IRmer take 2! - Nightingale Centre Training
advertisement
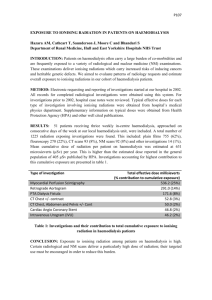
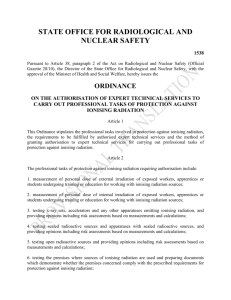
IRMER , WHY? Amanda Bath Advance Practitioner RPS May 2014 RPS- Radiation Protection Supervisor RPA- Radiation Protection Advisor CMPE- Christies Medical Physics and Engineering Topics •Ionising radiation and effects. •Risks •Legislation •How does it effect our practice Sources of Ionising Radiation UK Medical 15% Effects of Ionising Radiation somatic effects stochastic deterministic Stochastic Effects • Stochastic effects are ones where the chance of the effect happening increases with radiation dose. • There is no threshold dose at which they will definitely occur. Deterministic Effects • These occur when high radiation doses are received. This damage is a consequence of cell death and the effects can show immediately or after several cell divisions. The damage can be directly linked to that exposure. • There is a threshold below which no deterministic effects occur. Risks • • • • • • Annual Risk of death: Smoking 10 cigarettes a day – 1 in 200 Road accident – 1 in 5,000 Natural radiation – 1 in 9,000 Accidents at work – 1 in 20,000 Medical radiation – 1 in 53,000 Legislation The United Nations • • • • 1953 Dwight D.Eisenhower “Chance for Peace”. IAEA- International Atomic Energy Agency WHO- World Health Organisation. UNSCEAR- United Nations Scientific Committee on the Effects of Atomic Radiation. International Commission for Radiological Protection (ICRP) Independent advisory body founded in 1928 , registered charity. Three fundamental principles of radiation protection Justification Optimisation Dose limits European Union/Commission • • • • European Atomic Energy Community (EURATOM) Peaceful use of Nuclear Energy . Protection of patients exposed in medical practice Issued directives that led to IR99 and IRMER. UK Legislation The Health and Safety Executive (HSE)Work with Ionising Radiation , which includes: • The Ionising Radiations Regulations 1999 (IRR99) • An approved Code of Practice • Guidance notes IRR99 is UK law and is enforced by the HSE. IRR99 The employer has the responsibility for complying with the regulations but will not be able to fully discharge his responsibility without the cooperation of his employees. IRR99 As Low As Reasonably Practicable ALARP “Every radiation employer shall…take all necessary steps to restrict as far as reasonably practicable the extent to which his employees or other persons are exposed to ionising radiation.” IRR99- Requirements • • • • Appropriate training Register of staff “engaged “ in work. Staff uniquely identified . Training dates and refresher dates recorded. The Ionising Radiation (Medical Exposure) Regulations 2000 IR(ME)R Employers are required to provide written procedures and protocols to cover medical exposures for which they are responsible. IR(ME)R 2000 is UK law and is currently enforced by the Care Quality Commission.(CQC) IR(ME)R 4 duty holders in the administering of ionising radiation • Employer-radiological installation and risk assessments. (advice from RPA) • Referrer- registered medical practitioner/health professional. • Practitioner- registered medical practitioner/health professional. Justifies the exposure. • Operator- person who carries out the exposure. No role is specific to any profession IR(ME)R- Operators An operator is any person who is entitled, in accordance with the Employer’s procedures, to carry out practical aspects of the exposure allocated to them by the employer or practitioner. This includes identification of the patient! IR(ME)R-Requirements • Adequate training. • Continuing education and training with up to date records/register. • Assistant practitioners- work-based training , e-learning , within scope of qualification you have completed. • Competence matrix- individual training profiles. How does this effect our practice? How practice changes. Incidents1. Paper to electronic systems. 2. Film screen to full field digital mammography. 1.Electronic Requesting • No mammograms repeated within 6 months of previous mammogram. (exceptional circumstances). • Previous paperwork not available, no method of recording information. • Client had a mammogram 2 months earlier. Outcome • • • • New protocol in place. Check on PACS system for previous imaging Record on ‘Q’ page of RIS system. Result- fewer incidents. 2.FFD Mammography • Flat field test • The parameters are set automatically ie. large focal spot, Mo/Mo, 26kV and 200 mAs. • Ensure that the operating parameters are returned to Standard and Auto 2.FFD Mammography Outcome • New protocol in place. • Sign to say have returned to “auto” and “auto”. • All staff informed of incidents. • Not happened since. Regulatory Changes • • • • 2007 EU process of revision Influenced by IRCP and IAEA recommendations. The Department of Energy and Climate Change. Audit- Identification and justification. Audit • Audited the ‘Q’ page. • April 2013- 179 out of 196, (91%) of examinations were justified, from a target of 100%. • Dec 2013-199 out of 200 examinations (99.5%) were justified and had the operator recorded. Summary • • • • Legislation is LAW. Necessary to keep up to date with training. Recording of evidence. Resources. www.e-lfh.org.uk References • www.hse.gov.uk/radiation/ionising • www.christie.nhs.uk/the-foundation-trust/treatments-andclinical-services/christie-medical-physics-and-engineering(cmpe).aspx • www.e-lfh.org.uk • Amanda.bath@uhsm.nhs.uk