The role of the pharmacist in delivering thromboprophylaxis
advertisement

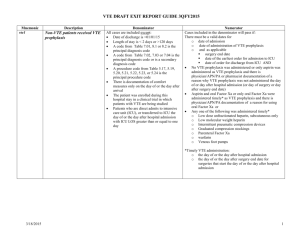
The role of the pharmacist in delivering thromboprophylaxis Robin Offord Director of Clinical Pharmacy UCL Hospitals NHS Foundation Trust robin.offord@uclh.nhs.uk The Pharmacy Department Medicines Information Medication Safety Production & Manufacturing Clinical Clinical Pharmacy Pharmacy Quality Assurance Formulary & Medicines Management Procurement Dispensing & Distribution Clinical Pharmacists – Back Office Functions Clinical Governance & Risk Management Financial Governance & Risk Management Education & Development Management & Leadership Medicines Management (Multiprofessional) Guidelines, Policies, & Protocols Expenditure Reports & Analysis Under- & PostGraduate Teaching Strategic Vision & Direction Formulary Evaluation & Audit Commissioning Competence Assessment & Peer Review HR, Employee Relations, & Recruitment Safe & Secure Handling Research & Research Support QIPP eLearning Project Management Quality Assurance EQUIP study • 19 acute hospital trusts in North-west England • 11,077 errors were detected in 124,260 medication orders – Drug charts checked on seven consecutive ‘census days’ • 8.9 errors for every 100 prescriptions ordered Recommendations Re-evaluate • • • • • Clinical working environments Undergraduate medical education programmes Foundation Year 1 education Other parts of the medical education continuum Interprofessional education Dornan T, et al. http://www.gmc-uk.org/about/research/research_commissioned.asp UCLH study in acute medical admissions Methodology notes • Errors identified by prescribing doctor, pharmacist or auditor • Graded as per EQUIP study by independent doctor and pharmacist • Excluded iv fluids, stat and VTE prophylaxis sections of the chart Results • 121 errors identified in 1,067 medication orders audited (11.3%) – EQUIP study reported an error rate of 13.4% for new admissions • 3% of errors recognised by doctor • 63% by pharmacist • 34% by auditor Clinical Pharmacists – Care bundle approach Medicines are accurately transcribed on admission and discharge Medicines Reconciliation Patients are satisfied with information about their medicines Medicines are safe and effective Medication Review Timely Supply Patients receive the correct medicines in a timely manner Provision of Patient Information Safe Discharge Duncan McRobbie Guy’s & St Thomas’ Hospitals NHS Foundation Trust Additional benefits • Depth and breadth of service provision – Generally, all inpatients are seen every day – Increasing levels of service to Pre-Admission Clinics • Strong working relationships – Accepted role in influencing and leading on prescribing decisions • Continuity – High levels of turnover • Impact of European Working Time Directive – Shift working • Short junior doctor rotations • Prescribing functions VTE CQUIN Actions Clinical Governance & Risk Management Financial Governance & Risk Management Education & Development Management & Leadership Medicines Management (Multiprofessional) Guidelines, Policies, & Protocols Expenditure Reports & Analysis Under- & PostGraduate Teaching Strategic Vision & Direction Formulary Evaluation & Audit Commissioning Competence Assessment & Peer Review HR, Employee Relations, & Recruitment Safe & Secure Handling Research & Research Support QIPP eLearning Project Management Quality Assurance VTE CQUIN Actions VTE Risk Assessment & Appropriate Action Medicines are accurately transcribed on admission and discharge Medicines Reconciliation Patients are satisfied with information about their medicines Medicines are safe and effective Medication Review Timely Supply Provision of Patient Information Patients receive the correct medicine in a timely manner Safe Discharge Pharmacy – CQUIN implementation in 2011-12 VTE Risk Assessment & Appropriate Action Thrombosis Committees - Evidence-based guidance covering all clinical specialities - Trust-wide awareness and education programme - Regular audits of progress - Electronic solutions for data capture Guidance Comprehensive clinical guidelines Online training and assessment tools Implementation Modified drug charts to aid appropriate prescribing Evaluation Audits by ward pharmacists at appropriate frequencies Performance reported via quality scorecards Future development Incorporate appropriate rules into ePrescribing solutions The Pharmacy Profession • Separation of regulatory and leadership functions in 2010: Multidisciplinary, multiprofessional approach • Shared core values – Make the patient the focus of everything that we do – Support our staff to deliver the best care that they can – Ensure best value in health care • Collaboration – Yields benefits greater than the sum of the individual contributions VTE Three Professions Group National VTE Prevention Programme SENIOR RESPONSIBLE OWNER (SRO) Sir Bruce Keogh NHS MD VTE BOARD (~15 people) Dr Anita Thomas OBE (Chair) NCD for VTE CLINICAL ADVISORY GROUP (~25 people) Dr Anita Thomas OBE (Chair) DH INTERNAL STAKEHOLDER GROUP Tim Brown VTE PREVENTION TEAM Margaret Candeland (0.3 WTE) Workstreams Patient Awareness & Experience Beverly Hunt Sally Brearley Professional Leadership AoMRC External Reference Groups VTE THREE PROFESSIONS GROUP Rotating Chair: AoMRC; RCN; RPS PREVENTION AND PH [QIPP / CQUIN] Measurement & Evaluation Anita Thomas Tim Brown Information & Audit Anita Thomas Tim Brown Communications Michael Carden Janine Ford VTE Prevention Action Plan • Royal Pharmaceutical Society working with UK Clinical Pharmacists Association HAT Group • Liaison with other professions to align actions • Announcement at VTE Prevention Leadership Summit – 30 March 2011 – Sir Bruce Keogh - NHS Medical Director – Andrew Gwynne MP - APPTG Chair – Rt Hon Andrew Lansley CBE MP - Secretary of State for Health