service provision - Quality Improvement Hub
advertisement

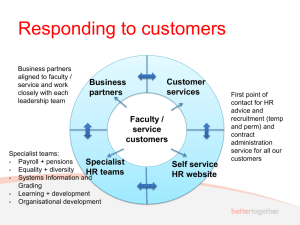
Experiences of dermatology services transformation Julia Schofield, Principal Lecturer University of Hertfordshire Consultant Dermatologist, United Lincolnshire Hospitals NHS Trust Experiences of dermatology services transformation • What did the service look like before the redesign work? • What changes were made and how were they made? • What the service looks like now • Where there any barriers and how were they overcome? • Examples of models of service from England How best to answer these questions? Setting the scene 1997-2010 The Blair years, the NHS and Dermatology : period of unprecedented reform Reform & modernisation: early stages • Background of long waiting lists and poor access to services • NHS Modernisation agency Action on Dermatology (2000-2003) • Action on Plastic Surgery (2003-2005) • Pilot site work and Good Practice Guidance • Role of GPwSIs and extended role practitioners • Lack of good evidence for what worked Trends in the number of dermatology patients waiting longer than 26 and 13 weeks to be seen using fourth quarter data 1999-2007, England source www.performance.doh.gov.uk/waitingtimes 30,000 25,000 13 to <26 20,000 >26 15,000 10,000 5,000 0 Q4 99/00 Q4 00/01 Q4 01/02 Q4 02/03 Q4 03/04 Q4 04/05 Q4 05/06 Q4 06/07 So what have we learnt that is important and where is the evidence? The commissioning cycle Service redesign cycle The 2009 Health Care Needs Assessment • The burden of disease: how much, how expensive, impact? • How we manage the burden: services available and their effectiveness • Recommendations for models of care based on the EVIDENCE http://www.nottingham.ac.uk/scs/documents/documentsdivisions/documentsdermatology/hcna skinconditionsuk2009.pdf Structure of the document: chapters 1. Introduction 2. Burden of skin disease 3. NHS reform and its impact 4. Services available and their effectiveness 5. Models of care and organisation of services 6. Specific skin disease areas 7. Recommendations Lots of references! Linking the evidence to service redesign: ASSESSING NEED • • • • Coding systems poor, underestimate problem Skin disease is very common Lots of people self care and buy OTC products 24% of the population seek medical advice about a skin condition each year (12.9 million) • Commonest reason people present to a GP with a new problem Skin disease seen by specialists • Limited information, good scottish data* • About 6.1% of people with skin disease are referred to see a specialist • 35-48% referrals are skin lesions, more in coastal areas • Ever increasing referrals to specialists • Eczema, acne and psoriasis commonly seen • Patients still admitted *Benton, EC, Kerr, OA, Fisher, A, Fraser, SJ, McCormack, SKA, Tidman, MJ (2008) The changing face of dermatological practice: 25 years' experience. British Journal of Dermatology, 159, 413-8. Need: summary of key messages 3752 deaths due to skin disease Self reported/ self managed skin disease 50% population approx 25 million 0.75 million people with skin disease referred for NHS specialist care, 1.5% 24% population, 12.9 million seeking Primary Care (England and Wales) Linking the evidence: SERVICE PROVISION • • • • • We MUST define the level of care and the location Confusion about terms Primary care means ‘first point of contact care’ Secondary care means ‘specialist care’ Too much talk of ‘shift’ without understanding the meaning Define LEVELS of care: self care, generalist, specialist, supra-specialist From Skin conditions in the UK: a Health Care Needs Assessment Schofield et al 2009 Linking the evidence: service provision Generalist care • Patients like to be treated by their GP • GP diagnostic skills for skin lesions are not great • Standards for GP skin surgery need to be improved • Up-skilling of Practice Nurses limited benefit • Community specialist outreach nursing services effective for chronic skin disease Linking the evidence: service provision Specialist care • Dermatologists should be diagnosing the skin lesions: they are good at it • Dermatologists can prevent hospital admissions for some conditions • If GPwSIs are to be used, they need to be accredited • Specialist nurse services for prediagnosed conditions are effective Services available: who sees what and where? Primary care Skin infections WHY? Specialist care Skin lesions 45-60% 31-59% are for diagnosis – skin lesions even higher Service provision: the diagnostic bottleneck Treatment Surgery Specialist opinion, diagnostic service CORRECT DIAGNOSIS = CORRECT MANAGEMENT Patients with skin disease requiring diagnosis and management Linking the evidence: DECIDING PRIORITIES MUST do’s • NICE guidance includes skin cancer, biologics for psoriasis, atopic eczema • DH access targets 31/62 days for cancer • 18 week patient journey • Choose and Book • Care Closer to Home recommendations Linking the evidence: deciding priorities Inequity of access need vs demand • Variable low priority frameworks across England • Skin surgery • Lymphoedema services • Botulinum toxin services for sweating • ‘One pot spent well’ • Decisions should be based on the evidence base What is need? Need is ‘the ability to benefit from care’ Williams HC. J Roy Coll Physicians 1997;31:261-2 The use of isotretinoin to treat acne The use of the biological agents to treat psoriasis Demand and supply Demand = “that which is asked for” Supply = “that which is provided for” Williams, HC. J Roy Coll Physicians 1997;31:261-2 Seborrhoeic keratoses – demand or need? How to save a billion (part II) • Up to £700m could be saved if PCTs decommissioned some procedures: “relatively ineffective” Max potential reduction in procedures (%) Max potential savings (£m) Tonsillectomy 90 45 Back pain injections & infusion 90 24 Grommets 90 21 Knee washouts 90 20 Aesthetic breast surgery 80 18 Varicose veins 80 18 Inguinal, umbilical & femoral hernias 50 50 Minor skin surgery for non cancerous lesions 25 74 “Potentially cosmetic” Linking the evidence: DESIGNING SERVICES • • • • • Emphasis on rapid access to diagnosis Right place, right person, first time Range of national guidance about models of care Integrated care Local specialist services with links to regional and national specialist services • Services for sick patients in hospital • Day treatment OP phototherapy services • Patients must be involved in the design of services Care Closer to Home 2007 Figure 2: Dermatology patient journey (source: modified from Model of Integrated Service Delivery. Skin Care Campaign 2007) Patient support groups The Patient Drop-in Centre The facility to refer directly to secondary care services is essential 2 week wait cancer pathway Pharmacist Discharge GP Referral management* Diagnosis and treatment GPwSI/PwSI (where appointed) Secondary care * Where referral management schemes are in place it is essential that these are led by experienced specialist clinical triage performed daily to reduce delays Tertiary (supra-specialist care) Diagnosis and specialist treatment Skin lesion models: separate diagnosis and management 18 week skin lesion pathway Linking the evidence: designing services • Shifting care to community settings does not necessarily reduce activity or cost • There is a link between a reduction in wait times and increased referral rates • National standards and review are in place for skin cancer services Linking the evidence: designing services • GPwSI services improve access but do not reduce cost • Specialist nurses working with specialist teams are effective • Specialty and Associate Specialist doctors are interested in working in new models of care Linking the evidence: designing services • Teledermatology useful for remote areas • ‘Store and forward’ digital image and referral useful • Clinically-led guidelines may be helpful but a lot of work! • Referral management services (RMS) evidence free zones*. ? Role of Tier 2 services/ Clinical Assessment and Treatment services Davies, M, Elwyn, G (2006) Referral management centres: promising innovations or Trojan horses? BMJ, 332, 844-6. Referral management services Referral management centres • Paper/electronic process • Count referrals • Assess quality and reduce inappropriate referrals • Redirect referrals to appropriate service • May lack clinical input Referral management services DH guidance 2006 • Must not lengthen patient journey • Must carry clinical support • Should confer real diagnostic or treatment benefit • Not be imposed without agreement • In England largely financially driven Experience of a Clinical Assessment and Treatment Service in Hertfordshire • Specialist led, GPwSIs, consultant outreach, specialist nurses • Specialist triage • Community settings • Routine, straightforward dermatology • Patients happy, good service • Robust governance and quality Dermatology Service from September 2007 Referral to CATS service Other referrals Consultant/Associate Specialist triage Triage CHOICE ROUTINE ROUTINE Skin surgery Needs specialist services Pre-diagnosed N/L eczema N/L psoriasis N/L leg ulcer CHOICE GPwSI Consultant outreach Urgent C H O I C E Wellswood House Borehamwood 2 week wait Consultant appointment OUTCOME Discharge or follow up Impact on secondary care referral rates 400 350 300 250 200 150 100 50 0 Sept Oct Nov Dec Jan Feb Mar Pre-CATS CATS period Apr May June July Aug BUT: total referral activity including CATS referrals increased 600 Pre-CATS CATS period TOTAL 500 400 300 200 100 0 Sept Oct Nov Dec Jan Feb Mar Apr May June July Aug Linking the evidence: SHAPING THE STRUCTURE OF THE SUPPLY (!) • Quality same wherever and whoever provides the service (OHOCOS 2006) • Joined up services: integrated models • Local resources local solutions • Robust standards of accreditation, DH guidance • Competency based assessments supervised practice Linking the evidence: MANAGING THE DEMAND • General Practitioner will remain the gatekeeper • Resources are finite and demand will need to be managed • No evidence that strategies to date are effective • Priority setting may be the key • Need vs demand increasingly an issue GP as gatekeeper: education and training • Limited undergraduate training • Postgraduate training not compulsory • GP curriculum could map better to what is seen in practice • Training and education important • Not a short term solution The final piece of evidence to think on 30,000 13 to <26 >26 25,000 18% more patients seen 5.6% more new patients seen Fewer people waiting 20,000 15,000 10,000 24% rise in consultant numbers 5,000 0 Q4 99/00 Q4 00/01 Q4 01/02 Q4 02/03 Q4 03/04 Q4 04/05 Q4 05/06 Q4 06/07 Implementing the 18 week target Presented the evidence • Service redesign cycle • Needs Assessment • Burden of skin disease • Service provision • Models of care • Referral management No magic wand! THANK YOU The HCNA is available free at: http://www.nottingham.ac.uk/scs /documents/documentsdivisio ns/documentsdermatology/hcn askinconditionsuk2009.pdf Hard copies can be purchased from the Centre of Evidence based Dermatology for a nominal sum from douglas.grindlay@nottingham. ac.uk