Unit 29 - Respiratory Lung and Gas Exchange Disorders
advertisement
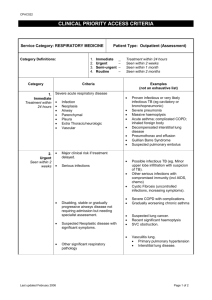
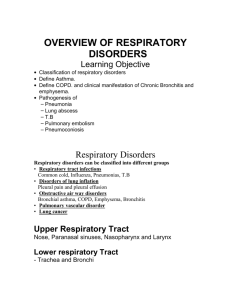
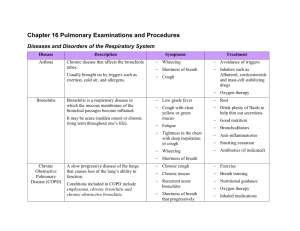
TRANSITION SERIES Topics for the Advanced EMT CHAPTER 29 Respiratory Emergencies: Lung and Gas Exchange Disorders Objectives • Identify pathophysiologic changes due to diseases that hamper gas diffusion or lung compliance. Introduction • This topic deals with disorders that alter lung compliance or the ability of the alveoli to diffuse gas. • Compliance refers to the ability of lung tissue to expand when air flows in. • Alveolar issues are those that inhibit or prohibit normal gas exchange with the blood stream. Epidemiology • 1.5 million people are diagnosed with emphysema. • Pulmonary edema afflicts 1%-2% of the general population. • 250,000 cases of pulmonary emboli a year. • Other etiologies like pneumothorax and cystic fibrosis occur also. Pathophysiology • Compliance – Refers to the ability of the lungs to stretch as air enters the passageways. – “Stiff” lungs are difficult to ventilate. • External respiration – Exchange of gases in the alveoli. • Internal respiration – Exchange of gases at the tissue capillary level. Pathophysiology (cont’d) • Emphysema – Loss of lung tissue elasticity – Destruction of alveolar surfaces – Gross disturbances in gas exchange Pathophysiologic changes in emphysema include decreased surface area of the alveoli. Pathophysiologic changes in emphysema include decreased surface area of the alveoli. Pathophysiology (cont’d) • Pulmonary edema – Fluid collects in alveoli due to increased hydrostatic pressure in perialveolar capillary beds. – Hinders normal gas exchange. – Primarily a gas exchange problem. – Cardiogenic and noncardiogenic causes. In pulmonary edema, fluid collects between the alveoli and capillaries, preventing normal exchange of oxygen and carbon dioxide. Fluid may also invade the alveolar sacs. Pathophysiology (cont’d) • Pulmonary embolism – Embolism in blood stream lodges in pulmonary artery. – Prohibits blood flow to a region of the lung. – Disturbance to normal V/Q ration. – Blood passes through lungs without oxygenation. A blood clot, air bubble, fat particle, foreign body, or amniotic fluid can cause an embolism, blocking blood flow through a pulmonary artery. Pathophysiology (cont’d) • Pneumothorax – Collection of air in the pleural cavity – Traumatic and nontraumatic etiologies. – Changes lung compliance. – Inability to inflate lung for diffusion to occur. – Tension versus nontension pneumothorax. In pneumothorax, the lung collapse decreases lung tissue compliance and causes a disturbance in gas exchange that leads to hypoxia. Pathophysiology (cont’d) • Cystic fibrosis – Hereditary disease. – Abnormal gene results in overproduction of mucus in the respiratory tree. – Repeated respiratory infections and scarring lead to loss of pulmonary function. Assessment Findings • General assessment findings – Common to most patients with dyspnea Changes in respiratory rate and breath sounds Accessory muscle use Tripod positioning and retractions Nasal flaring, mouth breathing Changes in pulse oximetry and vitals Skin change and mental status changes Assessment Findings (cont’d) • Additional findings with emphysema – On home oxygen – Thin, barrel chest appearance – Nonproductive cough – Diminished breath sounds – Dyspnea on exertion – Tripod positioning – Prescribed MDI or nebulizer Assessment Findings (cont’d) • Additional findings with pulmonary edema – Orthopnea – Frothy sputum with cough – Tripod positioning – Crackles and wheezing on auscultation – Distended neck veins – Tachycardia and tachypnea Assessment Findings (cont’d) • Additional findings with a pulmonary embolism – Unexplained dyspnea – Sharp, stabbing chest pain – Hematemesis – Syncope – Hypotension and cyanosis (late findings) Assessment Findings (cont’d) • Additional findings with a pneumothorax – Sudden onset of dyspnea – Sharp, localized chest pain – Diminished breath sounds on affected side – Subcutaneous emphysema Assessment Findings (cont’d) • Additional findings with cystic fibrosis – Known history of disease – Recurrent coughing of thick mucus – Rhonchi on auscultation – General malaise – GI complaints – Malnutrition and dehydration Differential Assessment Findings for Lung and Gas Exchange Disorders. Emergency Medical Care • Ensure airway adequacy. • Provide oxygen based on ventilatory need. – NRB mask at 15 lpm with adequate breathing. – PPV with 15 lpm oxygen with inadequate breathing. • Administer inhaled beta-2-specific bronchodilator if warranted. Emergency Medical Care (cont’d) • Initiate CPAP at 5-10 cm H2O per protocol for pulmonary edema patients. • Keep patient sitting upright if possible. • Provide rapid transport to the ED. Case Study • You are called for a patient complaining of respiratory distress. Upon arrival you find the patient sitting in bed, propped up by three pillows. The patient looks ashen, apprehensive, and is struggling to breathe. The respirations seem fast, but he is still speaking in normal-length sentences. Case Study (cont’d) • Scene Size-Up – Scene is safe, standard precautions taken. – Patient is 61 years old, about 200 lbs. – Entry and egress from room is unobstructed. – NOI appears to be respiratory distress. – No additional resources needed. Case Study (cont’d) • Primary Assessment Findings – Patient alert and oriented. – Airway patent and self-maintained. – Breathing adequate as evidenced by speech patterns, productive cough of frothy sputum. – Central and peripheral pulses present. – Skin is slightly ashen in color. Case Study (cont’d) • How would you categorize this patient’s stability? • What clue does the sleeping on multiple pillows provide? • What are some early differentials you are considering? Case Study (cont’d) • Medical History – Patient has had two heart attacks previously. • Medications – Lasix, potassium supplement, nitro PRN. • Allergies – None per the patient. Case Study (cont’d) • Pertinent Secondary Assessment Findings – Objective respiratory distress noted. – Inspiratory crackles with expiratory wheeze. – JVD and peripheral edema noted. – Pulse ox 92% on high-flow oxygen. Case Study (cont’d) • Pertinent Secondary Assessment Findings – No chest pain, no abdominal pain. – Patient coughs up a frothy white sputum. – B/P 168/100, HR 118 and irregular, respirations 26/min. Case Study (cont’d) • What pathologic change is causing the abnormal breath sounds? • What respiratory condition does this patient likely have? • What would be three assessment findings that could confirm your suspicion? Case Study (cont’d) • How would you best ascertain if this patient is breathing adequately? • Given this patient’s presentation, would it be beneficial to give him nitroglycerin? Case Study (cont’d) • Care provided: – Patient placed on high-flow oxygen. – High-Fowler position on wheeled cot. – CPAP initiated at 10 cm H20. Case Study (cont’d) • What are the reasons for the following interventions provided to this patient? – High-flow oxygen – Fowler positioning – CPAP administration Summary • Compliance disorders make ventilation difficult, impairing normal oxygenation. • Diffusion disorders make O2 and CO2 transfer across the alveolar membrane difficult, impairing normal oxygenation. Summary (cont’d) • The role of the Advanced EMT is to identify these problems and provide appropriate interventions to improve oxygenation and ventilation.