PROSES PEMBENTUKAN URIN

PROSES
PEMBENTUKAN URIN
Rahmatina B. Herman
Bagian Fisiologi
Fakultas Kedokteran Universitas Andalas
Functions of Urinary System
The urinary system performs a variety of functions aimed at maintaining homeostasis
In concert with hormonal and neural inputs, the kidneys primarily responsible for maintaining the stability of ECF volume, electrolyte composition, and osmolarity (solute concentration)
Excreting (eliminating) the end products (wastes) of bodily metabolism, such as urea, uric acid, creatinine; since these wastes are toxic , especially to brain
Main route for eliminating potentially toxic metabolic wastes and foreign compounds from the body
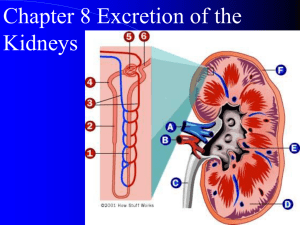
Urine Formation
The urinary system forms the urine and carries it to the outside that consists of:
- The kidneys as the urine forming organs
- The structures that carry urine from kidneys to the outside for eliminating from the body
Three basic processes in urine formation:
1. Filtration by glomerolus
2. Reabsorption by tubules
3. Secretion by tubules
Filtration By Glomerolus
Glomerular capillaries: impermiabel to protein
Glomerular filtrates:
- protein-free
- concentration of materials that do not bind with protein as same as in plasma
Filtration rate of glomerular capillary >> other capillaries, because of greater in:
- hydrostatic pressure
- glomerular filtration coefficient (K f
) product of permeability and effective filtration surface area of glomerular capillary
Afferent arteriole Efferent arteriole
Capillary pore
Layers of glomerular membrane:
1 the pores between endothelium cells of glomerular capillary
2 an acellular basement membrane
3 filtration slits between foot processes of podocytes of inner layer of Bowman capsule
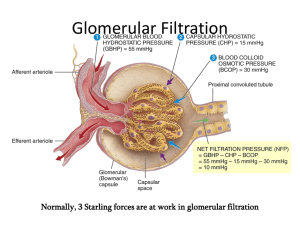
…..Filtration By Glomerolus
The factors governing filtration across glomerular capillaries (GC) are the same as all other capillaries
For each nephron:
- Glomerular filtration coefficient (K f
)
- Mean hydrostatic pressure in GC (P
GC
)
- Mean hydrostatic pressure in Bowman’s capsule (P
T
)
- Colloid osmotic pressure of plasma in GC (π
GC
)
- Colloid osmotic pressure of filtrate (π
T
) → protein free
Net Filtration Pressure
P
GC
π
GC
Glomerular capillary
P
T
Bowman’s capsule
P
GC
π
GC
P
T
: Mean hydrostatic pressure in GC
: Colloid osmotic pressure of plasma in GC
: 60 mmHg
: 32 mmHg
: Mean hydrostatic pressure in Bowman’s capsule : 18 mmHg
Net filtration pressure: 60-32-18= 10 mmHg
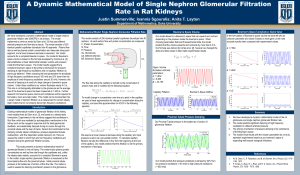
Glomerular Filtration Rate (GFR)
Is actual rate of filtration by glomerular capillaries
Depends on:
- Net filtration pressure
- Filtration coefficient (K f
)
GFR = (K f
) x Net filtration pressure
In males: 125 mL/min (7.5 L/h or 180 L/d) in females: 115 mL/min (6.9 L/h or 160 L/d)
Factors Affecting GFR
Changes in renal blood flow
Changes in glomerular capillary hydrostatic pressure
- Changes in systemic blood pressure
- Afferent or efferent arteriolar constriction
Changes in hydrostatic pressure in Bowman’s capsule
- Ureteral obstruction
- Edema of kidney inside tight renal capsule
Changes in concentration of plasma proteins
- Dehydration , hypoproteinemia, etc (minor factors)
Changes in K f
- Changes in glomerular capillary permeability
- Changes in effective filtration surface area
…..Filtration
Filtration fraction:
- Fraction of plasma flowing through glomeruli that is filtered into tubules
- Ratio of GFR to renal plasma flow (RPF)
GFR
RPF
- Normal: ± 0,20 it means: 20 % of plasma that enters glomeruli is filtered by glomerular capillaries
- GFR varies less than RPF when there is fall in systemic blood pressure, GFR falls less than RPF, because of efferent arteriole constriction
→ filtration fraction rises
Filterability
Filterability of solutes is determined by:
- Size/ molecular weight (MW)
- Electrical charge:
Negative charge is more difficult than positive charge, because basement membran of glomerular capillary consists proteoglican with negative charge
….. Filterability
Filterability of substances by GC decreases with increases MW
Substance
Water
Sodium
Glucose
Inulin
Myoglobin
Albumin
MW
18
23
180
5.500
17.000
69.000
Filterability
1,0
1,0
1,0
1,0
0,75
0,005
Secretion and Reabsorption
Once the glomerular filtrate is formed, then the tubular cells will:
Increase the concentration of certain substances in the filtrate by secretion
Reduce the concentration of certain substances in the filtrate by reabsorption
Secretion or reabsorption rate depending on the needs of the body of the material
Basic Mechanism of Secretion and Reabsorption
Active transport:
- primary active transport
- secondary active transport
- active transport mechanism for protein reabsorption: pinocytosis (endocytosis)
Passive transport:
- through intercellular space
- using carrier
Osmosis: water
Transport Maximum (Tm)
Limit of the rate at which the solute can be transported through active transport mechanism
Due to transport carrier system becomes saturated as tubular load increases
Passive transport does not demonstrate Tm, because the rate is determined by other factors:
- Electrochemical gradient for diffusion
- Permeability of the membrane for the substance
- The time that the fluid containing the substance remains within the tubule
This type of transport is referred to as gradient-time transport
Transport in Proximal Tubules
Proximal tubule epithelial cells are highly metabolic and have large numbers of mitochondria to support potent active transport processes
Proximal tubule epithelial cells have extensive brush border on the luminal side and also extensive labyrinth of intercellular and basal channels
extensive surface area for rapid transport
Epithelial brush border is loaded with protein carrier molecules and a large number of sodium ions
secondary active transport (co-/ counter transport)
So, it is the most active reabsorption process
Water moves across membrane by osmosis
Reabsorption in Proximal Tubule
In the first half of proximal tubule:
- sodium is reabsorbed by co-transport along with glucose, amino acids, and other solutes
- leaving behind solution that has higher chloride concentration flow to the second half of proximal tubule
In the second half of proximal tubule:
- sodium is reabsorbed mainly with chloride ions
- little glucose and amino acids remain to be reabsorbed
Secretion in Proximal Tubule
Proximal tubule is important site for secretion of many substances that must be rapidly removed from body, such as:
- organic acids and bases
- end product of metabolism
- many potentially harmful drugs or toxin
- para-aminohippuric acid (PAH)
Normal person can clear ± 90 % of PAH from plasma flowing through kidneys and excrete it into urine
So, PAH clearance can be used as index of renal plasma flow (RPF)
Transport in Loop of Henle
Loop of Henle consists of 3 functionally distinct segments:
the descending thin segment
the ascending thin segment
the thick ascending segment
The thin segments have thin epithelial membranes with no brush borders, few mitochondria , and minimal levels of metabolic activity
The thick segment has thick epithelial cells that have high metabolic activity and are capable of active reabsorption of sodium, chloride, and potassium
…..Transport in Loop of Henle
The descending thin segment:
- Highly permeable to water
- Moderately permeable to most solutes, including urea and sodium
The ascending thin segment:
impermeable to water
- reabsorption capacity is very low
The thick ascending segment
impermeable to water
highly metabolic → active reabsorption of Na, Cl, K (25%)
- has Na-H counter transport mechanism
↓ tubular fluid becomes very dilute
Transport in Distal Tubules
The very first portion of distal tubule forms part of juxtaglomerular complex that provides feedback control of GFR and blood flow in the same nephron
The next early part of distal tubule is highly convoluted and has many of the same reabsorptive characteristics of the thick segment of ascending limb of loop of
Henle:
- avidly reabsorbs most of ions including Na, Cl, K
- virtually impermeable to water and urea
Also dilutes the tubular fluid
Transport in Late Distal Tubules and Cortical Collecting Tubule
The second half of distal tubule and the subsequent cortical collecting tubule have similar functional characteristics
Anatomically, composed of 2 distinct cell types:
> principal cells: reabsorb Na + & water, and secrete K +
> intercalated cells: reabsorb K + & HCO
3
-
, and actively secrete H + → play a key role in acid-base regulation
Almost completely impermeable to urea
Rate of Na + reabsorption and K + secretion is controlled by aldosterone and their concentration in body fluids
Permeability to water is controlled by ADH (vasopressin) → important mechanism for controlling the degree of dilution or concentration of urine
Transport in Medullary Collecting Duct
Play an extremely important role in determining the final urine output of water and solutes
Epithelial cells are nearly cuboidal with smooth surfaces and relatively few mitochondria
Permeability to water is controlled by ADH
Permeable to urea → reabsorbed into medullary interstitium → raise osmolality → concentrated urine
Capable of secreting H + → also play key role in acidbase regulation
Countercurrent Mechanism
Countercurrent mechanism produces hyperosmotic renal medullary interstitium
concentrated urine
Countercurrent mechanism depends on special anatomical arrangement of the loops of Henle and vasa recta (specialized peritubular capillaries of renal medulla)
Basic requirements for forming a concentrated urine:
- High level of ADH increases permeability of distal tubules and collecting ducts to water
avidly reabsorb water
- High osmolarity of renal medullary interstitial fluid
osmotic gradient necessary for water reabsorption to occur in the presence of high levels of ADH
…..Countercurrent Mechanism
Major factors that contribute to build up of solute concentration into renal medulla:
1. Active transport of Na + and co-transport of K + , Cl
and other ions out of thick limb into medullary interstitium
2. Active transport of ions from collecting ducts into medullary interstitium
3. Passive diffusion of large amounts of urea from inner medullary collecting ducts into medullary interstitium
4. Diffusion of only small amounts of water from medullary tubules into medullary interstitium, far less then reabsorption of solutes into medullary interstitium
Tubule Characteristics – Urine Concentration
Segment of Tubules
Thin descending limb
Thin ascending limb
Thick ascending limb
Distal tubule
Cortical collecting tubule
Inner medullary collecting tubule
Active
NaCl
Transport
0
Permeability
H
2
O NaCl Urea
+++++ + +
0
+++++
0
0
+
0
+
0
+
+
+
+ ADH 0
+ ADH 0
0
0
+ ADH 0 +++