Mycobacterium tuberculosis
advertisement
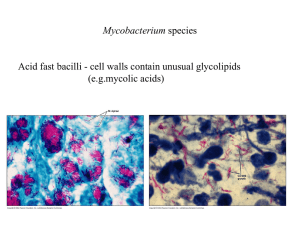
MYCOBACTERIA Dr. Sudheer Kher KEYWORDS Acid Fast Ziehl-Neelsen Stain Mycolic acids Tuberculosis (Koch’s disease) M. tuberculosis M. bovis M. leprae Tubercle Lowenstein Jensen medium PPD Tuberculin BCG Polymerase chain reaction Runyon groups Classification of Mycobacteria 1. Tubercle bacilli a) b) c) d) e) 2. Lepra bacilli a) b) 3. Human – MTB Bovine – M. bovis Murine – M. microti Avian – M. avium Cold blooded – M. marinum Human – M. leprae Rat – M. leprae murium Mycobacteria causing skin ulcers a) b) M. ulcerans M. belnei 4. Atypical Mycobacteria (Runyon Groups) a) b) c) d) 5. Photochromogens Scotochromogens Nonphotochromogens Rapid growers Johne’s bacillus M. paratuberculosis 6. Saprophytic mycobacteria a) b) c) d) e) M. butyricum M. phlei M. stercoralis M. smegmatis Others Tuberculosis (TB, Consumption, Koch’s Disease) • M. tuberculosis • major human disease – healthy people • problems – association with AIDS – multiple drug-resistance –Chronic disease –Prolonged treatment General characters of the genus Slender rods Resist staining but once stained, resist decolorization by dilute mineral acids; hence called ACID FAST BACILLI (AFB) Aerobic, Non-motile, Non-sporing, Noncapsulated. Growth generally slow Genus includes – Obligate parasites – Opportunist pathogens – Saprophytes Mycobacterium tuberculosis One of the most serious infectious diseases in the developing world One third of world’s population infected with M. tuberculosis Thirty million people have active disease Nine million new cases occur Three million people die of the disease, each year. Mycobacterium tuberculosis (MTB) Morphology – – Ziehl – Neelsen stain – Once stained by Carbol fuchsin, resist decolorization by 20% Sulphuric acide and absolute alcohol. Acid & Alcohol Fast (AFB) – Fluorescent dyes like Auramine O or Rhodamine also stain and the decolorization is resisted. – Reason for Acid & Alcohol fastness – Presence of unsaponifiable wax Mycolic acid Semi permeable membrane around the cell Property of cell wall and related to integrity of the cell wall – Staining may be uniform or granular MTB : Cultural characters Grow slowly. Generation time 14-15 hrs Colonies appear after 2 weeks or at 6-8 weeks MTB - Obligate aerobe MTB grows more luxuriantly (eugonic) than M. bovis (dysgonic). Addition of 0.5% Glycerol supports growth of human strains. No effect or inhibitory effect on bovine strains. MTB : Culture media Solid media – – Egg containing Lowenstein-Jensen Medium Petragnini medium Dorset – Blood containing – Tarshi’s – Serum containing – Loeffler’s serum slope – Potato containing – Pawlowsky’s Liquid media – – – – – – Dubos’ Middlebrooks Proskauer & Beck’s Sula’s Sauton’s Resistance Not specifically resistant to heat. 60 C x 20 min destroys. In sputum can survive 20-30 hrs Relatively resistant to disinfectants. Survives exposure to – – – – – 5 % Phenol 15 % Sulphuric acid 3 % Nitric acid 5 % Oxalic acid 4 % NaOH Biochemical reactions Niacin test – Human MTB produces niacin when grown in egg medium. Aryl Sulphatase test – Enzyme Aryl sulphatase formed by only atypical mycobacteria. Biochemical reactions Neutral red test – Virulent strains of tubercle bacilli bind neutral red in alkaline solution while avirulent strains can not. Catalase–paroxidase test – Most atypical mycobacteria are strongly catalase positive while MTB is only weakly positive. MTB is strongly peroxidase positive while atypical mycobacteria are negative. Nitrate reduction test – Positive in MTB and negative in M. bovis Mycobacterium tuberculosis (MTB) Morphology – – Straight or slightly curved rods Modes of infection 1- Droplet infection Person to person by inhalation aerosols Mycobacterium tuberculosis (Pulmonary tuberculosis) 2- Ingestion of milk Infected cattle Mycobacterium bovis (Intestinal tuberculosis) 3- Contamination of abrasion Laboratory workers (Skin infection) Pathogenesis of tuberculosis • infects lung • distributed within macrophages • facultative intracellular pathogen – inhibits phagosome-lysosome fusion – resists lysosomal enzymes Other minor pathogenesis factors tuberculosis • mycobactin – siderophore • cord factor – damages mitochondria Cell-mediated immunity tuberculosis • infiltration – macrophages – lymphocytes granulomas • tubercles • Classical tubercular lesion – Granuloma with typical Langhan’s giant cells, epithelioid cells, lymphocytes and fibrosis. There are multiple light areas (opacities) of varying size that run together (coalesce). Arrows indicate the location of cavities within these light areas. The appearance is typical for chronic pulmonary tuberculosis. Tuberculosis Clinical picture : * * * * * Low grade fever Weight loss Night sweats Fatigue Cough & haemoptysis Laboratory diagnosis M. tuberculosis Acid fast bacteria in sputum Culture on L J media Biochemical identification Antibiotic sensitivity test Tuberculin test PCR Lowenstein Jensen Medium – Selective. Always in screw capped bottle. Bluish Green. Contains – Egg protein – Solidifying agent Mineral salts – Mg sulphate, Mg citrate Asparagine Malachite Green – Selective agent Sterilized by - Inspissation Laboratory diagnosis - tuberculosis • skin testing – delayed hypersensitivity – tuberculin – protein purified derivative, PPD • X-ray Tuberculin Test (Mantoux test) Delayed hypersensitivity skin test to assay: cell mediated immunity to tubercle bacillius Material: A purified protein derivative (PPD) Dose : 0.1 ml of (PPD) is injected intradermal Reading : Positive test is defined as - Induration equal or greater than 10 mm - Develop 48-72 hours after injection Positive skin test tuberculosis indicates exposure to organism • does not indicate active disease • Tuberculin Test Interpretation: * A positive test indicates previous exposure and carriage of T.B. * A negative tuberculin test excludes infection in suspected persons * Tuberculin positive persons may develop reactivation type of T.B. * Tuberculin negative persons are at risk of gaining new infection * False positive reactions are mainly due to: - Infection with nontuberculous mycobacteria * False negative reactions may be due to: - Sever tuberculosis infection (Miliary T.B.) - Hodgkin’s disease - Corticosteroid therapy - Malnutrition - AIDS * Children below 5 years of age with no exposure history: - Positive test must be regarded suspicious Laboratory Diagnosis Demonstration of bacilli Culture & isolation or Animal inoculation Demonstration of hypersensitivity to tubercular protein Serological tests limited value Specimen * According to site of infection : - Sputum - Urine - Gastric lavage - Blood - Body fluids - Tissue biobsy * Specimens need appropriate processing Sputum Liquefaction with N-acetyl-L- cysteine Decontamination with NaOH Centrifugation Laboratory Diagnosis Pulmonary TB – – Specimen – Sputum – Early morning, if scanty 24 hrs, three consecutive day samples. Laryngeal swabs or gastric lavage in children. – Microscopy –See at least 100 field / 10 minutes. Grading – – 1+ -> 3-9 bacilli in entire smear – 2+ -> 10 or more in entire smear – 3+ -> 10 or more bacilli seen in most oil immersion fields – Culture & AST – Animal inoculation – Animal of choice Guinea Pig. Laboratory Diagnosis Extra -Pulmonary TB – – Specimen – CSF – in suspected meningitis Pleural fluid & other exudates 2-3 days urine in renal TB Biopsy material. Concentration methods Purpose – Homogenization & Concentration in sputum & other specimens. Methods – Concentration methods Useful for microscopy, culture & animal inoculation – Petroff’s method Most widely used Equal volumes of Sputum + 4% NaOH incubated at 37C X 20 min.Centrifuge at 3000 rpm X 30 min. Sediment neutralized by N/10 HCl. Can be used for smear, culture, animal inoculation – Simpler method To avoid centrifugation & Neutralization Equal volumes of sputum + solution of Cetrimoniom bromide 20 g + NaOH 40 g in one litre. Allow to stand for five minutes. Inoculate Acid Buffered LJ Medium with swab. Laboratory diagnosis M. tuberculosis (culture) • grows very slowly – several weeks – non-pigmented colonies – niacin production *differentiates from other mycobacteria Tuberculosis • polymerase chain amplification –rapid diagnosis Pathogenesis * Inhalation of tubercle bacilli * They multiply in the alveolar macrophages * An early tubercle (granuloma) is formed Pathogenesis * Lesions, healing or progression of infection depend upon 1- Dose of infecting mycobacteria 2- Resistance and hypersensitivity of host * Virulence : Glycolipids on the outer surface of bacteria - Enhance granuloma formation - Inhibit migration of polymorphnuclear leucocytes - Help survival of tubercle bacilli inside macrophages Pathogenesis A- Primary infection: * An exudative lesion : - spread to regional lymph nodes - A scar of healing may later calcify (Ghon’ focus) - Lymph nodes caseate and then calcify - Bacilli in the lesion slowly die - Tuberculin test becomes positive - The person immune & hypersensitive Pathogenesis B- Reactivation type : * Activation of tubercle bacilli due to immunity * Formation of tubercles that caseate - fibrosis - open into a bronchus (open tuberculosis) * Tubercle bacilli erode a blood vessels - Infect any organ (Miliary T.B.) Treatment Chemoprophylaxis – INH for one year Domicilliary treatment preferred Drugs – – – – – – – – – – Rifampicin Isoniazide Pyrazinamide Streptomycin Ethambutol Ethionamide Thiacetazone Paraminosalicylic acid Cycloserine Bactericidal Bacteriostatic Treatment Short term chemotherapy of six months is sufficient Problem area – Development of resistance by mutant selection – Solution – Treatment by two to three drug combination, adequate treatment. Treatment Use multiple drug therapy to prevent emergence of resistant mutants * Long duration treatment (6-18 months) * Four drugs are usually started in initial therapy due to: - Intracellular location of bacilli - Slow growth rate of bacilli - Caseous material blocks penetration of drugs - Some bacilli persist in a metabolically inactive state * Sputum becomes non-infective 2-3 weeks after starting therapy Treatment Drugs used : 1- First line drugs : - Isoniazid - Rifampicin - Pyrazinamide - Ethambutol - Streptomycin 2- Second line drugs (more toxic and less effective): - Kanamycin - capreomycin - Cycloserin - ethionamide - ciprofloxacin - Ofloxacin * Noncompliance (failure to complete the course): Directly observed therapy (DOT) Health care workers observe the medication Immuno-prophylaxis Intradermal injection of live attenuated vaccine Bacille Calmette-Guerin (BCG). The strain causes self limited lesion and induces hypersensitivity & immunity. Coverts tuberculin negative person to positive reactor. Immunity lasts for 10-15 years. Immunity 60-80% BCG Given at birth without tuberculin testing Protects against TB, the disease runs milder course in protected, prevents skeletal, meningeal & miliary forms. Also found useful in leprosy, leukaemias and other malignancies by non-specific stimulation of RE system.