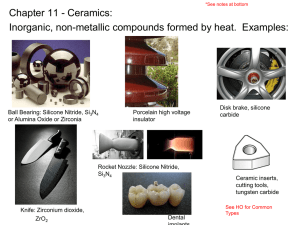
Ceramics
advertisement

CLASSIFICATION OF BIOMATERIALS Drug Delivery Devices Skin/cartilage Polymers Bone replacements Orthopedic screws/fixation Metals Dental Implants Ocular implants Synthetic BIOMATERIALS Ceramics Dental Implants Implantable Microelectrodes Semiconductor Materials Biosensors METALIC BIOMATERIALS Crystal structures and strong metallic bonds orthopedic applications material joint prosthesis and bone renewal - the face and jaw surgery Dental implant - cardio-vascular surgery Artificial heart parts, heart valve Metals used as Biomaterials Steel Cobalt-containing alloys Titanium and titanium containing alloys Dental amalgam (XHg) Gold Nickel- titanium alloys Corrosion; The undesired chemical reaction of metals with their surruondings that forms oxygen, hydroxide and other compounds then degradation Corroding Metal X Biocompatible Ceramic Biomaterials (Bioceramics) The class of ceramics used for repair and replacement of diseased and damaged parts of the musculoskeletal system are referred to as bioceramics. OBJECTIVES To examine chemical/physical properties of ceramics To introduce the use of ceramics as biomaterials To explore concepts and mechanisms of bioactivity 5 Ceramics (keramikos- pottery in Greek) Ceramics are refractory polycrystalline compounds Usually inorganic Highly inert Hard and brittle High compressive strength Generally good electric and thermal insulators Good aesthetic appearance Applications: orthopaedic implants dental applications compromise of non-load bearing for bioactivity 6 BIOCERAMICS Bioceramics; Repair the parts of body that injured or lost their function, restructuring or special ceramics are designed to replace ; - polycrystalline structure ceramic (alumina), - bioactive glass, - bioactive glass-ceramics, - bioactive composites… Using Areas of Bioceramics Glasses, Diagnostic devices, Thermometers, Tissue culture vessels. Filling materials, Gold-porcelain coating, Prosthetic parts Health Sector Dental Structure Ceramic Structure: AmXn ZnS A: metal, +ve CsCl NaCl X: nonmetal, -ve 9 Nature’s Ceramic Composites Natural hard tissues are “ceramic”- polymer composites: » Bones, Teeth, Shells Tissue = organic polymer fibers + mineral + living cells Mineral component (Ceramic) » Bone: hydroxyapatite (HA) – Ca5(PO4)3OH Mineralization under biological conditions: » Many elemental substitutions » Protein directed crystallization » Unique characteristics – crystal morphology and solubility Synthetic calcium phosphates are used as biomaterials – “bioactive” Synthetic HA Bone HA 10 Types of Ceramics nearly bioinert 11 Bioactivity vs. Biocompatibility Biocompatibility : Objective is to minimize inflammatory responses and toxic effects Bioactivity - Evolving concept: The characteristic that allows the material to form a bond with living tissue (Hench, 1971) The ability of a material to stimulate healing and trick the tissue system into responding as if it were a natural tissue (Hench 2002). Advantages: Bone tissue – implant interface, enhanced healing response, extends implant life Biodegradability: Breakdown of implant due to chemical or cellular actions If timed to rate of tissue healing transforms implant to scaffold for tissue regeneration Negates issues of stress shielding, implant loosening, long term stability 12 Classification based on tissue attachment 13 Mechanical Properties B. Amsden CHEE 340 14 BIOCERAMICS BIOINERT BIOACTIVE Bioactive ceramic, that allows the chemical bond formation between tissue and implant Bioinert ceramic, that doesn’t allow the chemical bond formation between tissue and implant MATERIAL TISSUE TOXIC DEAD Bioinert Various thicknesses of fibrous tissue NON-TOXIC Bioactive binding of tissueimplant interface, Soluble Tissue replaces İmplant place Classification of Bioceramics According to Tissue Responses Implant Type Tissue response Example Nonporous, dense and inert ceramics The formation of very fine fibrous tissue Alumina, Zirconia Porous inert ceramics The tissue growth in Hydroxyapatite pores Resorbable ceramics Absorption Tricalcium phosphate Bioactive glasses Ceramic implants are non-toxic Bioceramics According to Structural Functions Oxide ceramics, inert structure, polycrystalline ceramics consisting of metal ions in the plane formed by the dissolution of oxygen ions Alumina (Al2O3) orthopedic applications Zirconia (ZrO2) femoral prosthese Inert Ceramics: Alumina History: since early seventies more than 2.5 million femoral heads implanted worldwide. alumina-on-alumina implants have been FDA monitored over 3000 implants have been successfully implemented since 1987 Smaller the grain size and porosity, higher the strength E = 380 GPa (stress shielding may be a problem) High hardness: Low friction Low wear Corrosion resistance Friction: surface finish of <0.02 um Wear: no wear particles generated – biocompatible 19 Inert Ceramics: Aluminum Oxides (Alumina – Al2O3) Applications orthopaedics: »femoral head »bone screws and plates »porous coatings for femoral stems »porous spacers (specifically in revision surgery) »knee prosthesis dental: crowns and bridges 20 Alumina Bioinertness Results in biocompatibility – low immune response Disadvantage: » Minimal bone ingrowth » Non-adherent fibrous membrane » Interfacial failure and loss of implant can occur 21 Inert Ceramics: Zirconia, ZrO2 zirconium; named from the Arabic, zargun = gold color Fabrication: • Obtained from the mineral zircon • Addition of MgO, CaO, CeO, or Y2O3 stabilize tetragonal crystal structure (e.g. 97 mol%ZrO2 and 3 mol%Y2O3) • Usually hot-pressed or hot isostatically pressed Applications: • orthopaedics: femoral head, artificial knee, bone screws and plates, favored over UHMWPE due to superior wear resistance • dental: crowns and bridges 22 Glass and glass-ceramics: Silica(SiO2) –based ceramics (Includes LithiumAluminum or Magnesium-Aluminum crystals ) Bioglass: Instead of some silica groups, calcium, phosphorus or sodium is present (SiO2, Na2O, CaO, P2O5) Bioactive Ceramics: Glass Ceramics Glass: an inorganic melt cooled to solid form without crystallization an amorphous solid Possesses short range atomic order Brittle! Glass-ceramic is a polycrystalline solid prepared by controlled crystallization of glass Glass ceramics were the first biomaterials to display bioactivity (bone system): • Capable of direct chemical bonding with the host tissue • Stimulatory effects on bone-building cells 24 Bioactive Ceramics: Glass Ceramics Composition includes SiO2, CaO and Na2O Bioactivity depends on the relative amounts of SiO2, CaO and Na2O Cannot be used for load bearing applications Ideal as bone cement filler and coating due to its biological activity 25 Bioactive Ceramics: Glass ceramics SiO2 B C A D CaO A: Bonding within 30 days Na2O B: Nonbonding, reactivity too low C: Nonbonding, reactivity too high D: Bonding 26 Bioactive Ceramics: Glass Ceramics Bioactive: capable of direct chemical bonding with the host biological tissue Glass: • an inorganic melt cooled to solid form without crystallization • an amorphous solid • possesses short range atomic order BRITTLE! Glass-ceramic is a polycrystalline solid prepared by controlled crystallization of glass LESS BRITTLE 27 Calcium-phosphate ceramics ; their structure is the form of multiple oxides of calcium and phosphate atoms Hydroxyapatite Ca5(PO4)3OH, Tricalcium phosphate, Ca3(PO4)2 Oktacalcium phosphate CaH(PO4)3.2OH In medicine and dentistry Biodegradable Ceramics: Calcium (Ortho) Phosphate Structure resembles bone mineral; thus used for bone replacement Coating of metal implants to promote bone ingrowth Different forms exist depending on Ca/P ratio, presence of water, impurities and temperature 7 different forms of PO4 based calcium phosphates exist - depend on Ca/P ratio, presence of water, pH, impurities and temperature 29 Calcium Phosphate • Powders • Scaffolds • Coatings for implants – metals, heart valves to inhibit clotting • Self-Setting bone cement 30 Calcium Phosphates Uses repair material for bone damaged trauma or disease void filling after resection of bone tumors repair and fusion of vertebrae repair of herniated disks repair of maxillofacial and dental defects ocular implants drug-delivery coatings for metal implants, heart valves to inhibit clotting 31 Advantage of Bioceramics The resistance to Microorganisms, Temparature, Solvents pH changes High pressures is the advantage in health and dental aplications Bioceramics are used repair or renewal of a hard connective tissue in the skeleton The elderly, the bones are very brittle slow-moving cracks, uncertainties to durability in different strokes and pressures The most important reasons for limiting the use of bioceramics, Interaction of bioceramics with tissues All materials placed on live tissue ,takes response from tissue TISSUE - IMPLANT Why Use Bioceramics? General Options Toxic/ Imunogenic/ Disease transmission? Mechanical Properties? Bioactive? Degradable? Autograft Allograft Metals Ceramics Excellent Moderate Low Polymers Composites Advantages to Bioceramics: Disadvantage of Bioceramics: • Biological compatibility and activity • Brittleness – not for load bearing applications •Less stress shielding •No disease transmission •Unlimited material supply 35