Preparing for pre-exposure prophylaxis
(PrEP) to prevent HIV infection
James Wilton
Project Coordinator
Biomedical Science of HIV Prevention
jwilton@catie.ca
2
HIV/AIDS in Canada
• Number of people living with HIV
• 57,000 in 2005
• 65,000 in 2008
• 2,200 to 4,200 infected in 2005
• 2,300 to 4,300 infected in 2008
•
•
•
•
MSM (44%)
IDU (17%)
Women (26%)
Aboriginal (12.5%)
Source: Public Health Agency of Canada
2
3
Improving HIV prevention
1.
Do better with the strategies that we already have
2.
Develop new biomedical technologies to prevent HIV
3.
Adopt a more comprehensive approach to HIV prevention
3
Turning to antiretrovirals for prevention
The use of antiretrovirals for prevention by…
1. HIV-positive individuals to reduce their risk of
transmitting HIV
– Treatment as prevention
2. HIV-negative individuals to reduce their risk of
infection
– Post-exposure prophylaxis (PEP)
– Pre-exposure prophylaxis (PrEP)
4
What is pre-exposure prophylaxis (PrEP)?
• Pre
Before (and after)
• Exposure
When a fluid containing HIV comes into contact with
mucous membranes or non-intact skin
• Prophylaxis
An action taken to prevent infection or disease
5
What is PrEP to prevent HIV infection?
•
The ongoing use of one or two antiretrovirals by HIVnegative individuals starting before an exposure and
continuing afterwards
•
A potential option to prevent infection from ongoing
exposures to HIV during periods of risk
•
A recently proven strategy still being studied
•
PrEP is currently unapproved by Health Canada
6
How does PrEP work?
• Infection does not occur instantly after an
exposure to HIV
• The virus needs to spread throughout
the body
• This may take up to 3 days after the
exposure
• The “window of opportunity” for PrEP
• The brief period of time - after an
exposure - where HIV has not yet
spread throughout the body
• During this time, PrEP may be able to
stop HIV from causing an infection
7
Potential types of PrEP
How are the antiretrovirals
used?
• Oral pill
• Topical gel (microbicide)
•Rectal
•Vaginal
• Injection
• Intravaginal ring
How often are the
antiretrovirals used?
• Daily
• Intermittently
• Coitally (before/sex)
How many antiretrovirals are
used?
• Single
• Combination
What antiretrovirals are used?
• Over 25 available
8
What concerns does the use of PrEP raise?
• Side-effects and toxicity
• Drug resistance
• Adherence
• Risk compensation
• Access
• Cost
9
10
What’s being researched?
Large studies
• Viread or Truvada pill taken daily
• Viread tenofovir
• Truvada tenofovir + emtricitabine
• Tenofovir vaginal gel used before/after sex or daily
Small Studies
• Gels used rectally
• Pills used intermittently or before/after sex
• Slow-release intravaginal rings
• Long-lasting injections
• Antiretrovirals other than tenofovir and emtricitabine
10
How is the research conducted?
• Biomedical prevention trials
• Enrollment criteria
• Randomized
• Placebo-controlled
• Blinded
11
How is the research conducted?
• Biomedical prevention trials
• Enrollment criteria
• Randomized
• Placebo-controlled
• Blinded
• Comprehensive package of prevention services
•
•
•
•
•
Risk-reduction counseling
Access to male and female condoms
Adherence counseling
HIV testing
STI diagnosis and treatment
12
How is the research conducted?
• Biomedical prevention trials
• Enrollment criteria
• Randomized
• Placebo-controlled
• Blinded
• Comprehensive package of prevention services
• Several outcomes measured
•
•
•
•
HIV infections
Adherence
Side-effects and toxicity
Risk behavior
13
Limitations of biomedical prevention trials
• Ethical issues
• Measuring adherence
• Generalizability to other populations
• Applicability to the “real world”
14
What does the research say about PrEP?
Study participants
PrEP strategy
Reduced risk of
HIV infection
Overall
Consistent users
Safety concerns
15
What does the research say about PrEP?
CAPRISA 004
Study participants
Heterosexual
women
Type of PrEP
Coital tenofovir gel
(vaginal)
Reduced risk of
HIV infection
Overall
Consistent users
Safety concerns
39%
54%
• Diarrhea
16
What does the research say about PrEP?
CAPRISA 004
iPrEx
Study participants
Heterosexual women
Men who have sex
with men (MSM)
and trans women
Type of PrEP
Coital tenofovir gel
(vaginal)
Daily Truvada pill
39%
44%
54%
73%
• Diarrhea
• Nausea
• Headache
• Decrease in
kidney function
and bone density
• Drug resistance
Reduced risk of
HIV infection
Overall
Consistent users
Safety concerns
17
What does the research say about PrEP?
CAPRISA 004
iPrEx
FEM-PrEP
Study participants
Heterosexual
women
Men who have
sex with men
(MSM) and trans
women
Heterosexual
women
Type of PrEP
Coital tenofovir gel
(vaginal)
Daily Truvada pill
Daily Truvada pill
39%
44%
0%
54%
73%
-
• Diarrhea
• Nausea
• Headache
• Decrease in
kidney function
and bone density
• Drug resistance
• No major safety
concerns
Reduced risk of
HIV infection
Overall
Consistent users
Safety concerns
18
What does the research say about PrEP?
CAPRISA 004
iPrEx
FEM-PrEP
TDF2
Study participants
Heterosexual
women
Men who have
sex with men
(MSM) and trans
women
Heterosexual
women
Heterosexual
men and women
Type of PrEP
Coital tenofovir
gel (vaginal)
Daily Truvada pill
Daily Truvada
pill
Daily Truvada pill
39%
44%
0%
63%
54%
73%
-
78%
• Diarrhea
• Nausea
• Headache
• Decrease in
kidney function
and bone density
• Drug resistance
• No major
safety concerns
• Nausea
• Vomiting
• Dizziness
Reduced risk of
HIV infection
Overall
Consistent users
Safety concerns
19
What does the research say about PrEP?
CAPRISA 004
iPrEx
FEM-PrEP
TDF2
Partners PrEP
Heterosexual
women
Men who have
sex with men
(MSM) and trans
women
Heterosexual
women
Heterosexual men
and women
Serodiscordant
heterosexual
couples
Coital tenofovir
gel (vaginal)
Daily Truvada pill
Daily Truvada pill
Daily Truvada pill
Daily Viread pill
Daily Truvada
pill
39%
44%
0%
63%
62% (Viread)
73% (Truvada)
54%
73%
-
78%
-
• Diarrhea
• Nausea
• Headache
• Decrease in
kidney function
and bone density
• Drug resistance
• No major safety
concerns
• Nausea
• Vomiting
• Dizziness
• Nausea
• Diarrhea
20
What do we know about PrEP?
•
In combination with a comprehensive package of
prevention services…
1. Daily Truvada reduced the risk of infection when used by
• MSM and trans women
• Heterosexual men and women
2. Daily Viread reduced the risk of infection when used by
heterosexual men and women
3. A vaginal tenofovir gel used before and after sex reduced the
risk of infection when used by women.
•
It needs to be used consistently for it to work.
•
The risk of side effects, toxicity, and drug resistance are
low.
21
What don’t we know about PrEP?
• Safety/effectiveness of…
• A pill taken occasionally
• A gel used in the rectum
• Long-lasting options (intravaginal ring or injection)
• Other antiretrovirals
• Safety/effectiveness of Viread, Truvada and tenofovir gel…
• In populations not included in trials
• Over a longer period of time
• In the “real world”
22
What’s next for oral and topical PrEP?
1. Ongoing research
23
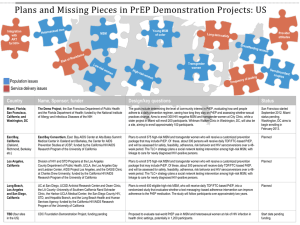
Ongoing PrEP research
Study
Location
Population
Intervention
Completion
CDC 4370
Thailand
2,400 people who
use injection
drugs
• Daily Viread pill
2012
VOICE
East/South
Africa
5,000 heterosexual
women
• Daily Viread pill
• Daily Truvada pill
• Daily tenofovir gel
2013
Go to www.avac.org for latest trial information
24
What’s next for oral and topical PrEP?
1. Ongoing research
2. Regulatory Approval
•
•
•
Health Canada
Safety and effectiveness data
Off-label prescriptions
25
What’s next for oral and topical PrEP?
1. Ongoing research
2. Regulatory Approval
3. Roll out
•
Impact outside of a clinical trial
26
Impact outside of a clinical trial
1. Uptake
• How many people are using it?
•
•
•
•
Awareness – Do people know its available?
Acceptability – Do people want to use it?
Access – Can people access it if they want to?
Who is using it?
2. Adherence
• Are people using it consistently and correctly?
3. Risk behavior
• Are people increasing their risk behavior?
27
What’s next for oral and topical PrEP?
1. Ongoing research
2. Regulatory Approval
3. Roll out
•
•
Impact outside of a clinical trial
Comprehensive approach
28
Integrating PrEP into a comprehensive approach
• Clinical services
• Non-clinical services
29
Integrating PrEP into a comprehensive approach
• Clinical services
• Eligibility assessment and prescription
• HIV testing
• Drug resistance testing
• Medical and clinical monitoring
• STI treatment and diagnosis
• Non-clinical services
30
Integrating PrEP into a comprehensive approach
• Clinical services
• Eligibility assessment and prescription
• HIV testing
• Drug resistance testing
• Medical and clinical monitoring
• STI treatment and diagnosis
• Non-clinical services
• Outreach and education
• Risk-reduction counseling
• Adherence support
• Advocacy
31
What’s next for oral and topical PrEP?
1. Ongoing research
2. Regulatory Approval
3. Roll out
•
•
•
Impact outside of a clinical trial
Comprehensive approach
Feasibility
•
•
Open-label studies
Demonstration projects
32
CDC PrEP Guidelines
•
In 2011, the CDC released interim guidance for
healthcare providers on the prescription of PrEP
•
“PrEP has the potential to contribute to effective
and safe HIV prevention for MSM if
1. Targeted to MSM at high risk for infection
2. Delivered as part of a comprehensive set of prevention
services (risk-reduction and adherence counseling,
condom access, diagnosis and treatment of STIs)
3. Accompanied by monitoring of HIV status, side-effects,
adherence, and risk behaviors at regular intervals”
33
34
CDC PrEP Guidelines
• Why were these guidelines released before regulatory
approval?
• “Concerns exist that without early guidance, various
unsafe and potentially less effective PrEP-related
practises could develop”
• Such as…
•
•
•
•
Use of other antiretrovirals
Use of other dosing schedules
Not screening for HIV status before initiating PrEP
Providing in absence of other HIV prevention services
35
Does PrEP have a role to play in Canada?
36
37
38
CATIE Resources
39
Thank you!
40