MODY 3 - Yorkshire and the Humber Deanery
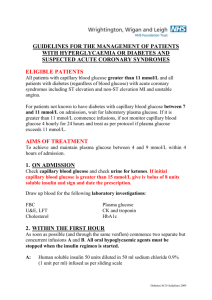
advertisement

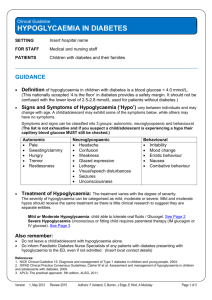
Michael Mansfield Diabetes Consultant Leeds Teaching Hospitals New units for HbA1c Diabetes is relevant to in-patient care NHS diabetes resource Gliptins & GLP-1 analogs & SGLT-2 inhibitors End of life Sodium type 1 diabetes type 2 diabetes gestational diabetes diabetes secondary to pancreatic disease unknown / unclear genetic diabetes other MODY 3 Mutations of the hepatocyte nuclear factor 1α gene Disordered insulin release Autosomal dominant pedigree over 2, ideally 3 generations Age of onset < 25 years in at least one family member No need for insulin (or detectable C-peptide) in first 2-5 years after diagnosis Progressive rise in glucose levels through life Low renal threshold for glucose Often very sensitive to sulphonylurea therapy Permanent neonatal diabetes mellitus Activating mutations of the KCNJ11 gene, which codes for the Kir6.2 subunit of the beta cell K-ATP channel. Congenital impairment of insulin release Mostly new mutations Onset in first 3 (- 6) months of life but no immune markers of type 1 diabetes Often responds well to sulphonylurea therapy New units for glycated haemoglobin DCCT HbA1c IFCC HbA1c % mmol/mol 6.0 42 6.5 48 7.0 53 7.5 59 8.0 64 9.0 75 Umpierrez et al JCEM 2002, Memphis, Tennessee and Atlanta Georgia Baker et al Thorax 2006 St George’s Hospital London The Think Glucose programme provides a package of tried and tested products, learning and support to improve awareness and remove the obstacles to the treatment of patients with diabetes as a secondary diagnosis. Implementing a clinical pathway will improve the patient experience and the quality of their care. Training of staff Links to and alerting of diabetes team New and NHS-wide documentation Importance of careful medicines reconciliation IV insulin infusion safety cannula IV fluid Insulin storage and insulin syringes National or local guidelines for: DKA, HHS hypoglycaemia surgery, endoscopy hyperkalaemia end of life tube feeding labour steroids for fetal lung maturation Capillary glucose monitoring and recording Patient self-management/admin of insulin “Sliding scales” and other insulin prescribing www.diabetes.nhs.uk withdrawn (USA) withdrawn withdrawn SGLT-2 inhibitors oral 2012 The incretin effect oral glucose IV glucose oral glucose IV glucose Satiety effect reduced food intake Increased glucose uptake & glycogenesis Slowed gastric emptying Increased insulin release Reduced glucagon release Site of GLP-1 synthesis Secretion increased after meals Overview of GLP-1 physiology DPP4 inhibitors NICE 2009 The problem with….. Metformin is bowel side effects, risk of lactic acidosis when eGFR decreased Sulphonylureas weight gain and risk of hypoglycaemia Insulin is weight gain, risk of hypoglycaemia, some driving restrictions injections Glitazones take weeks to start working, expensive, very marked weight gain, fluid retention and heart failure, distal bone fracture risk Gliptins (DPP4 inhibitors) expensive, no long-term safety record weak pancreatitis signal Exenatide expensive, nausea and vomiting in first months injected, no long-term safety record, pancreatitis signal Liraglutide even more expensive, nausea and vomiting in first months injected, no long-term safety record pancreatitis signal, v weak thyroid malignancy signal Dapaglifozin expensive, genital thrush, no long-term safety record glucose control in diabetes at the end of life altered nutrition negative energy balance weight reduction reduction in physical activity systemic humoral stress response pancreatic destruction renal impairment liver destruction loss of fat and muscle steroids psychological stress mental illness July 2012 Key principles Aims for glucose levels: 1. No glucose level less than 6 mmol/L 2. No glucose level higher than about 15 mmol/L Breaks down care in to 4 scenarios: 1. End of life but prognosis of more than 1 year 2. Prognosis in months 3. Prognosis in weeks 4. Prognosis in days A few words on hyponatraemia Always check for hyperglycaemia: For every 3.5 mmol/L the glucose is high, sodium falls by 1 mmol/L It’s all about the brain Always look for timescale of sodium fall Brain tolerates slow changes (up or down) remarkably well SIADH is not the only cause, dehydration is common too Assessment of patient’s circulating volume status is key A cause for appropriate ADH release/activity excludes SIADH If patient has been on steroids then suppressed HPA axis possible Low circulating volume (NB intact thirst) acute medical emergency including sepsis surgical abdomen hypoadrenalism (Addisons or suppressed HPA axis) diuretics ascites nephrosis congestive cardiac failure Normal or increased circulating volume syndromes of inappropriate ADH activity (secretion or receptor) sick cell syndrome Redistribution of body water hyperglycaemia Management Usually not urgent unless the cause itself is emergency Treatment obviously depends on the cause In practice it often seems to self correct May need treatment anyway if brain function impaired by sudden and/or severe fall: ie neurological signs / seizures / reduced GCS IV saline and in some exceptional circumstances hypertonic saline appropriate. Aim for slow improvement in Na 5mmol/L in 12 hours. Not much improvement needed to reverse brain dysfunction Read this article: Adrogue 2000 NEJM 342: 1851