chapter37_Sections 4
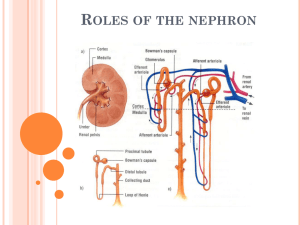
advertisement
Cecie Starr Christine Evers Lisa Starr www.cengage.com/biology/starr Chapter 37 The Internal Environment (Sections 37.4 - 37.7) Albia Dugger • Miami Dade College 37.4 Urine Formation • Urine consists of water and solutes filtered from blood and not returned to it, along with solutes secreted from blood into the nephron’s tubular regions • Urine is formed by three processes: • Glomerular filtration • Tubular reabsorption • Tubular secretion Glomerular Filtration • Blood pressure drives glomerular filtration • 20% of blood fluid entering a glomerulus is forced out through gaps in capillary walls into Bowman’s capsule • Plasma proteins, blood cells, and platelets remain in blood • Protein-free plasma in Bowman’s capsule becomes filtrate that enters the proximal tubule • glomerular filtration • Protein-free plasma forced out of glomerular capillaries by blood pressure enters Bowman’s capsule Glomerular Filtration Glomerular Filtration glomerulus inside Bowman’s capsule outer wall of Bowman’s capsule efferent arteriole (to peritubular capillaries) afferent arteriole (from renal artery) filtrate (to proximal tubule) Fig. 37.9, p. 620 Tubular Reabsorption • Tubular reabsorption returns water, glucose, amino acids, most Na+, Cl–, K+, and bicarbonate ions to the blood • In the proximal tubule, transport proteins move ions and other nutrients into peritubular capillaries • Water follows solutes by osmosis • tubular reabsorption • Substances move from the filtrate inside a kidney tubule into the peritubular capillaries Tubular Secretion • Tubular secretion moves H+, K+ and breakdown products of foreign organic molecules (drugs, food additives, pesticides) from blood in peritubular capillaries into the filtrate • Membrane proteins in peritubular capillaries actively transport substances into interstitial fluid • Substances cross tubule epithelium and enter the filtrate • tubular secretion • Substances move out of peritubular capillaries and into the filtrate in kidney tubules Concentrating the Urine • Active transport of ions at the ascending loop of Henle, and urea pumped out of the collecting tubule, contribute to high solute concentration in interstitial fluid of the renal medulla • High solute concentration draws water out of filtrate in the descending loop of Henle, and again as urine descends through the collecting tubule • The body adjusts how much water is reabsorbed at distal tubules and collecting tubules Hormonal Effects on Urine Formation • Hormones alter permeability of distal and collecting tubules to adjust urine concentration • A rise in Na+ concentration causes the hypothalamus to tell the pituitary gland to secrete antidiuretic hormone • When blood pressure declines, cells in nephron arterioles release renin, which (through a series of reactions) results in secretion of aldosterone by adrenal glands Key Terms • antidiuretic hormone (ADH) • Pituitary hormone that encourages water reabsorption • Makes distal tubules and collecting tubules more permeable to water • aldosterone • Adrenal hormone that makes distal tubules and collecting tubules more permeable to Na+ • Encourages sodium reabsorption • Leads to more water reabsorption Hormonal Effects on Urine (cont.) • Atrial natriuretic peptide (ANP) makes urine more dilute by inhibiting aldosterone secretion • Muscle cells in the heart’s atria release ANP when high blood volume causes atrial walls to stretch • Parathyroid hormone (PTH) affects urine composition • When blood calcium level declines, PTH acts on the kidney to increase reabsorption of calcium Urine Formation Urine Formation proximal tubule collecting tubule distal tubule protein-free plasma Glomerular 2 Tubular 3 Tubular 1 filtration reabsorption secretion Bowman’s capsule Na+, Cl–, K+, nutrients, H2O Na+, Cl–, H2O H+, K+ H+ 4 peritubular capillary renal cortex renal medulla descending arm of loop of Henle increasing solute concentration in interstitial fluid 1 Glomerular filtration Proteinfree plasma forced out of glomerular capillaries by blood pressure enters Bowman’s capsule. Na+ H2O 2 Tubular reabsorption Essential ions, nutrients, water, and some urea in the filtrate return to the blood. Green arrows indicate reabsorption. H2O 3 Tubular secretion Wastes and excess ions are moved from the blood into the filtrate for elimination in urine. Blue arrows indicate secretion. ascending arm of loop of Henle Na+ urea H2O 4 Hormones that alter permeability of distal and collecting tubules adjust urine concentration. Aldosterone increases Na+ reabsorption, and water follows by osmosis. Antidiuretic hormone directly increases water reabsorption. urine to renal pelvis Fig. 37.10, p. 621 Urine Formation collecting tubule proximal tubule distal tubule protein-free plasma 2 Tubular 1 Glomerular reabsorption Bowman’s filtration capsule Na+, Cl–, K+, nutrients, H2O 3 Tubular secretion Na+, Cl–, H2O H+, K+ H+ 4 renal cortex renal medulla peritubular capillary descending arm of loop of Henle increasing solute concentration in interstitial fluid Na+ H2O H2O ascending arm of loop of Henle Na+ urea H2O urine to renal pelvis Stepped Art Fig. 37.10, p. 621 ANIMATION: Urine formation To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE Key Concepts • What Kidneys Do • Urine begins forming when protein-free plasma filters across capillary walls into kidney tubules • Reabsorption returns most water, solutes, and nutrients to the blood • Unabsorbed filtrate and secreted substances become the urine • Hormones adjust urine concentration ANIMATION: Formation of urine To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE ANIMATION: Tubular reabsorption To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE Animation: Reabsorption and Secretion 37.5 Kidney Disease • Kidney function is measured in terms of the filtration rate through glomerular capillaries • Kidney failure occurs when the filtration rate falls by half • Failure of both kidneys can be fatal: Wastes build up in blood and interstitial fluid, pH rises, and changes in ion concentrations (Na+, K+) interfere with metabolism Causes of Kidney Failure • Most kidney problems arise as complications of diabetes mellitus or high blood pressure, which damage capillaries that interact with nephrons • Kidneys also fail after filtering toxins (lead, arsenic, pesticides), high doses of drugs (aspirin), or other dangerous substances from the blood • High-protein diets force kidneys to work harder, and increase the risk for kidney stones Treating Kidney Failure • Kidney dialysis can restore proper solute balances in a person with kidney failure • With hemodialysis, a patient’s blood is pumped through semipermeable tubes submerged in a solution that draws out wastes, and cleansed blood is returned to the patient’s body • With peritoneal dialysis, dialysis solution is pumped into a patient’s abdominal cavity at night, and drained in the morning Two Types of Kidney Dialysis filter where blood flows through semipermeable tubes and exchanges substances with dialysis solution Two Types of Kidney Dialysis abdominal cavity, lined with peritoneum (green) patient’s blood inside tubing A Hemodialysis Tubes carry blood from a patient’s body through a filter with dialysis solution that contains the proper concentrations of salts. Wastes diffuse from the blood into the solution and cleansed, solute-balanced blood returns to the body. dialysis solution flowing into abdominal cavity dialysis solution with unwanted wastes and solutes draining out B Peritoneal dialysis Dialysis solution is pumped into a patient’s abdominal cavity. Wastes diffuse across the lining of the cavity into the solution, which is then drained out. Fig. 37.11, p. 622 filter where blood flows through semipermeable tubes and exchanges substances with dialysis solution Two Types of Kidney Dialysis abdominal cavity, lined with peritoneum (green) patient’s blood inside tubing A Hemodialysis Tubes carry blood from a patient’s body through a filter with dialysis solution that contains the proper concentrations of salts. Wastes diffuse from the blood into the solution and cleansed, solute-balanced blood returns to the body. dialysis solution flowing into abdominal cavity dialysis solution with unwanted wastes and solutes draining out B Peritoneal dialysis Dialysis solution is pumped into a patient’s abdominal cavity. Wastes diffuse across the lining of the cavity into the solution, which is then drained out. Stepped Art Fig. 37.11, p. 622 ANIMATION: Kidney dialysis To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE 37.6 Heat Gains and Losses • Maintaining the temperature of the internal environment within a tolerable range is another major aspect of homeostasis • The heat content of any complex animal depends on a balance between gains (from metabolism and the environment) and losses (to the environment): Heat change = heat produced + heat gained - heat lost Changes to Core Temperature • Heat is gained or lost at body surfaces by processes of radiation, conduction, convection, and evaporation • Thermal radiation is emission of heat into space around a warm object • Conduction transfers heat between objects in direct contact with each other • In convection, moving air or water transfers heat • In evaporation, converting water on a body surface from liquid to gas cools the body Endotherm? Ectotherm? Heterotherm? • Fishes, amphibians, and nonbird reptiles are ectotherms, which are “heated from outside” by the environment • Most birds and mammals are endotherms, which are “heated from within” by metabolism • Some birds and mammals are heterotherms, which maintain a constant core temperature some of the time but allow their temperature to shift at other times Key Terms • ectotherm • Animal that controls its internal temperature by altering its behavior; for example, a fish or a lizard • endotherm • Animal that controls its internal temperature by adjusting its metabolism; for example, a bird or a mammal • heterotherm • Animal that maintains its temperature by production of metabolic heat sometimes, and allows its temperature to fluctuate with the environment at other times Ectotherm and Endotherm Key Concepts • Adjusting the Core Temperature • Heat losses to the environment and heat gains from the environment and from metabolic activity determine an animal’s body temperature • Ectotherms adjust their temperature behaviorally • Endotherms can adjust production of metabolic heat 37.7 Temperature Regulation in Mammals • The hypothalamus maintains body temperature through negative feedback response • The hypothalamus receives input from thermoreceptors • When the temperature deviates, the hypothalamus calls for responses that return temperature to the set point Responses to Heat Stress • When a mammal is too hot, the hypothalamus issues commands for peripheral vasodilation (increases radiation) • Sweat increases evaporative heat loss across skin; mammals that don’t sweat may drool, lick fur, or pant to speed cooling • Dangerous overheating (hyperthermia) occurs when the body gets too hot – above 41.5°C (105°F) Evaporative Cooling • Sweat only cools if it evaporates from skin • On humid days, evaporation rate slows, so sweating is less effective at cooling ANIMATION: Control of human body temperature To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE Responses to Cold Stress • The hypothalamus can cause arterioles in skin to contract, reducing radiation; fluffing up hair or fur reduces convection; and shivering produces metabolic heat • shivering response • In response to cold, rhythmic muscle contractions generate metabolic heat Responses to Cold Stress (cont.) • Exposure to cold increases secretion of thyroid hormone, which binds to metabolically active fat (brown adipose tissue) and encourages nonshivering heat production • brown adipose tissue • Adipose tissue that responds to cold by releasing energy as heat, rather than using it to make ATP • nonshivering heat production • Heat-generating mechanism of brown adipose tissue; energy is released as heat, rather than stored in ATP Hypothermia • Hypothermia occurs when a drop in core body temperature disrupts normal function • In humans, body temperature of 95°F (35°C) impairs brain activity • Severe hypothermia causes loss of consciousness, disrupts heart rhythm, and can be fatal Impact of Cold Stress Titanic: Death by Hypothermia Heat and Cold Stress Compared Key Concepts • Regulation • Mammals react to heat stress by moving blood to the skin and increasing evaporation by sweating or panting • They react to cold stress by moving blood to their core, fluffing up fur or hair, and increasing metabolic heat production Truth in a Test Tube (revisited) • Water-soluble drugs and toxins are generally not reabsorbed from filtrate in kidney tubules, and end up in the urine • How fast kidneys remove substances from blood varies with age and health • A healthy 35-year-old eliminates drugs twice as fast as a healthy 85-year-old ANIMATION: Feedback control of temperature To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE ANIMATION: Human thermoregulation To play movie you must be in Slide Show Mode PC Users: Please wait for content to load, then click to play Mac Users: CLICK HERE