Ch 20: The Blood - Bloodhounds Incorporated
advertisement
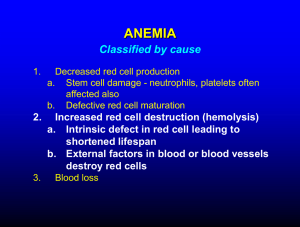
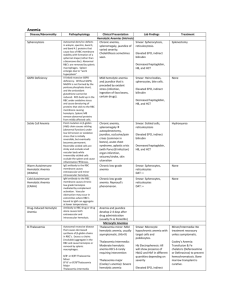
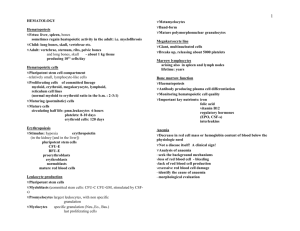
Blood Plasma and Cellular Elements of Blood Hematopoiesis RBC Physiology Coagulation Blood = connective tis sue extracellular matrix: Plas m a color ?? volume ?? specialized cells: (Form e d e le m e nts ) RBCs WBCs Plate le ts Plasma Water Plasma proteins • Albumin (60%) Osmotic Gradient • Globulins (Ab) • Fibrinogen Molecules • • • • Electrolytes Nutrients Trace Elements Dissolved gases Serum = Plasma – Clotting factors Hem(at)opoiesis = Blood Cell Formation Few uncommitted, pluripotent stem cells in red bone marrow throughout life time (Fig 16-2) Controlled by cytokines, e.g. • Erythropoietin (hormone or cytokine?) • CSFs (Colony-stimulating factor)and ILs (interleukins): e.g. M-CSF, IL-3 (= multi CSF) Neulasta (pegfilgrastim) is a CSF • Thrombopoietin (TPO) Some Terminology: • Anemia vs. Leukemia vs. leukocytosis vs. leukopenia Any of various acute or chronic neoplastic diseases of the bone marrow in which unrestrained proliferation of white blood cells occurs, usually accompanied by anemia, impaired blood clotting, and enlargement of the lymph nodes, liver, and spleen. Leukemias (“white blood”) group of cancerous conditions of WBCs. Named according to the abnormal WBC type primarily involved (e.g. lymphocytic leukemia, myelocytic leukemia). Leukemia is acute (quickly advancing - mostly in children) if it derives from blast-type cells like lymphoblasts, and chronic (slowly advancing - mostly in adults) if it involves proliferation of later cell stages like myelocytes. Leukemia, lymphoma and myeloma are cancers that originate in the bone marrow (in the case of leukemia and myeloma) or in lymphatic tissues (in the case of lymphoma). Leukemia, lymphoma and myeloma are considered to be related cancers because they involve the uncontrolled growth of cells with similar functions and origins. The diseases result from an acquired (not inherited) genetic injury to the DNA of a single cell, which becomes abnormal (malignant) and multiplies continuously. The accumulation of malignant cells interferes with the body's production of healthy blood cells and makes the body unable to protect itself against infections. Leukemia - Leukemia is a malignant disease (cancer) that originates in a cell in the marrow Non-Hodgkin Lymphoma - Lymphoma is a general term for a group of cancers that originate in the lymphatic system Hodgkin Lymphoma - Hodgkin lymphoma (also known as Hodgkin's disease) is a specialized form of lymphoma and represents about 8 percent of all lymphomas diagnosed each year Myeloma - Myeloma is a cancer of plasma cells, a type of white blood cell found in many tissues of the body, but mainly in the marrow Myelodysplastic Syndromes - Myelodysplastic syndromes are a group of diseases that originate in an early bloodforming cell in the marrow Leukopenia at http://www.merck.com/pubs/mmanual/section11/chapte r135/135a.htm EPO Regulates RBC Production “Hormone” synthesized by kidneys in response to hypoxemia EPO gene cloned in 1985 Recombinant EPO now available (Epogen, Procrit) Use in therapy, abuse in sport • Bone marrow damage from chemotherapy • Chronic renal failure Your book calls it a cytokine because it is made on demand, not stored. (p540). Trivia Dept.: Neulasta® (pegfilgrastim) stimulates production of WBC Running Problem: Blood Doping The Erythrocyte (RBC) Biconcave Disk, 7 μ diameter, Carry O2 120 day lifespan No mitochondria, no nucleus • ATP from glycolysis Bag of Hb HCT = hematocrit = PCV MCV-Mean Cell Volume • ↓ in Fe-deficiency anemia Hemoglobin (Hb) [Hb] often reported in CBC • Four globulin proteins (Fig 18-8) Two αTwo βEach has the heme group Heme is a porphyrin that binds Fe Fe is considered a trace mineral • Meat, beans, spinach • Stored in liver, “recycled” • Fe deficiency Hemoglobin (Hb) Synthesis and Breakdown Requires iron (Fe) + Vit. B12 (cobalamin) Reversible binding between Fe & O2 Hb Breakdown: • Hb → Bilirubin → bile. Hyperbilirubinemia • Too fast causes icterus (jaundice) • HbA vs. HbF Fetal Hb has two chains instead of two chains HbF is designed to steal oxygen from maternal blood in placenta. Replaced shortly after birth. CO is a product of incomplete combustion (complete combustion producesCO2 and H2O.) This obviously includes exposures to fires by victims and fire fighters but also includes smokers (cigars produce more CO than cigarettes - up to 20% CO Hb possible). Exhaust fumes are a common source of CO exposure. A recent report detailed high levels of CO exposure in enclosed pickup truck beds from a backdraft of exhaust fumes into the back of the truck. Carbon monoxide also binds coordinately to heme iron atoms in a manner similar to that of oxygen, but the binding of carbon monoxide to heme is much stronger than that of oxygen. The preferential binding of carbon monoxide to heme iron is largely responsible for the asphyxiation that results from carbon monoxide poisoning. RBC Disorders Too high PCV: • Polycythemia vera • Dehydration (PCV ~ 60-70%) Anemias (O2 carrying capacity of blood too low) • Hemorrhagic anemia Fe deficiency anemia • Hemolytic anemia, due to genetic diseases (e.g. Hereditary spherocytosis) or infections • Pernicious anemia Vit. B12 Deficiency • Aplastic anemia • Renal anemia ↓ EPO • Sickle Cell Anemia Polycythemia vera most commonly due to bone marrow cancer. Hematocrit can become as high as 80%. Secondary poycytemia when less oxygen is available (high altitudes) or EPO production increased. Polycythemia vera is a clonal stem cell disorder characterized by excessive erythrocyte production. Its etiology is not fully established, but hypersensitivity to interleukin-3 may play a role in the sustained erythrocytosis observed in this disease. Polycythemia vera usually occurs within the age range of 20-80, with 60 being the mean age of onset. The disease is slightly more common in males than in females. Clinical features include headaches, weakness, weight loss, and pruritus (itching without visible eruption on the skin). Major Criteria total RBC vol men > 36 mg/kg; women >32 mg/kg arterial 02 saturation > 92% Splenomegaly Fe deficiency anemia USUALLY A SECONDARY RESULT OF HEMORRHAGIC ANEMIAS. But also due to inadequate intake of iron containing foods or impaired absorption. Results in microcytes (pale small RBCs) Pernicious anemia (p.621) leads to large pale cells due to developing RBCs not dividing. Aplastic anemia due to some toxic chemicals and drugs and ionizing radiation. E.g.: arsenic, chloramphenicol. Fallout from nuclear bomb, excessive exposure to X-rays. Cancer and cancer chemotherapy. Marrow destruction of course affects all formed elements, anemia is just one symptom. Sickle cell anemia HbS instead of normal HbA. One in 100 black newborns in US. Malaria connection: RBCs loose potassium which is essential for survival of parasite (plasmodium) Platelets = Thrombocytes Megakaryocyte (MK) is polypoid. Mechanism? MK produces ~ 4,000 platelets • Lifespan 10 days. Platelets contain granules filled with clotting proteins & cytokines Activated when blood vessel wall damaged Hemostasis = Opposite of hemorrhage stops bleeding too much bleeding Too much hemostasis thrombi / emboli Too little hemostasis Three major steps: 1. Vasoconstriction 2. Platelet plug Temporarily blocks the hole 1. 3. Coagulation cascade (= clot formation seals hole until tissues repaired) 1. 4. Platelet-derived cytokines further the process Two pathways: Extrinsic and Intrinsic After vessel repair, plasmin dissolves the clot Steps of Hemostasis Vessel damage exposes collagen fibers Platelets adhere to collagen & release factors + feedback loop local vasoconstriction decreased blood flow & platelet aggregation platelet plug formation Steps of Hemostasis cont. 1. Two coagulation pathways converge onto common pathway 1. 2. 2. 3. Intrinsic Pathway. Collagen exposure. All factors needed are present in blood. Slower. Extrinsic Pathway. Uses Tissue Factors released by injured cells and a shortcut. Usually both pathways are triggered by same tissue damaging events. The different factors can be subject to a variety of problems 1. 2. Hemophilia Hypercoagulable states Vit K needed for synthesis of several clotting factors Structure of Blood Clot Plasmin, trapped in clot, will dissolve clot by fibrinolysis SEM x 4625 Clot formation limited to area of injury: Intact endothelial cells release anticoagulants (heparin, antithrombin III, protein C). Clot Busters & Anticoagulants Dissolve obsolete or unwanted clots Prevent coagulation by blocking 1 or more steps in fibrin forming cascade Enhance fibrinolysis Inhibit platelet adhesion plug prevention Urokinase, Streptokinase & t-PA Examples: Examples: Coumadin (warfarin) blocks Vit K EDTA chelates Ca2+ Aspirin prevents platelet plug Coumarin and warfarin block Vit K action (Vitamin K is cofactor in synthesis of several coagulation factors. Ca chelators (EDTA and citrate) only in vitro Heparin inhibits activity of thrombin (produced by basophils) Aspirin prevents platelet plug fomation Hemophilia It is sometimes called Christmas disease after Stephen Christmas, the first patient described with this disease. In addition, the first report of its identification was published in the Christmas edition of the British Medical Journal. In more recent history, royal watchers know that Queen Victoria of Britain's son Leopold had hemophilia, and that two of her daughters, Alice and Beatrice, were carriers of the gene. Through them, hemophilia was passed to the royal families in Spain and Russia, leading to one of the most famous young men with the disease, Tsar Nicholas II's only son Alekei.