Renal System
advertisement

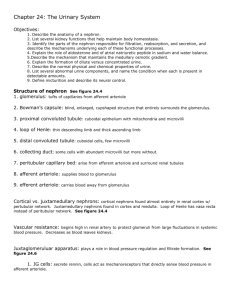
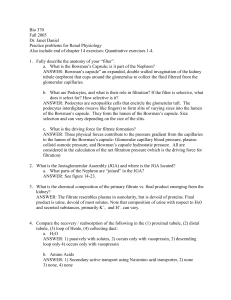
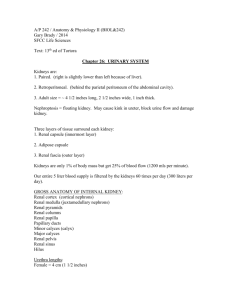
Excretory System Tony Serino, Ph.D. Assistant Professor of Biology Misericordia Univ. Excretory System • Remove wastes from internal environment • Wastes: water, heat, salts, urea, etc. • Excretory organs include: Lungs, Skin, Liver, GI tract, and Kidneys • Urinary system account for bulk of excretion Fluid Input & Output Urinary System Ureter Histolgy -about 25 cm long, retroperitoneal, moves urine by peristalsis; volume of urine moved is called a jet (1-5 jets/min) -ureters enter the bladder wall obliquely, allowing them to remain closed except during peristalsis Adventitia Mucosa Muscularis Urinary Bladder (Remanent of Allantois) Urinary Bladder Histology Mucosa Submucosa Muscularis (Detrusor Muscle) (Serosa) Urinary Bladder Filling • Highly distensible • 10-600ml normally • Capable of 2-3X that volume • Under normal conditions, the pressure does not significantly increase until at least 300 ml volume is reached Urethra Urethra Histology -epithelium changes from transitional to stratified squamous along its length -large numbers of mucous glands present Bladder (Storage) Reflex Voluntary control • As urine accumulates, the bladder wall thins and rugae disappear • Innervation (sympathetic) to the sphincter muscles (particularly the internal sphincter) keeps the bladder closed and depresses bladder contraction Micturition Reflex (Voiding) • Urine volume increases, and the smooth muscle increases pressure in bladder • Stretch receptors in detrusor muscle, increase parasympathetic activity in the splanchnic nerve cause increase bladder contraction and internal sphincter relaxation • Voluntary relaxation of external sphincter by a decrease in firing of the pudendal nerve Kidney Location (x.s.) (Retroperitoneal) Human Kidney Hilus Cortex vs. Medulla Capsule Anatomy of Kidney Major and Minor Calyx Arterial Supply Venous Drainage Renal Circulation Renal Cortex Blood Flow Glomerulus BP in Renal Vessels Nephron (two types) Epithelium of Nephron Urine Formation Overveiw a. b. c. d. d Pressure Filtration Reabsorption Secretion Reabsorption of water Glomerulus (SEM) Glomerulus Bowman’s Capsule Podocytes Filtration in Glomerulus Capillary Lumen Endothelium Basement Mem. Pedicels Slit pores Glomerular Filtrate Fenestration Glomerular Filtration • A pressure filtration produced by the BP, fenestrated capillaries of glomerulus, and the podocytes creates the glomerular filtrate • Slit size allows filtration of any substance smaller than a protein • Blood proteins create an osmotic gradient to prevent complete loss of water in blood, • Pressure in Bowman’s capsule also works against filtration • Volume of filtrate produced per minute is the Glomerular Filtration Rate (GFR) • Average GFR = 120-125 ml/min Forces controlling Glomerular Filtration PCT and DCT (H&E stain) Tubular Reabsorption • 75-85% of glomerular filtrate reabsorbed in PCT • Some of the reabsorption is by passive diffusion – Example: Na+ • Much of the reabsorption is active, most linked to the transport of Na+; known as co-transport • The amount of transporter proteins is limited; so most actively transported substances have a maximum tubular transport rate (Tm) Reabsorption Loop of Henle and CD • Provides mechanism where water can be conserved; capable of producing a low volume, concentrated urine • Loop of Henle acts as a counter-current multiplier to maintain a high salt concentration in medulla • CD has variable water permeability and must pass through the medulla • Allows for the passive absorption of water Counter-current Multiplier • Descending is permeable to water but not salt; loss of water concentrates urine in tube • Ascending is permeable to NaCl but not water; Salt now higher in tube than interstitium; first passively diffuses out then near top is actively transported out • Results in a self-perpetuating mechanism; maintaining a high salt concentration in center of kidney Vasa Recta • Supply long loops of Henle • Provide mechanism to prevent accumulation of water in interstitial space • Passive diffusion allows the blood to equilibrate with osmotic gradient in extracellular space Counter-current Exchange Tubular Secretion • PCT and DCT both actively involved in secretion (active transport of substances from the blood to the urine) • Both ducts play important roles in controlling amount of H+/HCO3- lost in urine and therefore blood pH • DCT actively controls Na+ reabsorption upon stimulation by aldosterone (controls final 2% of Na+ in urine) Summary Re-absorption Water Re-absorption with ADH present Loses water Loses NaCl Selective Secretion & Re-absorption Dehydration & Water Intoxication Thirst ADH release Reabsorption of Water in CD Hypertonic, low volume urine Juxtaglomerular Apparatus Renin-Angiotensin-Aldosterone iBP Decreased Stretch in JG cells Decreased Na in Urine in DCT h Renin Release h stimulation of Macula Densa Angiotensinogen g Angiotensin I h arteriolar constriction Converting Enzyme h BP Angiotensin II h Aldosterone Release h Na+ reabsorption h water retention and BV Declining BP Regulation Stimulates thirst Increase BP Regulation (ANP) Acid/Base Transport