Melanin black polymers
advertisement

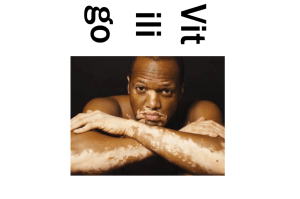
Vitiligo, Depigmentation and Monobenzone VITILIGO Occurs worldwide about 1% of the population, mostly between the age of 10-30 Chronic skin disease Other name = Leukoderma White spots occur when the skin no longer forms melanin (pigment that determines the color of your skin, hair, and eyes) The white patches of irregular shapes begin to appear on your skin Total absence of melanocytes microscopically Cont….. Associated with three other autoimmune diseases: 1. Addison’s Disease 2. Hyperthyroidism 3. Pernicious Anemia A skin biopsy may be required to rule out the other causes of pigment loss. CLINICAL FEATURES Totally amelanotic macule (patch) surrounded by normal skin Vitiligo macules characteristically have fairly discrete margins and they are round, oval or linear in shape Lesions enlarge centrifugally over time, but the rate may be slow or rapid Vitiligo macule patches ranges from millimeter to centimeter in size CYTOLOGY •Normal skin is pigmented with melanin that is produced by melanocytes •Detection by Masson Silver Stain •Therefore white spots are due to melanocyte death DISTRIBUTION PATTERN OF VITILIGO Focal •a few isolated lesions Segmental •unilateral distribution Vulgaris • fingers and around mouth Universal • total depigmentation Sub types of Vitiligo Differ by anatomical location, and size of lesions Focal – A few isolated lesions, most common in children Segmental – unilateral distribution Acrofacial – fingers and periorificial areas Universal – almost total depigmentation Generalized – most common, symmetrical distribution, occurs symmetrically on both sides of the body Mucosal – Depigmentation of only the mucous membrane Causes of Vitiligo HYPOTHESIZED CAUSES Autoimmune theory: Cell mediated immune process Biochemical Theory Oxidative Stress Theory Melanin Melanin is black pigment of skin, hair & eyes Synthesis occurs in melanosomes present in melanocytes. Tyrosine is the precursor of melanin and tyrosinase is the enzyme involved in it’s formation Melanochromes formed from tyrosine polymerizes to form melanin polymers MELANIN SYNTHESIS Tyrosine DOPA Dopamine Leucodopachrome 5,6-Dihydroxyindole Cysteine Melanin red polymers Indole 5-6-quinone Melanochrome Melanin black polymers THE PATHOGENESIS OF VITILIGO Chemical Melanocytotoxin: 1) Melanin synthesis can be triggered by: Sunburn, skin injury or exposure to cytotoxic compound stimulate melanin synthesis Melanocyte stimulating hormone induced by UV exposure Cytokines produced during emotional stress or physical trauma 2) Specific Quinones (Dopa Quinone) and Indoles (Dihydroxy indoles) are generated as intermediates during melanin synthesis 3) Quinones & Indoles, if abundant in the cells, can readily oxidize either enzymatically or spontaneously and produce reactive oxygen species and ultimately induce apoptosis. Apoptosis in Vitiligo Melanocytes 1. Exposure of melanocytes to pigment inducers via action of tyrosinase related protein 1 (Tyrp 1) results in generation of intracellular quinone 2. Reactive oxygen species (ROS) forms 3. ROS stimulates the apoptotic pathway 4. Potentially could lead to cell death or interact with endogenous or regulated antioxidants Essentials of Vitiligo Etiology in Diagram 1. Stress to the skin in form of wound, burn, excessive sun exposure or contact with bleching phenol 2. Differential gene expression among melanocytes 3. Inflammatory infiltrate of T cells & macrophages 4. Further induce melanocyte apoptosis TREATMENT SCHEME FOR VITILIGO Where Depigmentation Therapy Required Generalized vitiligo •Typical appearance of a man with generalized vitiligo affecting the skin around eyes, nose, mouth, and the chest and hands List of Depigmenting Agents MONOBENZONE Monobenzyl ether of hydroquinone (MBEH) Chemical Name: P- (Benzyloxy) - Phenol Oliver et al. discovered it on 1939 Acts as a skin sensitizer Topical application increases the excretion of melanin from melanocytes in animal Depigmentation spreads to distant sites unexposed to Monobenzone, indicating that it induces a progressive systemic reaction against melanocytes Mechanism of Action Many theories have been proposed: MBEH reacts with tyrosinase, the key enzyme in melanin synthesis, to form a reactive quinone product. This quinone metabolite in turn binds covalently to cysteine residues in tyrosinase proteins through the sulfhydryl (-SH) group to form hapten-carrier complexes, i.e., generation of neo-antigens in the tyrosinase peptide chain occurs which excites a systemic, melanocyte destructive, inflammatory response. MBEH induces cellular oxidative stress in exposed pigmented cells by producing reactive oxygen species (ROS) such as peroxide. This induces lysosomal degradation of melanosomes by autophagy, in addition to disruption of melanosomal membranes and melanosome structure. This is followed by increased surface expression of melanosomal antigens by both major histocompatibility complex (MHC) class I and II routes and initiation of melanocyte Ag-specific T-cell responses. Cont…. ROS generation also results in release of tyrosinase and MART-1 antigen containing exosomes which further contributes to immune response. Rapid and persistent innate immune activation also occurs in MBEH-exposed skin. MBEH is a contact-sensitizer inducing a type IV delayed type hypersensitivity response against the quinone hapten mentioned earlier. This depends on the production of proinflammatory cytokines such as interleukin (IL)-1b and IL-18 by the Langerhans cells or keratinocytes. Electron Microscopy Necrotic changes consisting plasma membrane and cytoplasmic disintegration DNA fragmetation treated skin within Monobenzyl Ether of Hydroquinone Apoptosis is shown in confocal microscopic images of explant cultures exposed to 5 ml of 250mM MBEH (Monobenzyl Ether of Hydroquinone) for 24 hours. Side Effects of Monobenzone Mild burning, irritation, redness, cracking, or peeling of the treated skin may occur. If any of these effects persist or worsen, doctor needs to be informed. Note: Get emergency medical help if you have any of these signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue,or throat. Why Monobenzone???? MBEH is the most widely used depigmenting agent Monomethyl ether of Hydroquinine / 4-Methoxy Phenol requires longer time prior to the onset of visible depigmentation Application of 88% Phenol solution on large areas proved to be toxic to Liver and Kidney. Cardiovascular shock, cardiac arrythmias, bradycardia as well as metabolic acidosis with in 6 hours of skin peeling procedures with phenol. Different type of lasers are selectively destructive to melanocytes but technique is painful and expensive. Moreover these are more efficient in patients with Koebner Phenomenon (skin lesions which appear at the site of injury). Moreover treatment is only available in the clinic. Patients with negetive Koebner may relapse. Cyrotherapyrequires an experienced person hence treatment is hospital based. It gives edema, pain and bulla formation as side effects.Moreover it is suitable for small lesions since single sitting can not be utilized for extensive viiligo. Topical Imatinib, Imiquimod and Diphencyprone may be considered as potential depigmenting agents, but require further investigation Efficacy of Monobenzone Therapy Residual patches of vitiligo affecting more than 70% of her skin surface Depigmentation after topical application of 20% Monobenzone daily during 8 months Why Treatment is Important??? Although vitiligo is usually not harmful medically and causes no physical pain, its emotional and psychological effects can be devastating. In India, vitiligo patients, especially women, are sometimes discriminated against in marriage. Developing vitiligo after marriage can be grounds for divorce. White patches of vitiligo can affect emotional and psychological well-being and self-esteem. People with vitiligo can experience emotional stress Conclusion Most commonly acquired Hypomelanosis. Known as ‘‘ Ven kushtam’’ in India, means White Leprosy. Extremly disfiguring, leading to significant patient morbidity. Low self esteem, poor body image and poor quality of life has been found in patients. Depigmentation is the only option when more than 70% of the body covered with vitiligo. Monobenzone induce depigmentation that is clinically and histologically indistinguishable from vitiligo vulgaris. Superiority of Monobenzone comes when it gives a uniform white color References JG van den Boorn et al. Effective Melanoma Immunotherapy in Mice by the Skin-Depigmenting Agent Monobenzone and the Adjuvants Imiquimod and CpG. Plis One 2010;5(5) : 1-12 JG van den Boorn et al. Autoimmune Destruction of Skin Melanocytes by Perilesional T Cells from Vitiligo Patients Journal of Investigative Dermatology 2009; 129: 2220-32 Thomas J. Childhood Vitiligo – An Overview. Journal of the Indian Society of Teledermatology, 2008;2(4) : 1-6 Van Geel et al. In vivo vitiligo induction and therapy model: double-blind, randomized clinical trial. Pigment Cell Melanoma Res. 2011;25: 57–65 Gupta D, Kumari R and Thappa DM. Depigmentation therapies in Vitiligo. Indian Journal of Dermatology, Venereology and Leprology 2012;78(1) : 49-58 Draelos ZD. The combination of 2% 4-hydroxyanisole (mequinol) and 0.01% tretinoin effectively improves the appearance of solar lentigines in ethnic groups Al-Bayati MA. Analysis of causes that led to the development of vitiligo in Jeanett’s case with recommendations for clinical tests and treatments. M.A. AlBayati/Medical Veritas 2007; 4: 1251–62 Westerhof W. Vitiligo Management Update. Skin Therapy Letter 2000; 6(5): 1-2 Schallreuter KU et al. Vitiligo pathogenesis: autoimmune disease, genetic defect, excessive reactive oxygen species, calcium imbalance, or what else? Experimental Dermatology 2008; 17: 139–60. Nordlund JJ, Le Poole C, and Boissy RE. Clinical and Basic Immunodermatology 2008, 4, 661-89 Hariharan V et. al. Monobenzyl Ether of Hydroquinone and 4-Tertiary Butyl Phenol Activate Markedly Different Physiological Responses in Melanocytes: Relevance to Skin Depigmentation. Journal of Investigative Dermatology 2010; 130:211–20. Kavuossi H. Induction of depigmentation in a universal vitiligo patient with combination of cryotherapy and phenol. Journal of Pakistan Association of Dermatologists 2009; 19: 112-4. Shajil EM et al. Vitiligo: pathomechanisms and Genetic Polymorphisms of genes. Indian Journal of Experimental Biology 2006;44:526-39 www.clinicalpharmacy.ir/Upload/Modules/Contents/Vitiligo.pdf Depigmenting Agents: Skin-lightening Products for Patients with Facial Melasma. European Dermatology, 2010;5:68–73 Lotti T et al. New and Experimental Treatments of Vitiligo and Other Hypomelanoses. Dermatol Clin 2007;25 :393–400 Falabella R and Barona MI. Update on skin repigmentation therapies in vitiligo. Pigment Cell Melanoma Res. 2008;22: 42–65 Petit L and Pierard GI. Skin Lightening products revisited. International Journal of Cosmetic Science 2003;25:169-81 Zanini M. Depigmentation therapy for generalized vitiligo with topical 88% phenol solution. An Bras Dermatol. 2005;80(4):415-6. www.msu.edu/~comptona/Vitiligo/Vitiligo%20Vulgaris.ppt Remember, A little Consideration, A Little Thought for them makes all the differences. No wonder they are one amongst us. And last, but not the least, Monobenzone- a scientifically established treatment for vitiligo. THANK YOU Puneet Laboratories Pvt. Ltd.