Cysts
advertisement

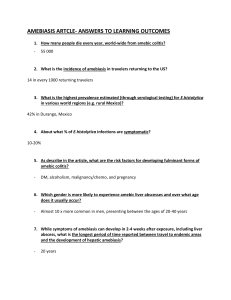
Entamoeba histolytica & Giardia lambila Entamoeba histolytica: a protozoan parasite, cause amebiasis 50000000 people worldwide suffer from E. histolytica infection amebic dysentery and amebic liver abscess kill at least 40000110000 individuals yearly the second leading cause of death among parasitic diseases Giardia lambila: a major cause of diarrheal outbreaks from contaminated water supplies resides small intestine ( duodenum), gallbladder, causing giardiasis or ‘‘traveler’s diarrhea’’ common in children with younger age, with a high incidence among tourists & homosexual male, opportunistic protozoa (parasite) Case study I A 36 year old man presented to the emergency department of a general hospital with 10 day history of intermittent diarrhea and tenesmus, with blood and mucus visible in the stool. He had just returned from a working trip to India, where he had visited a rural town in the last week of his trip. Physical Examination: VS: T 38.8 C, P96/min, R 16/min, BP 130/80 mmHg PE: Ill- appearing male in mild distress; abdominal exam revealed mild diffuse tenderness, and rectal exam was positive for blood Laboratory studies WBC: 11600/l Differential: 72% PMNs 20% lymph Imaging Sigmoidoscopic examination revealed multiple small hemorrhagic areas with ulcers Microscopic exam as following Case study II A 25 year old man presented to a hospital clinic with a 2 week history of sustained diarrhea (three to five bowel movement per day), nausea, flatulence, and lack of appetite. He described his diarrhea as initially watery, and then greasy and foul smelling. He added that he had a bloating sensation. He did not have fever or chills. The patient had been in good health. Four weeks previous to seeing his physician, he had visited a rural town for several days. Physical Examination: VS: T 37C, P82/min, R 14min, BP 134/80 mmHg PE: abdomen was distened and mildly tender, no hepatosplenomegaly. Rectal exam was normal. Laboratory studies: WBC: 6300/l Differential: normal Serum chemistries: BUN 22 mg/dl creatinine 1.2 mg/dl Microscopic exam and duodenal aspirate exam as following Brain abscess Lung abscess Live abscess Large intestine ulcers Lung abscess Inhabits in large intestine metastasis trophozites Cysts or Quadrinucleate Cysts trophozites cyst trophozites Pathogenesis & Symptoms Pathogenesis ingestion of the quadrinucleate cyst of E. histolytica from fecally contaminated food or water initiates infection infection also occurs through direct person-to- person contact inhabits the large intestine, invade the mucosal crypts, feed RBCs & form ulcers Pathogenic factors: Lectin adherence to host cells, in signal, cell killing amoebapores form pores in host cell membranes phagocytosis cysteine proteinases: cytopathic for host tissue … invasion 1. Adherence Ameba 4. Phagocytosis and Invasion 2. Lectin Signal 3. Cell killing amoebic invasion through the mucosa and into the submucosal tissues is the hallmark of amoebic colitis the lateral extension through the submucosal tissues gives rise to the classic flask-shaped ulcer of amoebiasis or ameboma amebic liver abscess is the most common manifestation of extrainintestinal disease the most serious complication of amoebic liver abscess are rupture Symptoms asymptomatic/Carrier state: the amoebae may reproduce but the patient shows no clinical symptoms symptomatic intestinal amebiasis: may complain of more specific symptoms, including diarrhea, abdominal pain and chronic weight loss symptomatic extraintestinal amebiasis: the formation of an abscess in the right lobe of the liver , trophozoites extension through the diaphragm, causing amebic pneumonitis (abscess) brain abscess Diagnosis Microscopic examination a direct saline wet mount------trophozoites, cyst from pus------ trophozoites only iodine stain------------------------cyst concentration techniques permanent stained E.histolytica size Trophozoite pseudopodium movement inclusion karyosome Cyst size No. of nuclei chromatoid E. coli 10-40 m more transparent active RBC centrol, small 20-50 m less transparent sluggish no RBC asymmetrical 12-20 m 1-4 rounded ends 15-25m 1-8 splintered ends Immunologic techniques monoclonal antibody detected antigen from stool or pus detected specific antibodies by antigen ELISA, IFA, IHA PCR techniques 16S rRNA, Prx gene … differentiation of E.histolytica from the commensals E. dispar is not possible by morphology but requires the use of speciesspecific Mab or PCR techniques Imaging colonoscopy, Sigmoidoscopic examination -----biopsy sonography, computed tomography (CT), magnetic resonance imaging (MRI) Epidemiology generally higher in the tropics, subtropics, and poor sanitation, poor nutrition (for example) a high-carbohydrate diet, alcoholism, genetic makeup, bacteria infection of the intestine, local injury to the colonic mucosa the true prevalence of E. histolytica is perhaps closer to 1% to 5% worldwide the realisation that E. histolytica & E.dispar are morphologically identical species with remarkable different physiological and pathogical characteristics has impacted on all aspects but notably on the epidemiology no sexual preference for intestinal amoebiasis, but amebic liver abscess is 3 to 10 times more common in men the high-risk group for amebiasis include travelers, institutionalized mental patients, promiscuous homonsexual a severe form of infection in neonates, pregnant women, women in the postpartum period, immunocompromised patients, patients with malnutrition or malignancy ingestion of the infective cyst, through hand – mouth contamination & food /water contamination flies & cockroaches may also serve as vectors of E. histolytica Treatment & Prevention Whenever possible, a laboratory diagnosis of E.histolytica infection, unless confirmed by visualization of ingested RBCs in the trophozoite, should be substantiated by (1) presence of RBCs in stool (2) serum antibody titer (3) stool E.histolytica antigen titer Infection Asymptomatic intestinal amoebiasis Drug and Dosage paromomycin 25-30mg/kg/D in 3 divided does for 7 days metronidazole 750 mg 3 time daily for 10 days Amebic dysentery and liver abscess metronidazole 750 mg 3 time daily Ameboma for 10 days follow by paromomycin Metronidazole and tinidazole are first-line agents in the treatment of acute amebic colitis and amebic liver abscess therapeutic aspiration of an amebic liver abscess is occasionally required as an adjunct to antiparasitic therapy the prevention of amebic infection starts with avoidance of fecally contaminated food and water. The high incidence of amebiasis in recent community-based studies suggests that an effective vaccine would improve public health. Free-living amoebae --- Naegleria, Acanthamoeba, Balamuthia Naegleria Human beings usually acquire Naegleria infection from swimming in the contaminated water or contaminated pipeline Naegleria fowleri caused primary amebic meningoencephalitis (PAM), an acute, suppurative infection of the brain and meninges. Acanthamoeba, Balamuthia Acanthamoeba species cause granulomatous amebic encephalitis (GAE), amebic keratitis, corneal ulceration, amebic dermatitis Balamuthia infection have cutaneous lesions and GAE a wet mount of cerebrospinal fluid (CSF) is usually more useful detection of motile organisms is a diagnostic finding, but they must distinguished from motile leukocytes to detected of parasites a culture is in order DNA-based or Mab-based technique may also help for difference diagnosis the drug of choice for the treatment of PAM is amphotericin B the treatment of GAE has not been standardized the treatment of AK includes systemic antifungal drugs, tropical antiamebic eye drops, and surgical debridement of the ocular lesions Giardia lamblia Trophozoites of Giardia are fund in the upper part of the small intestine ( duodenum), gallbladder, causing giardiasis or ‘tourist diarrhea Giardia is worldwide in distribution Giardia lamblia is considered to be one of the major cause of parasitic diarrhea Human infection mainly results from ingestion mature cystcontaminated food or water excystation occurs in the upper regions of the small intestine, where the trophozoite resides & multiplies by binary fission trophozoites pass through the digestive tract, encyst in the colon & transformed into cysts, pass in the feces cysts with highly resistant Infections with G. lamblia are often completely asymptomatic Extensive ulceration of mucosa may occur in heavy infection symptomatic infection may cause intestinal disorders, most commonly diarrhea------Vit A & soluble fat, nausea, flatulence, weight loss a direct saline wet mount------trophozoites, cyst iodine stain------------------------cyst concentration techniques duodenal aspiration entero test -----an alternative & more satisfactory technique for trophozoites detection Imaging DNA-based or Mab-based technique may also help for difference diagnosis common in children 6-10 years of age, with a high incidence among tourists & homosexual male, opportunistic protozoa (parasite) Metronidazole is most common drug in treatment (Tinidazole Paromomycin)