CFM Protocol: Neonatal Brain Monitoring & Hypothermia
advertisement
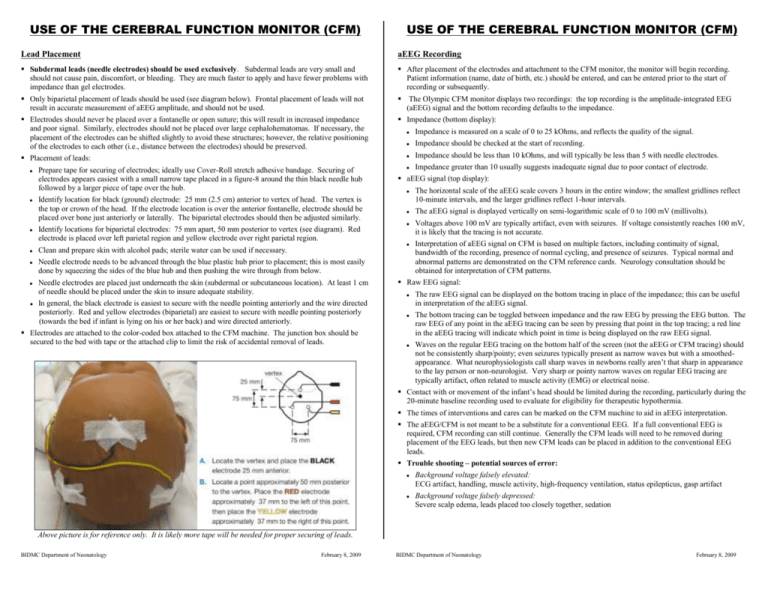
USE OF THE CEREBRAL FUNCTION MONITOR (CFM) USE OF THE CEREBRAL FUNCTION MONITOR (CFM) Lead Placement aEEG Recording Subdermal leads (needle electrodes) should be used exclusively. Subdermal leads are very small and should not cause pain, discomfort, or bleeding. They are much faster to apply and have fewer problems with impedance than gel electrodes. After placement of the electrodes and attachment to the CFM monitor, the monitor will begin recording. Patient information (name, date of birth, etc.) should be entered, and can be entered prior to the start of recording or subsequently. Only biparietal placement of leads should be used (see diagram below). Frontal placement of leads will not result in accurate measurement of aEEG amplitude, and should not be used. The Olympic CFM monitor displays two recordings: the top recording is the amplitude-integrated EEG (aEEG) signal and the bottom recording defaults to the impedance. Electrodes should never be placed over a fontanelle or open suture; this will result in increased impedance and poor signal. Similarly, electrodes should not be placed over large cephalohematomas. If necessary, the placement of the electrodes can be shifted slightly to avoid these structures; however, the relative positioning of the electrodes to each other (i.e., distance between the electrodes) should be preserved. Impedance (bottom display): Placement of leads: Prepare tape for securing of electrodes; ideally use Cover-Roll stretch adhesive bandage. Securing of electrodes appears easiest with a small narrow tape placed in a figure-8 around the thin black needle hub followed by a larger piece of tape over the hub. Identify location for black (ground) electrode: 25 mm (2.5 cm) anterior to vertex of head. The vertex is the top or crown of the head. If the electrode location is over the anterior fontanelle, electrode should be placed over bone just anteriorly or laterally. The biparietal electrodes should then be adjusted similarly. Identify locations for biparietal electrodes: 75 mm apart, 50 mm posterior to vertex (see diagram). Red electrode is placed over left parietal region and yellow electrode over right parietal region. Clean and prepare skin with alcohol pads; sterile water can be used if necessary. Needle electrode needs to be advanced through the blue plastic hub prior to placement; this is most easily done by squeezing the sides of the blue hub and then pushing the wire through from below. Needle electrodes are placed just underneath the skin (subdermal or subcutaneous location). At least 1 cm of needle should be placed under the skin to insure adequate stability. In general, the black electrode is easiest to secure with the needle pointing anteriorly and the wire directed posteriorly. Red and yellow electrodes (biparietal) are easiest to secure with needle pointing posteriorly (towards the bed if infant is lying on his or her back) and wire directed anteriorly. Electrodes are attached to the color-coded box attached to the CFM machine. The junction box should be secured to the bed with tape or the attached clip to limit the risk of accidental removal of leads. Impedance is measured on a scale of 0 to 25 kOhms, and reflects the quality of the signal. Impedance should be checked at the start of recording. Impedance should be less than 10 kOhms, and will typically be less than 5 with needle electrodes. Impedance greater than 10 usually suggests inadequate signal due to poor contact of electrode. aEEG signal (top display): The horizontal scale of the aEEG scale covers 3 hours in the entire window; the smallest gridlines reflect 10-minute intervals, and the larger gridlines reflect 1-hour intervals. The aEEG signal is displayed vertically on semi-logarithmic scale of 0 to 100 mV (millivolts). Voltages above 100 mV are typically artifact, even with seizures. If voltage consistently reaches 100 mV, it is likely that the tracing is not accurate. Interpretation of aEEG signal on CFM is based on multiple factors, including continuity of signal, bandwidth of the recording, presence of normal cycling, and presence of seizures. Typical normal and abnormal patterns are demonstrated on the CFM reference cards. Neurology consultation should be obtained for interpretation of CFM patterns. Raw EEG signal: The raw EEG signal can be displayed on the bottom tracing in place of the impedance; this can be useful in interpretation of the aEEG signal. The bottom tracing can be toggled between impedance and the raw EEG by pressing the EEG button. The raw EEG of any point in the aEEG tracing can be seen by pressing that point in the top tracing; a red line in the aEEG tracing will indicate which point in time is being displayed on the raw EEG signal. Waves on the regular EEG tracing on the bottom half of the screen (not the aEEG or CFM tracing) should not be consistently sharp/pointy; even seizures typically present as narrow waves but with a smoothedappearance. What neurophysiologists call sharp waves in newborns really aren’t that sharp in appearance to the lay person or non-neurologist. Very sharp or pointy narrow waves on regular EEG tracing are typically artifact, often related to muscle activity (EMG) or electrical noise. Contact with or movement of the infant’s head should be limited during the recording, particularly during the 20-minute baseline recording used to evaluate for eligibility for therapeutic hypothermia. The times of interventions and cares can be marked on the CFM machine to aid in aEEG interpretation. The aEEG/CFM is not meant to be a substitute for a conventional EEG. If a full conventional EEG is required, CFM recording can still continue. Generally the CFM leads will need to be removed during placement of the EEG leads, but then new CFM leads can be placed in addition to the conventional EEG leads. Trouble shooting – potential sources of error: Background voltage falsely elevated: ECG artifact, handling, muscle activity, high-frequency ventilation, status epilepticus, gasp artifact Background voltage falsely depressed: Severe scalp edema, leads placed too closely together, sedation Above picture is for reference only. It is likely more tape will be needed for proper securing of leads. BIDMC Department of Neonatology February 8, 2009 BIDMC Department of Neonatology February 8, 2009 CFM Trace Examples Therapeutic Hypothermia The following examples are taken from “Olympic CFM 6000 Clinical Guide”, Olympic Medical / Natus. Normal trace (continuous with cycling) The following are taken from the Therapeutic Hypothermia Protocol from Children’s Hospital Boston. Inclusion Criteria: Gestational age 36 weeks and birth weight 2000 gm Evidence of sleep/wake cycling Upper margin > 10 Volts and lower margin > 5 Volts Limited variability (narrow band) Evidence of fetal distress as evidenced by at least one of the following: History of acute perinatal event (e.g. placental abruption, cord prolapse, severe fetal heart rate abnormality, variable or late decelerations) Biophysical profile < 6/10 (or < 4/8) within 6 hours of birth Cord pH ≤ 7.0 or base deficit ≥ 16 mEq/L Evidence of neonatal distress as evidenced by at least one of the following: Note dark central band of continuous activity. Moderately abnormal trace (discontinuous pattern) Apgar score ≤ 5 at 10 minutes Postnatal blood gas at 1 hour ≤ 7.0 or base deficit ≥ 16 mEq/L Continued need for ventilation initiated at birth and continued for at least 10 minutes Evidence of neonatal encephalopathy by physical exam (by neurologist) No evidence of sleep/wake cycling Upper margin > 10 Volts and lower margin < 5 Volts Increased variability (broad band) Discontinuous pattern, can be seen in moderate/severe encephalopathy or after drugs like anticonvulsants and sedatives. No dark central band is seen. Note the universal gray color. Abnormal cerebral function monitor (CFM), with minimum of 20 minutes recording, with one of the following: Severely abnormal: upper margin < 10 Volts Moderately abnormal: upper margin > 10 Volts and lower margin < 5 Volts Seizures identified by aEEG Exclusion Criteria: Normal initial CFM tracing: lower margin > 5 Volts and no seizures (only on initial CFM recording) Inability to initiate cooling by 6 hours of age Severely abnormal trace (inactive, flat) Presence of lethal chromosomal anomaly (e.g. Trisomy 13 or 18) No evidence of sleep/wake cycling Upper margin < 10 Volts Presence of severe congenital anomalies (e.g. complex cyanotic congenital heart disease, major central nervous system anomaly) Symptomatic systemic congenital viral infection (e.g. hepatosplenomegaly, microcephaly) Greatly reduced variability Symptomatic systemic bacterial infection (e.g. meningo-encephalitis, DIC) Bleeding diathesis (platelet count < 50K, spontaneous clinical bleeding) Major intracranial hemorrhage General suppression of amplitude – trace is narrow, low voltage. May be accompanied by brief bursts of voltage (burst-suppression). Can be accompanied by seizure activity. Seizures Seizure onset shows continuous high activity Causes CFM to narrow and rise up Seizures show a decrease in variability as level of electrocortical activity rises, represented by sudden narrowing and rise in band. Infants with a normal interictal band of activity can have a mild hypoxicischemic insult or seizure may be due to a cerebral infarction or biochemical abnormality. BIDMC Department of Neonatology February 8, 2009 BIDMC Department of Neonatology February 8, 2009