Reducing Surgical Site Infection at the VA
advertisement
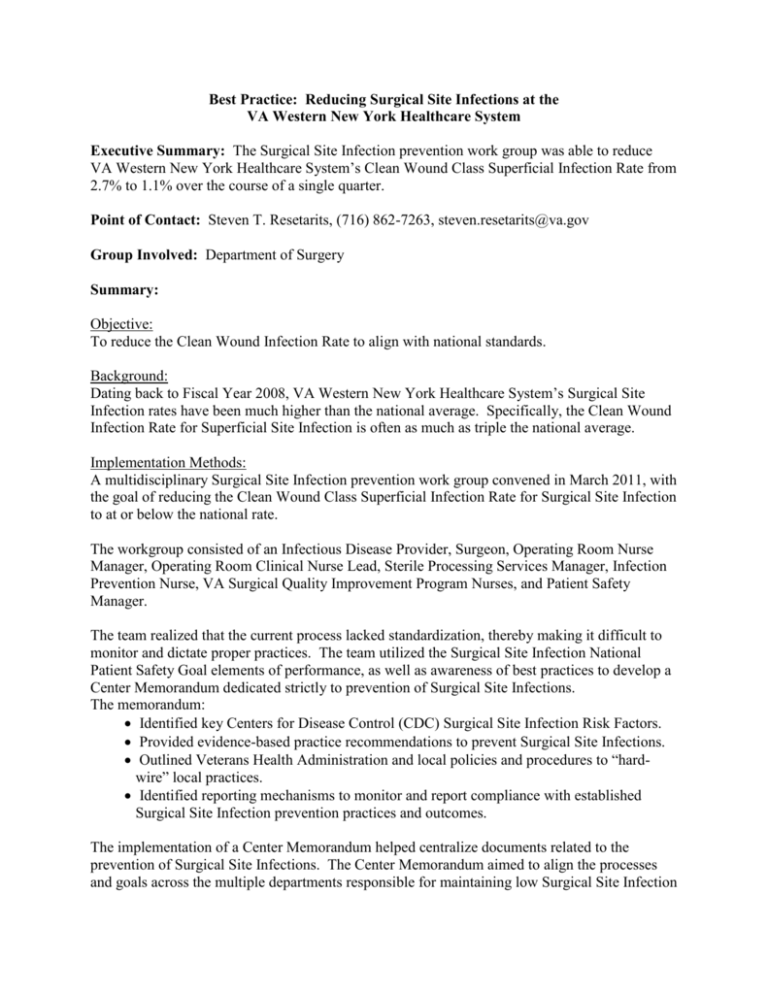
Best Practice: Reducing Surgical Site Infections at the VA Western New York Healthcare System Executive Summary: The Surgical Site Infection prevention work group was able to reduce VA Western New York Healthcare System’s Clean Wound Class Superficial Infection Rate from 2.7% to 1.1% over the course of a single quarter. Point of Contact: Steven T. Resetarits, (716) 862-7263, steven.resetarits@va.gov Group Involved: Department of Surgery Summary: Objective: To reduce the Clean Wound Infection Rate to align with national standards. Background: Dating back to Fiscal Year 2008, VA Western New York Healthcare System’s Surgical Site Infection rates have been much higher than the national average. Specifically, the Clean Wound Infection Rate for Superficial Site Infection is often as much as triple the national average. Implementation Methods: A multidisciplinary Surgical Site Infection prevention work group convened in March 2011, with the goal of reducing the Clean Wound Class Superficial Infection Rate for Surgical Site Infection to at or below the national rate. The workgroup consisted of an Infectious Disease Provider, Surgeon, Operating Room Nurse Manager, Operating Room Clinical Nurse Lead, Sterile Processing Services Manager, Infection Prevention Nurse, VA Surgical Quality Improvement Program Nurses, and Patient Safety Manager. The team realized that the current process lacked standardization, thereby making it difficult to monitor and dictate proper practices. The team utilized the Surgical Site Infection National Patient Safety Goal elements of performance, as well as awareness of best practices to develop a Center Memorandum dedicated strictly to prevention of Surgical Site Infections. The memorandum: Identified key Centers for Disease Control (CDC) Surgical Site Infection Risk Factors. Provided evidence-based practice recommendations to prevent Surgical Site Infections. Outlined Veterans Health Administration and local policies and procedures to “hardwire” local practices. Identified reporting mechanisms to monitor and report compliance with established Surgical Site Infection prevention practices and outcomes. The implementation of a Center Memorandum helped centralize documents related to the prevention of Surgical Site Infections. The Center Memorandum aimed to align the processes and goals across the multiple departments responsible for maintaining low Surgical Site Infection Steven Resetarits Graduate Management Portfolio rates. The ultimate goal was to provide better patient care through process improvement. This would occur through monitoring and reporting compliance , as well as staff education, competency and annual improvement plans. Implementation occurred in several ways: Staff was educated on formal processes of patient preparation. A two-step patient preparation process was utilized, with the patient prepped initially in the Ambulatory Surgery Unit, with preparation finalized prior to operation. Team worked with staff to remove as much variation as possible, with the hopes of streamlining new processes. Team members would conduct observations as well as chart reviews to ensure proper patient handling and preparation. After VAWNYHS implemented the Center Memorandum, the team became responsible for both ensuring policy compliance and monitoring data to determine the effectiveness of the of the Surgical Site Infection prevention measures. Results: Shortly after the implementation of the Center Memorandum, as well as staff education regarding new processes and responsibilities, VAWNYHS identified a Clean Wound Class Superficial Infection Rate of 1.1%, which decreased from 2.7% the previous quarter. The following three quarters each noted a 0.5% Clean Wound Class Superficial Infection Rate, which is significantly below the national average of roughly 1.0%. The implementation of the Center Memorandum created a culture of compliance that became hard-wired into everyday practice. Conclusion: I joined this project in its infancy, and had the privilege of watching the improvements as they occurred. This project is outcomes-based: the results are clearly measurable, and progress is verifiable. Each quarter, the team took great pleasure in reviewing the results, and after several quarters, the team was able to say the project was a resounding success. As the implementation process is not specific to our facility, the local methods are replicable across all healthcare systems. As several quarters have passed without a regression to former practices and results, the process is sustainable. The improvement team has permanently changed the status quo within our surgery department. The project is also innovative. It required an overhaul of current practices, changed provider’s techniques, and modified standard practices. New process Implemented