lymphocytes - 51%, monocytes - 1%, platelets – 68 G/L, ESR - 42 mm/hour. What is the most probable diagnosis? A. Chronic leukemia B. Sepsis C. *Acute leukemia D. Systemic lupus erythematosus E. Thrombocytopenic purpura The 10-years old girl was admitted to hospital with complains of general malaise, weakness, weight loss, increased temperature to 39 С, pain along the bones, mainly at night, which is not suppressed by analgesics, hemorrhagic rash on legs. She is ill during 1 month. The disease has begun after overcooling. Objectively: dystrophy, skin is pale, on legs and abdomen are petechia and ecchymoses; all groups of lymph nodes are enlarged; spleen enlarged, hepatomegaly, joints are not changed. What is the most probable diagnosis? A. Hemorrhagic vasculitis B. Sepsis C. *Acute leukemia D. Rheumatic fever E. Systemic lupus erythematosus The 7-years old boy during 6 months is treated because of acute leukemia, has received ALL BFM-protocol. Now he is receiving supporting therapy by methothrexat and 6mercaptopurin; complaints are absent. In general blood analysis: Hb - 100 g/L, leukocytes - 6,0 T/L, thrombocytes – 140 G/L, ESR - 12 mm/hour. What amount of lymphocytes in peripheral blood will confirm the remission? A. less than 20 % B. less than 30 % C. less than 40 % D. *less than 50 % E. less than 60 % The 6-year old boy is treated in hematological department because of acute leukemia. In general blood analysis: Hb - 64 g/L, thrombocytes – 90 G/L, leukocytes – 28 T/L, blasts - 52%, segments - 4%, lymphocytes - 41%, monocytes - 3%, ESR - 46 mm/hour, in myelogram: blasts - 70%, significant suppression of erythrocytes and thrombocytes formation. The child receives medicines according to the treatment protocol. What of the following is necessary to use intrathecal for neuroleukemia prevention? A. *Methotrexate B. Vincristin Prednison Cyclophosphamid Cytosar The 4-year old girl had influenza during three days. For the moment of examination her condition became worse: she is weak, drowsy, does not want to eat. Objectively: skin is pale with jaundice; sclera and visible mucous membranes are yellow, tachycardia, liver enlarged, spleen is palpable. In anamnesis were noted mild manifestations of jaundice; was treated surgically because of right hand polydactylia. In general blood analysis: Hb 76g/L, color index – 1,1, reticulocytes – 19 %, microspherocytosis. What disease is the most probable in this case? A. Cooley’s disease B. Fankoni anemia C. *Minkovsky-Chauffard disease D. Gained hemolytic anemia E. Viral hepatitis The 3-years old boy has severe anemia, jaundice, numerous disembriogenetic stigmas, microphthalmia and moderate hepatosplenomegaly. Microspherocytic hemolytic anemia is suspected. What from this is reasonable to perform to prove the diagnosis? A. Hemoglobin level B. Bilirubin level C. *Osmotic resistance of erythrocytes D. Coombs' test E. Reticulocytes level In patient with Burkitt's lymphoma who has chemotherapy developed hyperpotassemia, hypocalcemia, hyperphosphatemia, and hyperuricemy. What is the most possible reason? A. Bad response to therapy B. Complication of poorly treated disease C. *Development of hepatic metastasis D. Toxicity of chemotherapeutic agents E. Tumor lysis syndrome The 3 months old boy was admitted to hospital in severe condition because of neurological signs: muscles hypotonia, convulsions, and positive meningeal signs. Also is present skin pallor with jaundice, small hemorrhages on the abdomen, tachycardia, hepatosplenomegaly, edema of eyelids, anuria more than 6 hours. 3 days ago the child has dyspeptic manifestations, which mother treated by herself. What diagnosis is the most reliable? A. Acquired autoimmune hemolytic anemia B. Viral hepatitis C. Minkovsky-Chauffard disease D. *Hemolytic-uremic syndrome E. Bacterial meningitis The family of a child just diagnosed with acute lymphoblastic leukemia asks for information about the child’s prognosis. Included as a poor prognostic sign is which of the following? A. *Presence of a mediastinal mass B. Hyperdiploidy with more than 50 chromosomes C. White blood cell count at diagnosis of less than 100,000 mm3 D. Age between 1 and 10 years E. Early pre-B-cell variety of the disease While bathing her 2-year-old son, a mother feels a mass in his abdomen. A thorough medical evaluation of the child reveals aniridia, hypospadias, horseshoe kidney, and hemihypertrophy. The most likely diagnosis for this child is: A. Neuroblastoma B. *Wilms tumor C. D. E. 6. 7. 8. 9. 10. 11. Hepatoblastoma Rhabdomyosarcoma Testicular cancer An 8-year-old child being treated with a combination of chemotherapy agents develops very red, inflamed sores in the mouth and esophagus. He has difficulty eating and drinking food and liquids. Which of the following antineoplastic agents is the most likely etiology? A. Vincristine B. Prednisone C. *Methotrexate D. 6-mercaptopurine E. Doxorubicin (Adriamycin) Which recommendation is correct for the prevention of iron deficiency anemia in children? A. Don’t give breastfeeding for children elder than 6 months B. Oral iron supplements for all children between two and 10 years of age C. *For artificial feeding use only iron-fortified infant formula D. Give whole cow's milk after six months of age E. Give iron supplement for all breastfeeding infants An otherwise healthy 17-year-old complains of swollen glands in his neck and groin for the last 6 months and an increasing cough over the previous 2 weeks. He also reports some fevers, especially at night, and possibly some weight loss. On examination, you notice that he has nontender cervical, supraclavicular, axillary, and inguinal nodes, no hepatosplenomegaly, and otherwise looks to be fairly healthy. Which of the following would be the appropriate next step? A. Biopsy of a node B. Complete blood count and differential C. Trial of antituberculous drugs D. *Chest radiograph E. Cat-scratch titers A 7-year-old patient with known hereditary spherocytosis presents with pallor, lowgrade fever, and splenomegaly. Blood counts are as follows: hemoglobin 3 g/dl, reticulocyte count 2%, white blood cell count 8000/mm3, and platelet count 200,000/ mm3. The most likely diagnosis is: A. Acute splenic sequestration crisis B. *Aplastic crisis C. Hemolytic crisis D. Acute leukemia E. Superimposed iron deficiency Further hematologic evaluation is indicated for: A. *A full-term newborn with a hemoglobin level of 12 g/L B. A 2-month-old infant with a hemoglobin level of 10 g/L C. A 2-year-old child with a platelets level of 200 000 / mm3 D. A full-term newborn with a reticulocytes level of 3% E. A 14-years-old girl with a hemoglobin level of 13 g/L On a routine-screening complete blood count, a 1-year-old is noted to have a microcytic anemia. A follow-up hemoglobin electrophoresis demonstrates an increased concentration of hemoglobin A2. The child is most likely to have: A. Iron deficiency B. *Beta thalassemia trait C. Sickle cell anemia D. Chronic systemic illness E. Lead poisoning A 4-year-old previously well boy develops pallor, dark urine, and jaundice. There has C. D. E. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. been no apparent exposure to a jaundiced person or to any toxins. He is taking trimethoprim-sulfamethoxazole for otitis media. You consider the possibility of a hemolytic crisis caused by glucose-6- phosphate dehydrogenase (G6PD) deficiency. In which of the following ethnic groups is the incidence LOWEST? A. African American B. Greek C. Chinese D. Middle Eastern E. *Scandinavian On a routine newborn screen, a 2-week-old child in your clinic is noted to have sickle cell disease. As you discuss treatment options with this family, you recommend: A. Monthly injections of vitamin B12 B. Tetracycline prophylaxis C. Meningococcal vaccine at 2, 4, and 6 months of age D. *Education of parents regarding abdominal palpation and temperature taking E. Infusion of immunoglobulin every 6 weeks A 2950-g black baby boy is born at home at term. On arrival at the hospital, he appears pale, but the physical examination is otherwise normal. Laboratory studies reveal the following: mother’s blood type A, Rh positive; baby’s blood type O, Rh-positive; hematocrit 38%; reticulocyte count 5%. Which of the following is the most likely cause of the anemia? A. *Fetomaternal transfusion B. ABO incompatibility C. Physiologic anemia of the newborn D. Sickle cell anemia E. Iron-deficiency anemia A preterm black male infant was found to be jaundiced 12 h after birth. At 36 h of age, his serum bilirubin was 18 mg/dL, haemoglobin concentration was 12.5 g/dL, and reticulocyte count 9%. Many nucleated red cells and some spherocytes were seen in the peripheral blood smear. The differential diagnosis should include which of the following? A. Pyruvate kinase deficiency B. *Hereditary spherocytosis C. Sickle cell anemia D. Rh incompatibility E. Polycythemia On a routine well-child examination, a 1-year-old boy is noted to be pale. He is in the seventy-fifth percentile for weight and the twenty-fifth percentile for length. Results of physical examination are otherwise normal. His hematocrit is 24%. Of the following questions, which is most likely to be helpful in making a diagnosis? A. *What is the child’s usual daily diet? B. Did the child receive phototherapy for neonatal jaundice? C. Has anyone in the family received a blood transfusion? D. Is the child on any medications? E. What is the pattern and appearance of his bowel movements? You are asked to see a 5-week-old baby whose birth weight was 1.360 kg, he was born after 34 weeks of gestation. Delivery was normal and his haemoglobin at birth was normal. The baby has fed and gained weight well. Hower, his haemoglobin is now 80 g/L. You would expect the anemia to be due: A. *Physiological increase in blood volume B. Lack of iron in the diet C. Congenital infection D. Increased fragility of blood cells E. Lack of iron absorption 24. 25. 26. 27. 28. 29. An 11-monthold boy presents with pallor. There is no bruising or hepatosplenomegaly. His mother is of Italian and his father is of English origin. His haemoglobin is 75 g/L. The blood film shoes hypochromic microcytic red cells and the white cells show normal morphology. Which of the following is correct? A. This disease is a sex-linked disorder B. *A dietary history is very important C. Long term treatment with blood transfusion will be required D. A bone marrow examination is indicated E. Such hemoglobin level is normal for his age An infant or young child with hemolytic anemia, which was undergone splenectomy, has an increase risk of: A. Thrombocytosis B. Polycytemia C. Leukemia D. *Severe bacterial infection E. Hemorrhages Having performed a complete history and physical examination on the 1-year-old boy with skin paleness, you proceed with a diagnostic workup. Initial laboratory results are as follows: hemoglobin 8 g/dL; hematocrit 24%; leukocyte count 11,000/mm3 with 38% neutrophils, 7% bands, 55% lymphocytes; hypochromia on smear; free erythrocyte protoporphyrin (FEP) 110 mkg/dL - normal; lead level 7 mkg/dL (should be less than 10 mkg/dL), whole blood; platelet count adequate; reticulocyte count 0.5%; sickle cell preparation negative; stool guaiac negative; and mean corpuscular volume (MCV) 65 fl. You would most appropriately recommend A. Blood transfusion B. *Oral ferrous sulfate C. Intramuscular iron dextran D. An iron-fortified cereal E. Calcium supplements In the 12-years old girl are developed signs of tracheobronchitis, Raynaud's syndrome, vomiting and abdominal pain after prolonged overcooling. Objectively: skin and sclera jaundice, hepatosplenomegaly. Examination results: positive direct and indirect Coombs' test, moderate anemia, increased indirect bilirubin level. What diagnosis is the most reliable? A. Minkovsky-Chauffard disease B. Cooley’s disease C. *Acquired autoimmune hemolytic anemia D. Sickle cell anemia E. Viral hepatitis A 5-year-old child was diagnosed idiopathic (immune) thrombocytopenic purpura. Appropriate treatment of this child includes: A. *Intravenous gamma globulin B. Platelet transfusion C. Aspirin therapy D. Factor VIII infusion E. Prednisone, vincristine, and asparaginase induction followed by methotrexate and 6-mercaptopurine A newborn infant is born with petechiae scattered across his body. His platelet count is noted to be 22,000 per cu.mm with hemoglobin of 12 mg/dL. Which of the following is most likely to explain this infant’s condition? A. *Congenital cytomegalovirus infection B. Uncomplicated prematurity C. Chlamydial conjunctivitis D. Maternal ingestion of aspirin 30. 31. 32. 33. 34. 35. E. Nasolacrimal duct stenosis During a routine-screening CBC, a 1-year-old is noted to have eosinophilia. Which of the following most commonly causes increased eosinophilia in the peripheral blood smear? A. Bacterial infections B. Chronic allergic rhinitis C. Fungal infections D. *Helminth invasion E. Tuberculosis A 10-year-old boy is admitted to the hospital because of bleeding. Pertinent laboratory findings include a platelet count of 50,000/mm3, prothrombin time (PT) of 15 s (control 11.5 s), activated partial thromboplastin time (aPTT) of 51 s (control 36 s), thrombin time (TT) of 13.7 s (control 10.5 s), and factor VIII level of 14% (normal 38 to 178%). The most likely cause of his bleeding is: A. Immune thrombocytopenic purpura (ITP) B. Vitamin K deficiency C. *Disseminated intravascular coagulation (DIC) D. Hemophilia A E. Hemophilia B You examine the 7 years old girl with complains of numerous hemorrhagic rashes on limbs and face, that had appeared suddenly in the morning. Rush is painless. Yesterday she had nasal bleeding. From anamnesis: 2 weeks ago she has recovered from respiratory infection. What is the most probable diagnosis? A. Allergic dermatitis B. *ITP C. Chicken pox D. Hemorrhagic vasculitis E. DIC-syndrome The girl is 10 years old. She is hospitalized with numerous petechial rashes on limbs, trunk; the rush elements are different in size and in color. Thrombocytopenic purpura is suspected. What in blood analysis will confirm the diagnosis? A. Leucocytosis B. Increased ESR C. *Prolonged time of the bleeding D. Prolonged time of coagulation E. Reduction of thrombocytes adhesive activity The 8 years old girl suffering from idiopathic thrombocytopenic purpura during 1,5 years, she has often relapses. She received glucocorticoids before. In the general blood analysis: RBC 3,0 millions in mm3, Hb 88 g/l, thrombocytes 49,000-68,000 /mm3. What should be the next treatment step? A. Glucocorticoids in high doses B. Transplantation of the bone marrow C. *Intravenous immune globulin (IVIG) D. Spleenectomy E. Cytostatics The 10 years old boy complains of periodic nasal bleedings, bruises on legs, hips, forearms. Objectively: skin is pale, on limbs - hemorrhagic rashes of different size and color. Other organs and systems are normal. The liver margin is on the level of right costal arch, spleen is not enlarged. What is the most probable diagnosis? A. Von Willebrand's disease B. Hemophilia C. *ITP D. Schoenlein-Henoch purpura E. DIC-syndrome 36. 37. 38. 39. 40. 41. 42. The girl, 10 years old, has addressed to physician with complains of numerous hemorrhagic rashes on limbs, trunk, which appeared without any reason. Two weeks ago she has recovered from viral infection. Thrombocytopenic purpura is suspected. What therapy is necessary to prescribe this child? A. Heparin B. Acetylsalicylic acid C. *Prednisolon D. Crioplasm E. Azathioprin The 5 years old boy is hospitalized in clinic because of long (during 2 days) bleeding after tooth extraction. In anamnesis he has nasal bleedings, bruises on abdomen, and back often. His mother has metrorrhagias sometimes. In the general blood analysis: RBC 2,8 millions/mm3, Hb 86g/L, thrombocytes 196000/mm3, time of bleeding is 12 minutes, time of coagulation is 5 minutes. What is the most probable diagnose? A. Shoenlein-Genoch's disease B. Hemophilia C. Thrombocytopenic purpura D. *Von Willebrand's disease E. DIC-syndrome The girl, 7 years old, is hospitalized with complains of acute abdominal pain, sickness, vomiting, hemorrhagic rashes on skin. Hemorrhagic vasculitis is suspected. What therapy is necessary to prescribe this child? A. *NSAIDS and antiaggregants B. Spleenectomy C. Crioplasm D. Prednisolon and intravenous immunoglobulin (IVIG) E. Cryoplasm A previously healthy 3-year-old develops mucosal petechiae, multiple ecchymoses, and a platelet count of 20,000/mm3 2 weeks after a bout of chickenpox. What is the most likely diagnosis? A. von Willebrand disease B. Acute leukemia C. *Idiopathic (immune) thrombocytopenic purpura D. Aplastic anemia E. Thrombotic thrombocytopenic purpura In counseling a 15-year-old boy to avoid anabolic steroids, which are being used by some of his teammates, you indicate potential toxic effects to include which of the following? A. Hypoglycemia B. Increased testicular size C. Increased high-density lipoproteins D. *Toxic hepatitis E. Delayed closure of epiphyses The 4 years old boy is hospitalized with nasal bleeding, which had appeared in 1 hour after trauma. From anamnesis: he several time had hemarthrosis before 1 year. In the general blood analysis: RBC 3,1 millions/mm3, Hb 89 g/L, thrombocytes 165,000/mm3. Time of bleeding 4 minutes, time of clotting is 18 minutes. What is the most probable diagnose? A. Werlhof's disease B. Hemorrhagic vasculitis C. *Hemophilia D. Von Willebrand's disease E. DIC-syndrome After watching a recent afternoon television show about eating disorders, a mother 43. 44. 45. 46. 47. brings to your office her 15-year-old girl with the concern that “she may have one.” You try to determine whether this girl has anorexia nervosa or bulimia. Which of the following statements is correct? A. Rarely do anorexia and bulimia occur in the same patient simultaneously B. Anorexia nervosa most commonly occurs in girls less than 10 years old C. No signs of bulimia can be found, on careful physical examination D. *When used appropriately, imipramine is a useful adjunct in the treatment of bulimia E. Girls with anorexia nervosa are usually too weak to engage in active sports An otherwise healthy 7-year-old girl is brought to your office by her father because she has some acne, breast development, and fine pubic hair. The most likely etiology for her condition is: A. A feminizing ovarian tumor B. A gonadotropin-producing tumor C. A lesion of the central nervous system D. Exogenous estrogens E. *Early onset of “normal” puberty (constitutional) A 10-year-old obese boy has central fat distribution, arrested growth, hypertension, plethora, purple striae, and osteoporosis. Which of the following disorders is most likely to be responsible for the clinical picture that this boy presents? A. *Bilateral adrenal hyperplasia B. Adrenal adenoma C. Adrenal carcinoma D. Craniopharyngioma E. Ectopic adrenocorticotropin-producing tumor Appropriate initial management of the young man with Bilateral adrenal hyperplasia is: A. *Measurement of evening cortisol levels B. MRI of the adrenals C. Bilateral inferior petrosal blood sampling D. MRI of the brain and pituitary E. Adrenal scintigraphy with radiocholesterol The parents of a 14-year-old boy are concerned about his short stature and lack of sexual development. By history, you learn that his birth weight and length were 3 kg and 50 cm, respectively, and that he had a normal growth pattern, although he was always shorter than children his age. The physical examination is normal. His upper-to-lower segment ratio is 0.98. A small amount of fine axillary and pubic hair is present. There is no scrotal pigmentation; his testes measure 4.0 cm3 and his penis is 6 cm in length. In this situation you should: A. Measure pituitary gonadotropin B. Obtain a CT scan of the pituitary area C. Biopsy his testes D. Measure serum testosterone levels E. *Reassure the parents that the boy is normal The parents of a 14-year-old boy are concerned about his short stature and lack of sexual development. By history, you learn that his birth weight and length were 3 kg and 50 cm, respectively, and that he had a normal growth pattern, although he was always shorter than children his age. The physical examination is normal. His upper-to-lower segment ratio is 0.98. A small amount of fine axillary and pubic hair is present. There is no scrotal pigmentation; his testes measure 4.0 cm3 and his penis is 6 cm in length. Which of the following is the most likely diagnosis for this patient ? A. Hypopituitarism B. Klinefelter syndrome C. Hypothyroidism D. *Constitutionally short stature with delayed puberty 48. 49. 50. 51. 52. 53. 54. E. Male Turner syndrome A 14-year-old child who presents with delayed skeletal maturation (bone age) may have any of the following disorders EXEPT: A. Growth hormon deficiency B. Precocious puberty C. Hypothyroidism D. *Nonclassic (late-onset) 21-hydroxylase deficiency E. Constitutional delay of puberty All of the following are goals of newborn screening for congenital hypothyroidism EXEPT: A. To ensure normal linear growth B. To ensure normal intellectual function C. To facilitate genetic counseling D. *To prevent sudden infant death syndrome E. To prevent neurologic sequelae A child with pheochromocytoma may present with all of the following signs and symptoms EXEPT: A. Headache B. Weight loss C. Seizures D. Sweating E. *Flushing In the 1.5 months old boy there is often vomiting, liquid feces, hyperpigmentation of the scrotum. The skin is dry, grayish color. The blood potassium is 3.0 mmol/l. Adrenogenital syndrome is diagnosed. What treatment is pathogenetically correct in this case? A. Euphyllin, adrenalin, lasix B. 0,9% NaCl solution, hepatoprotectors C. *DOKSA, prednisolon, KCl solution D. Aminazin, metoclopramide E. Enterosgel, bufidum-bacterin The boy, 11 years old, complains of severe weakness, malaise, poor memory, significant weight loss, and hyperpigmentation of the skin. He is ill for 3 months. Objectively: astenic stature is noted brown color of tongue margins and lips mucous, hyperpigmentation of palms' folds, on neck, lumbar region. Cardiac rate is 110/minute, BP 70/35 mm Hg, heart tones are weak. In the blood: sugar - 3.2 mmol/l, potassium - 7.0 mmol/l, sodium - 110 mmol/l. What is the most reliable diagnosis? A. Adrenal gland tuberculosis B. Chronic heart failure C. Adrenal gland tumor D. *Chronic adrenal insufficiency E. Andrenogenital syndrome The girl, 3 years old, is hospitalized in infectious unit with meningococcal infection. Objectively: on skin hemorrhagic rashes; nose bleeding, abdominal pain are present. On the second day of the treatment her condition became worse: increased temperature - 39 С, child became adynamic, appeared loss of consciousness episodes. BP 65/40 mm Hg, pulse is weak, arrhythmic, 120 per minute, heart tones are dull. What is the reason of this complication? A. *Acute adrenal insufficiency B. Meningococcal meningitis C. Acute myocarditis D. DIC-syndrome E. Meningococcemia The 3.5 months old girl was hospitalized to the infectious department with complaints on 55. 56. 57. 58. 59. frequent liquid stool (approximately 12-14 times per day) with mucus admixtures, undigested meal remainders, periodic regurgitation. Objectively: was diagnosed hypotrophy 2 stage, nipples hyperpigmentation, clitoris hypertrophy. These symptoms had appeared in 3-weeks age. About what disease is possible to think? A. Salmonellosis B. Malabsorption syndrome C. *Adrenogenital syndrome D. Itsenko-Kushing syndrome E. Alactasia During examination of the 10 years old boy pediatrician has revealed paleness with jaundice, wrinkled skin, long lashes, excess of fat on upper half of the body, high trembling voice, and absence of permanent teeth. The height of the child is 106 cm (the average is 134 cm). The delay of the growth had begun after 2-year age. Put the diagnosis. A. *Dwarfism B. Hypothalamic syndrome C. Somatogenic nanism D. Adrenogenital syndrome E. False adiposogenital dystrophy In the 10 years old girl was diagnosed chronic adrenal insufficiency. What laboratory studies are necessary to perform to prove the diagnosis? A. General blood test, urinalyses B. Biochemical blood test (sugar, protein, bilirubin, AST, ALT) C. Blood test on cortisol, aldosteron, ACTH. Urinalysis: 17-OKS, 17-KS D. Acute inflammation reactants E. Blood test on somatothropine and ACTH content. Urinalysis: iodine excretion The boy, 8 years old, complains of spasmodic abdominal pain, vomiting, and increased temperature to 38 С. Objectively: skin is pale, "marble", with acrocyanosis. The heart tones are weak, pulse is weak, tachycardia, BP 70/30 mm Hg. Muscular tone is reduced, adynamia is present. In child was diagnosed acute adrenal insufficiency. What therapy is necessary to perform first of all? A. Antibiotics B. Antipyretics C. *Corticosteroids D. Cardiac glycosides E. Analgetics In the 12 years old girl was revealed pigmentation of the skin and mucous membranes – golden-brown color, muscular hypotonia, physical and sexual development retardation, hypodynamia. The preliminary diagnosis is: Addison’s disease. What hormones are necessary to give this child? A. Somatothropine, sexual hormones B. *Adrenal gland hormones, sexual hormones C. Thyroxin, sexual hormones D. Anabolic hormones, sexual hormones E. Parathormon, sexual hormones The boy, 8 years old, was hospitalized to the clinic with complaints on muscular weakness, languor, periodic stomachache. He is ill during 5 years. Objectively: is noted hyperpigmentation of the skin, delay in physical and sexual development, Cardiac rate is 106/ minute, BP 80/40 mm Hg. Heart tones are weak. In the blood: increased level of potassium, increased ACTH, decrease of sodium, chloride, cortisone. In urine decreased secretion of 17-OKS, 17-KS. What is the previous diagnosis? A. Acute adrenal insufficiency B. *Chronic adrenal insufficiency C. Adrenogenital syndrome Itsenko-Kushing syndrome Somatogenic nanism In the girl, 11 years old, is revealed enlarged thyroid gland, 2nd degree. The gland is enlarged unevenly, nodular formations are palpable. Regional lymphatic nodes are not enlarged. Chronic autoimmune thyroiditis is suspected. What method of investigation will prove the diagnosis? A. Investigation of thyroid hormones level B. Ultrasonic examination of the thyroid gland C. Thermography of the thyroid gland D. *Puncture biopsy of the thyroid gland E. Thyroidlymphographia The 7 years old child suffers from diabetes mellitus during 1 year. For the moment of examination he complains of thirst, frequent urination. Daily amount of urine is 3.5 liters. What is the reason of polyuria? A. Dehydration B. Decreased level of potassium in blood C. Increased level of phosphorus in blood D. Hypercalcemia E. *Hyperglycemia The 7-year-old child during 1 year has diabetes mellitus. He complains of thirst, frequent urination. Daily amount of urine is 3.5 litres. Indicate the reason of poliuria: A. Hypernatriemia B. Hypocaliemia C. Hyperphosphatemia D. Hypermagnesiemia E. *Hyperglycemia The boy, 7 years complains of hard inspiration with normal expiration, periodical vomiting. In anamnesis - often infectious diseases, collapses. Objectively: skin paleness, tonsillar and lymphatic nodes hyperplasia, thin hair, muscular tone decrease. In blood test: lymphocytosis, neuthropenia. On x-ray: enlarged thymus. Put the previous diagnosis. A. Thymus hypoplasia B. Thymoma C. *Thymomegaly D. Croup syndrome E. Foreign body aspiration The 10 years old boy has diabetes mellitus type 1. For the moment of examination he is unconscious. The skin is pale, wet and cold. Breathing is superficial. Muscular hypotonia, seizures had developed. It’s known that after injection of the insulin he had no meal. What is the most reliable diagnosis? A. Hyperglycemic coma B. *Hypoglycemic coma C. Hyperosmolar coma D. Infection E. Epilepsy The 10-year-old boy is unconscious. He has diabetes mellitus, is treated with insulin. After injection of the insulin he did not eat. In 2 hours had appeared dizziness, sleepiness and loss of the consciousness. The skin is pale, covered with "cool perspiration"; breathing is superficial. Muscular hypotonia and seizures had developed. What is the most reliable diagnosis? A. Hyperglycemic coma B. *Hypoglycemic coma C. Acute cardiac insufficiency D. Syncope D. E. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. 71. 72. E. Epilepsy The 12 years old girl is unconscious. She was hospitalized a 10 minutes before. During examination pediatrician has noted acetone smell in the air, dryness of the skin, redness of cheeks, reduced eyeballs tonus, Kussmaul’s breathing; heart tones are weakened, cardiac rate is 146/minute. The glucose level in the blood is 19.2 mmol/l, ketone bodies 500 mkmol/l. Which coma has developed in the child? A. Hypoosmolar B. Hyperosmolar C. *Ketoacidic D. Hyperlactacidemic E. Hypoglycemic The 10 years old boy was hospitalized because of blood glucose level 6.8 mmol/l. Other complaints are absent. Glucose tolerant test was reccomended to the boy. Indicate the dose of the glucose for this examination. A. 0.5 g/kg B. 1 g/kg C. 1.5 g/kg D. *1.75 g/kg E. 1.25 g/kg The 6-year-old boy was admitted to the hospital with complains of thirst, frequent urination, and weight loss. Blood glucose is 13,4 mmol/l. Glucosuria is 4%. It was diagnosed diabetes mellitus type 1. What insulin is indicated to this boy? A. Monotard B. Ultralente C. Semilente D. *Aktrapid E. Protofan The 11-years old girl has polyuria, polydipsia, dry skin, loss of weight. What is the most possible diagnosis? A. Addison’s disease B. Congenital hypothyroidism C. *Diabetes mellitus D. Grave’s disease E. Cushing syndrome The 6 years old boy is admitted to the hospital because of the diabetes mellitus. In the morning has appeared signs of influenza, at dinner he had poor appetite, through 1 hour after dinner he has lost the consciousness, the seizures had appeared. During examination: child is unconscious, the skin is pale, wet, and there is a lockjaw. Hypoglycemic coma is diagnosed. What urgent therapy does need this boy? A. Insulin intravenously B. *Glucose intravenously C. Heparin intravenously D. Sibasone intramuscular E. Cordiamin intravenously The 9 year-old girl is suffering from diabetes mellitus type 1 (DM) during 5 years. The disease is characterized with high hyperglycemia, tendency to ketosis and ketoacidosis, presence of chronic complications. Her daily insulin dose is 1 unit per kg. What is the severity of the DM according classification? A. Mild B. Moderate C. *Severe D. Moderately-severe E. Very severe In the 13 years old boy, who has diabetes mellitus type 1 for 6 years, was revealed 73. 74. 75. 76. 77. 78. delayed sexual development, small growth, hepatomegaly. What complication has developed in this boy? A. Cushing's syndrome B. *Mauriac's syndrome C. Laurence-Moon-Bardet-Biedl syndrome D. Waterhouse-Friderichsen syndrome E. Marfan's syndrome The 9-years old boy has daily diuresis 6,5 L of urine, specific gravity of urine 1.0041.008, and glucose in urine absent. What diagnosis is the most possible? A. Pyelonephritis B. Diabetes mellitus C. Glomerulonephritis D. *Diabetes insipidus E. Renal malformation The patient S., 11 years old, has DM type 1 during 5 years. He had no comas, but several times he was hospitalized because of ketoacidosis I-II stage. He has diabetic retinopathy I stage and hepatomegaly. He has daily insulin injections. What is the severity of the DM in this patient? A. Mild B. *Moderate C. Severe D. Extremely severe E. Not enough information for the severity estimation The patient M., 14 years old, has DM type 1 during 2 years. He had diabetic coma two months ago several times he was hospitalized because of ketoacidosis I-II stage. He has diabetic retinopathy III stage and diabetic nephropathy III stage. He has daily insulin injections. What is the severity of the DM in this patient? A. Mild B. Moderate C. *Severe D. Extremely severe E. Not enough information for the severity estimation The patient P., 4 years old, is suspecting to have DM during 3 months. She has hepatomegaly and she doesn’t use insulin for the treatment. What is the severity of the DM in this patient? A. Mild B. Moderate C. Severe D. Extremely severe E. *Not enough information for the severity estimation The patient B., 16 years old, has DM during 1 year. He had no ketoacidosis in anamnesis. He has no any complications of the DM. His treatment consists of diet, physical exercises and phytotherapy. What is the severity of the DM in this patient? A. *Mild B. Moderate C. Severe D. Extremely severe E. Not enough information for the severity estimation The patient V., 14 years old, has DM type 1 during 3 years. He had no comas, but several times he was hospitalized because of ketoacidosis I-II stage and one time because of hypoglycaemia. He has diabetic retinopathy I stage and diabetic arthropathy I st. He has daily insulin injections. What is the severity of the DM in this patient? A. Mild B. *Moderate Severe Extremely severe Not enough information for the severity estimation The patient B., 12 years old, has DM during 4 year. He has diabetic nephropathy III stage. He has daily insulin injections. What is the severity of the DM in this patient? A. Mild B. Moderate C. Severe D. Extremely severe E. *Not enough information for the severity estimation What are the clinical criteria of ideal glycemic control in DM? A. *Symptoms and complications are absent B. Symptoms are absent, but sometimes could be mild hypoglycemia in anamnesis C. Can be polyuria, polydipsia, poor weight gain. Can be episodes of severe hypoglycemia in anamnesis ut no comas D. Poor vision, painful seizures, growth and sexual development retardation, angiopathies, skin nfections, episodes of severe hypoglycemia and even comas in anamnesis E. Symptoms and complications are absent. There can be episodes of severe hypoglycemia in anamnesis but no comas. What are the clinical criteria of optimal glycemic control in DM? A. Symptoms and complications are absent B. *Symptoms are absent, but sometimes could be mild hypoglycemia in anamnesis C. Can be polyuria, polydipsia, poor weight gain. Can be episodes of severe hypoglycemia in anamnesis ut no comas D. Poor vision, painful seizures, growth and sexual development retardation, angiopathies, skin infections, episodes of severe hypoglycemia and even comas in anamnesis E. Symptoms and complications are absent. There can be episodes of severe hypoglycemia in anamnesis but no comas. What are the clinical criteria of suboptimal glycemic control in DM? A. Symptoms and complications are absent B. Symptoms are absent, but sometimes could be mild hypoglycemia in anamnesis C. *Can be polyuria, polydipsia, poor weight gain. Can be episodes of severe hypoglycemia in anamnesis ut no comas. D. Poor vision, painful seizures, growth and sexual development retardation, angiopathies, skin infections, episodes of severe hypoglycemia and even comas in anamnesis E. Symptoms and complications are absent. There can be episodes of severe hypoglycemia in anamnesis ut no comas. What are the clinical criteria of high risk for the life glycemic control in DM? A. Symptoms and complications are absent B. Symptoms are absent, but sometimes could be mild hypoglycemia in anamnesis C. Can be polyuria, polydipsia, poor weight gain. Can be episodes of severe hypoglycemia in anamnesis but no comas. D. *Poor vision, painful seizures, growth and sexual development retardation, angiopathies, skin infections, episodes of severe hypoglycemia and even comas in anamnesis E. Symptoms and complications are absent. There can be episodes of severe hypoglycemia in anamnesis ut no comas. Choose the correct statement: A. To make the diagnosis of DM is always necessary to perform OGTT B. A random blood glucose level greater than 11,1 mmol/l, is sufficient to make the diagnosis of DM C. D. E. 79. 80. 81. 82. 83. 84. C. 85. 86. 87. 88. 89. 90. 91. *A random blood glucose level greater than 11,1 mmol/ which is verified on a repeat test, is sufficient to make the diagnosis of DM D. A random blood glucose level greater than 6,1 mmol/l, is sufficient to make the diagnosis of DM E. A random blood glucose level greater than 11,1 mmol/l, which is verified on a repeat test, is ufficient to make the diagnosis of DM Choose the correct staement: A. To make the diagnosis of DM is always necessary to perform OGTT B. A random blood glucose level greater than 11,1 mmol/l, is sufficient to make the diagnosis of DM C. A random blood glucose level greater than 6,1 mmol/ which is verified on a repeat test, is sufficient o make the diagnosis of DM D. A fasting blood gluose level greater than 6,1 mmol/l, is sufficient to make the diagnosis of DM E. *A fasting blood glucose level greater than 6,1 mmol/l, which is verified on a repeat test, is sufficient to make the diagnosis of DM To the 7 years old boy who had fasting (whole blood) glucose level 6,0 mmol/L was performed GTT. In two hours his glucose level was 12,0 mmol/L. What is his diagnose? A. Impaired Glucose Tolerance (IGT) B. Impaired Fasting Glycaemia (IFG) C. *Diabetes mellitus D. Diabetes insipidus E. He is healthy To the 12 years old boy who had fasting (whole blood) glucose level 5,9 mmol/L was performed GTT. In two hours his glucose level was 7,1 mmol/L. What is his diagnose? A. Impaired Glucose Tolerance (IGT) B. *Impaired Fasting Glycaemia (IFG) C. Diabetes mellitus D. Diabetes insipidus E. He is healthy To the 13 years old girl who had fasting (whole blood) glucose level 6,0 mmol/L was performed GTT. In two hours his glucose level was 9,1 mmol/L. What is his diagnose? A. *Impaired Glucose Tolerance (IGT) B. Impaired Fasting Glycaemia (IFG) C. Diabetes mellitus D. Diabetes insipidus E. He is healthy To the 12 years old boy who had fasting (whole blood) glucose level 5,4 mmol/L was performed GTT. In two hours his glucose level was 5,2 mmol/L. What is his diagnose? A. Impaired Glucose Tolerance (IGT) B. Impaired Fasting Glycaemia (IFG) C. Diabetes mellitus D. Diabetes insipidus E. *He is healthy To the 10 years old girl who had fasting (whole blood) glucose level 5,9 mmol/L was performed GTT. In two hours his glucose level was 7,3 mmol/L. What is his diagnose? A. Impaired Glucose Tolerance (IGT) B. *Impaired Fasting Glycaemia (IFG) C. Diabetes mellitus D. Diabetes insipidus E. He is healthy To the 16 years old boy who had fasting (whole blood) glucose level 6,2 mmol/L was performed OGTT. In two hours his glucose level was 14,0 mmol/L. What is his diagnose? Impaired Glucose Tolerance (IGT) Impaired Fasting Glycaemia (IFG) *Diabetes mellitus Diabetes insipidus He is healthy To the 17 years old girl who had fasting (whole blood) glucose level 5,9 mmol/L was performed OGTT. In two hours his glucose level was 10,0 mmol/L. What is his diagnose? A. *Impaired Glucose Tolerance (IGT) B. Impaired Fasting Glycaemia (IFG) C. Diabetes mellitus D. Diabetes insipidus E. He is healthy In the 10-years old girl are developed signs of Raynaud's syndrome, vomiting and abdominal pain after prolonged overcooling. Objectively: skin and sclera yellowish, liver and spleen enlarged. Examination results: positive direct and indirect Coombs' test, moderate anemia, increased indirect bilirubin level. What diagnosis is the most possible? A. Minkovsky-Chauffard disease B. Thalassemia C. *Acquired autoimmune hemolytic anemia D. Sickle cell anemia E. Hepatitis B The boy is 7 years old. He is hospitalized with petechial rashes on limbs; the rush elements are different in size and in color. Thrombocytopenic purpura is suspected. What in blood analysis will confirm the diagnosis? A. Leucocytosis B. Increased ESR C. *Prolonged time of the bleeding D. Prolonged time of coagulation E. Reduction of thrombocytes adhesive activity The 9 years old girl suffering from ITP during 2 years, she has often relapses. She received glucocorticoids before. In the general blood analysis: RBC 3,0 millions in mm3, Hb 88 g/l, thrombocytes 49,000-68,000 /mm3. What should be the next treatment step? A. Glucocorticoids in high doses B. Transplantation of the bone marrow C. *Intravenous immune globulin (IVIG) D. Spleenectomy E. Cytostatics The 10 years old boy complains of periodic nasal bleedings, bruises on legs, hips, forearms. Objectively: skin is pale, on limbs - hemorrhagic rashes of different size and color. Other organs and systems are normal. The liver margin is on the level of right costal arch, spleen is not enlarged. What is the most probable diagnosis? A. Von Willebrand's disease B. Hemophilia C. * ITP D. Schoenlein-Henoch purpura E. DIC-syndrome The girl, 10 years old, has addressed to physician with complains of numerous hemorrhagic rashes on limbs, trunk, which appeared without any reason. Two weeks ago she has recovered from viral infection. Thrombocytopenic purpura is suspected. What therapy is necessary to prescribe this child? A. Heparin B. Acetylsalicylic acid A. B. C. D. E. 92. 93. 94. 95. 96. 97. C. D. E. 98. 99. 100. 101. 102. 103. *Prednisolon Crioplasm Azathioprin The 5 years old boy is hospitalized in clinic because of long (during 2 days) bleeding after tooth extraction. In anamnesis he has nasal bleedings, bruises on abdomen, and back often. His mother has metrorrhagias sometimes. In the general blood analysis: RBC 2,8 millions/mm3, Hb 86g/L, thrombocytes 196000/mm3, time of bleeding is 12 minutes, time of coagulation is 5 minutes. What is the most probable diagnose? A. Shoenlein-Genoch's disease B. Hemophilia C. Thrombocytopenic purpura D. *Von Willebrand's disease E. DIC-syndrome The girl, 7 years old, is hospitalized with complains of acute abdominal pain, sickness, vomiting, hemorrhagic rashes on skin. Hemorrhagic vasculitis is suspected. What therapy is necessary to prescribe this child? A. *NSAIDS and antiaggregants B. Spleenectomy C. Crioplasm D. Prednisolon and intravenous immunoglobulin (IVIG) E. Cryoplasm The 4 years old boy is hospitalized with nasal bleeding, which had appeared in 1 hour after trauma. From anamnesis: he several time had hemarthrosis before 1 year. In the general blood analysis: RBC 3,1 millions/mm3, Hb 89 g/L, thrombocytes 165,000/mm3. Time of bleeding 4 minutes, time of clotting is 18 minutes. What is the most probable diagnose? A. Werlhof's disease B. Hemophilia C. *Hemorrhagic vasculitis D. Von Willebrand's disease E. DIC-syndrome The 3.5 months old girl was hospitalized to the infectious department with complaints on frequent liquid stool (approximately 12-14 times per day) with mucus admixtures, undigested meal remainders, periodic regurgitation. Objectively: was diagnosed hypotrophy 2 stage, nipples hyperpigmentation, clitoris hypertrophy. These symptoms had appeared in 3-weeks age. About what disease is possible to think? A. Salmonellosis B. Malabsorption syndrome C. *Adrenogenital syndrome D. Itsenko-Kushing syndrome E. Alactasia The boy, 7 years complains of hard inspiration with normal expiration, periodical vomiting. In anamnesis - often infectious diseases, collapses. Objectively: skin paleness, tonsillar and lymphatic nodes hyperplasia, thin hair, muscular tone decrease. In blood test: lymphocytosis, neuthropenia. On x-ray: enlarged thymus. Put the previous diagnosis. A. Thymus hypoplasia B. Thymoma C. *Thymomegaly D. Croup syndrome E. Foreign body aspiration An 8 year old child has low-grade fever, arthritis, colicky abdominal pain and a purpuric rash localized on the lower extremities. laboratory studies reveal a guaiac-positive stool, urinalysis with red blood cell (RBC) casts and mild proteinuria, and a normal platelet 104. 105. 106. 107. 108. 109. count. The most likely diagnosis is: A. * Henoch-Schonlein's vasculitis B. Systemic lupus erythematosus (SLE) C. Rocky Mountain spotted fever D. Idiopathic thrombocytopenic purpura E. Poststreptococcal glomerulonephritis A young man has painful indurations in the peripapillary regions of both mammary glands. The most reasonable action will be: A. * To leave these indurations untouched B. To remove them C. To cut and drain them D. To take an aspirate for bacterial inoculation and cytology E. To administer steroids locally Patient with thyreotoxicosis is in the 2 beds hospital ward of pediatrics department. The area of the ward is 18 m2, height 3 m, ventilation rate 2,5/hr. Air temperature – 20 degrees per calcium, relative humidity – 45 %, air movement velocity - 0,3 m/s, light coefficient - 1/5, noise level - 30 dB. Do hygienic evaluation of the conditions meet the standards? A. * Not comfortable microclimate B. Non-effective ventilation C. Poor lighting D. High level of noise E. All conditions meet the requirements A 7 y.o. boy has crampy abdominal pain and a rash on the back of his legs and buttocks as well as on the extensor surfaces of his forearms. Laboratory analysis reveals proteinuria and microhematuria. He is most likely to be affected by: A. * Anaphylactoid purpura B. Systemic lupus erythematosus C. Poststreptococcal glomerulonephritis D. Polyarteritis nodosa E. Dermatomyositis A 3-year-old child has been admitted to a hospital because of ostealgia and body A. Sternal puncture B. Ultrasound C. Lymph node puncture D. Lymph node biopsy E. Computer tomography A 2-months-old child after preventive vaccination had a prolonged hemorrhage from the vaccination place and due to those an intramuscular hematoma. During examination of the child a considerable rise of prothrombin consumption and a significant prolongation of the activated partial thromboplastic time were found. What is the most probable diagnosis? A. * Hemophilia B. Werlhof's disease C. Henoch-Schoenlein disease D. Hemorrhagic disease of the neonate E. Inborn afibrinogenemia A 14-year-old girl has been presenting with irritability and tearfulness for about a year. A year ago she was also found to have diffuse enlargement of the thyroid gland (II grade). This condition was regarded as a pubertal manifestation, the girl didn't undergo any treatment. The girl's irritability gradually gave place to a complete apathy. The girl got puffy face, soft tissues with edemas, bradycardia, constipations. Skin pallor and gland density progressed, the skin became of a waxen hue. What disease may be suspected? A. B. C. D. E. 110. 111. 112. 113. * Autoimmune thyroiditis Diffuse toxic goiter Thyroid carcinoma Subacute thyroiditis Juvenile basophilism A 2 m.o. child with birth weight 5100 g has jaundice, hoarse cry, umbilical hernia, physical development retardation. Liver is +2 cm enlarged, spleen is not enlarged. In anamnesis: delayed falling-away of umbilical cord rest. In blood: Hb- 120 g/L, erythrocytes - 4,5, ESR- 3 mm/h. Whole serum bilirubin is 28 mkmol/L, indirect - 20 mkmol/L, direct - 8 mkmol/L. What is the most probable diagnosis? A. * Congenital hypothyreosis B. Congenital hepatitis C. Hemolitic anemia D. Conjugated jaundice E. Cytomegalovirus infection Examination of a 12 year old child revealed diffuse thyroid enlargement of the II degree. Heart auscultation revealed dullness of heart sounds, heart rate was 64/min. The child has frequent constipations, anemia. Concentration of thyreoglobulin antibodies is increased. What disease might have caused such symptoms? A. * Autoimmune thyroiditis B. Diffuse toxic goiter C. Thyroid carcinoma D. Thyroid hyperplasia E. Endemic goiter A 13 y.o. teenager who suffers from hemophilia A was hospitalized after a fight at school. His diagnosis is right-sided hemarthros of knee joint, retroperitoneal hematoma. What should be primarily prescribed? A. * Fresh frozen plasma B. Aminocapronic acid C. Washed thrombocytes D. Placental albumin E. Dry plasma On the second day after preventive vaccination a 2-year-old boy presented with abdominal pain without clear localization, body temperature 38. On the third day the child got red papular haemorrhagic eruption on the extensor surfaces of limbs and around the joints. Knee joints were edematic and slightly painful. Examination of other organs and systems revealed no pathological changes. What is the most likely diagnosis? A. * Haemorrhagic vasculitis B. Thrombocytopenic purpura C. Meningococcemia D. Urticaria E. DIC syndrome